Research Article - (2024) Volume 12, Issue 8
Case Report of Asymptomatic Leukoplakia in an Edentulous Patient: A Diagnostic Approach
*Correspondence: Eman Alsheikh, Department of Oral Medicine, MSc Cairo University, Sudan, Email:
Abstract
Introduction: Oral Leukoplakia (ol) is a Potentially Malignant Oral Disorder (pmod) that can transform into Oral Squamous Cell Carcinoma (oscc). Defined as "a white plaque of questionable risk," ol necessitates the exclusion of other known diseases or disorders that do not carry an increased cancer risk. Case presentation: A 65-year-old female, i'tidal hussein mohammed, presented to the diagnostic clinic at cairo university in 2017, seeking denture fabrication after being edentulous for five years. An intraoral examination revealed a non-symptomatic white lesion on the left lower ridge, raising suspicion for leukoplakia. Conclusion: Regular dental check-ups and thorough examinations are crucial, particularly in asymptomatic edentulous patients. Early diagnosis, monitoring, and patient education on routine dental visits can significantly mitigate the risk of malignant transformation in potentially malignant lesions.
Keywords
oral leukoplakia, toluidine blue test, potentially malignant lesions
Introduction
Oral Leukoplakia (OL) is a Potentially Malignant Oral Disorder (PMOD) that sometimes transforms into Oral Squamous Cell Carcinoma (OSCC). OL, which is defined as “a white plaque of questionable risk, (other) known diseases or disorders that carry no increased risk of cancers having been excluded” [1].
Epidemiology
OL is recognized as the most prevalent potentially malignant disorder affecting the oral cavity, observed in around 2%-3% of the global population. It is more commonly diagnosed in individuals over 40 years of age. The likelihood of malignant transformation in leukoplakia varies, with studies indicating a range from 1% to 40%, averaging about 13%. Although surgery is considered the main treatment, particularly for cases of isolated leukoplakia or proliferative verrucous leukoplakia where complete removal of the lesion is recommended, approximately 80% of these cases may undergo excessive surgical treatment, leading to unnecessary procedures [2].
Aetiology
Oral leukoplakia (OL) is influenced by several risk factors, though its exact cause remains uncertain. Smoking is the primary risk factor, with smokers being six times more likely to develop OL. Alcohol, while recognized as a contributing factor, plays a less defined role in OL compared to oral squamous cell carcinoma (OSCC). OL can also occur in individuals who do not smoke or consume alcohol, suggesting the involvement of genetic predisposition. In Southeast Asia, the use of betel quid significantly contributes to the higher prevalence of OL. The pathogenesis of OL is unclear, but it has been linked to several predisposing factors, such as tobacco and alcohol use. There is also some evidence connecting OL with HPV infection in the oral epithelium. Additionally, genetic changes in genes responsible for genomic stability, cell cycle regulation, cytoskeleton integrity, angiogenesis, and apoptosis may contribute to the development of OL and its progression to malignancy. [3].
Clinical Presentation
Oral leukoplakia can affect any part of the oral mucosa, either as solitary or multiple white patches. The sites most affected include the lateral and ventral tongue, buccal mucosa, and floor of the mouth, the latter site being frequently affected in populations with a high prevalence of smoking [4]. Oral leukoplakia may be subclassified into homogeneous and non-homogeneous forms. Homogenous oral leukoplakia is characterized by a predominantly flat, uniform, often well-demarcated white patch, with a consistent surface topography, and it usually lacks symptoms. When homogenous oral leukoplakia is found on the floor of the mouth, it can have a distinctive ebbing tide appearance [4]. The non-homogeneous form is any white patch that deviates from the above. Non-homogenous oral leukoplakia should be regarded with significant suspicion as it carries a higher risk of malignant transformation than homogenous oral leukoplakia. There are several diverse clinical presentations including erythroleukoplakia, which is defined as a mixed white and red patch but retaining a predominantly white color. Non-homogenous OL may show focal superficial ulceration, and the margins can be more diffused. Non-homogenous OL with red or ulcerated areas can be symptomatic. Finally, Proliferative Verrucous Leukoplakia (PVL) is a rare form of oral leukoplakia, characterized by an exophytic, wrinkled, corrugated surface. PVL commonly affects the gingivae, is often multifocal, and is most commonly found in elderly females [5].
Diagnostic Procedures
Based on the present definition, a diagnosis of leukoplakia is one by exclusion of known, well-defined lesions and disorders that may occur in the oral mucosa, as being listed in (Table 1) [6]. As a result of the WHO definition of oral leukoplakia, the accuracy of the clinical diagnosis largely depends on the experience of the clinician. Depending on the clinical presentation and in the absence of symptoms, it may then be justified to render a diagnosis of oral leukoplakia without taking a biopsy. Less-experienced clinicians are advised to refer the patient either to a more experienced clinician or to take a biopsy in order to rule out any known, well-defined disease and also to report the possible presence and degree of epithelial dysplasia or even carcinoma (in situ). It should be recognized that in large or multiple OL an incisional biopsy may not be representative for the entire lesion [7]. Furthermore, even in biopsied whitish lesions, the final diagnosis of oral leukoplakia may remain questionable, for instance in some cases of lichen planus. At present, there are no molecular markers or sets of markers that would more accurately result in a proper diagnosis of oral leukoplakia [8].
| LESION OR DISEASE | MAIN DIAGNOSTIC CRITERIA |
|---|---|
| Aspirin burn (including other types of chemical burns) | History of prolonged application of aspirin tablets or other chemical agents; the histopathology is not diagnostic. |
| Candidiasis and hyperplastic | Somewhat questionable entity; some refer to this lesion a candida-associated leukoplakia. |
| Hairy leukoplakia | Usually bilateral on the borders of the tongue; histopathology is important, including the immunohistochemical demonstration of the presence of EBV |
| Keratotic lesions (include reversed smoking keratosis, sublingual keratosis, alveolar ridge keratosis, frictional keratosis, sanguinaria-associated keratosis, and keratosis of unknown significance) | Different etiologies and various clinical presentations; in many cases the taking of a biopsy is indicated. Some of the keratotic lesions carry an increased risk of malignant transformation |
| Lesion caused by prolonged, direct contact of the oral mucosa with an amalgam restoration or other dental restorations; often listed as a lichenoid lesion | Disappearance of the lesion within an arbitrarily chosen period of 2–3 months after removal of the restoration; the taking of a pretreatment biopsy is recommended. |
| Lichen planus and lichenoid lesions/reactions, e.g., in cGVHD | Often a clinical diagnosis; the non-reticular types such as erosive and plaque types may occasionally be difficult to distinguish from leukoplakia even when biopsied. |
| Lichen sclerosis | The diagnosis should be supported by a biopsy |
| Lupus erythematosus | Often a clinical diagnosis; almost always cutaneous involvement as well. Histopathology and direct immunofluorescence may be helpful |
| Morsicatio | History of habitual chewing or biting. Clinical aspect of irregular whitish-yellowish flakes. Often bilateral |
| Papilloma and allied lesions, e.g., condyloma acuminatum, multifocal epithelial hyperplasia, squamous papilloma, and verruca vulgaris | Clinical aspect; medical history. A biopsy may be helpful including HPV typing. |
| Reversed smoking induced palatal lesion | May mimic leukoplakia or erythroplakia; carries a high risk of malignant transformation |
| Smoker’s palate (stomatitis nicotina) | Usually a clinical diagnosis. Rarely becomes malignant. Regresses after cessation of the smoking habit |
| Snuff dipper’s lesion | See keratotic lesions above (tobacco pouch keratosis) |
| Syphilis, secondary (mucous patches) | Medical history; clinical aspect. Demonstration of T. pallidum; serology. |
| White sponge nevus | Young age; often family history. The clinical aspect is more or less diagnostic. Occasionally a biopsy may be helpful. |
Table 1: Some known, well defined predominantly white lesions or diseases that should be excluded from leukoplakia
History and Clinical Assessment
Case Presentation
A 65-year-old female patient (born in 1952), named I'tidal Hussein Mohammed, presented to the Diagnostic Clinic at Cairo University in 2017. She had a significant past medical history of Hepatitis C infection, though she reported being medically fit at the time of the visit. The patient was edentulous and sought dental treatment for the fabrication of new dentures, as her previous teeth were extracted approximately five years ago. She had not previously sought dental assistance for this issue.
During the routine intraoral examination, a white lesion was noted on the left lower ridge, adjacent to the site of the second premolar (now missing). The patient reported no symptoms and had not noticed the lesion prior to the examination. She could not confirm whether the lesion had changed in size over time.
Examination
A thorough examination of the entire oral mucosa was performed. The white lesion was non-scrapable and approximately 1 cm in diameter, with irregular but well-defined borders. There were no signs of ulceration or discomfort upon palpation. Given the patient's history of tooth extraction and delayed presentation for dental care, the lesion raised suspicion of leukoplakia (Figure 1).
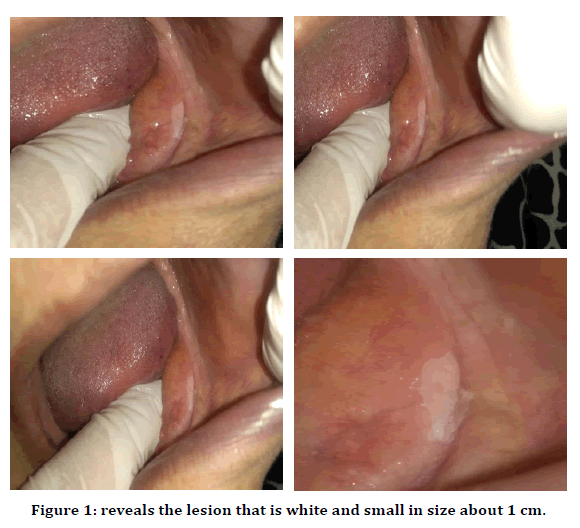
Figure 1. reveals the lesion that is white and small in size about 1 cm.
Diagnostic Tests
To further evaluate the lesion, a Toluidine Blue test was conducted. Toluidine Blue is a metachromatic dye that preferentially binds to nucleic acids, helping to identify areas of high cellular activity, which are potentially dysplastic or malignant. Positive staining in this case warranted a biopsy to rule out malignancy (Figure 2).
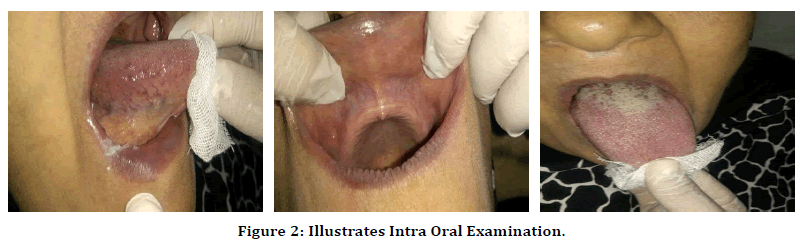
Figure 2. Illustrates Intra Oral Examination.
Diagnosis
The lesion was clinically diagnosed as leukoplakia, which was later confirmed through histopathological examination of the biopsy sample. Histopathology revealed hyperkeratosis with no evidence of dysplasia, classifying the lesion as non-dysplastic leukoplakia (Figure 3).
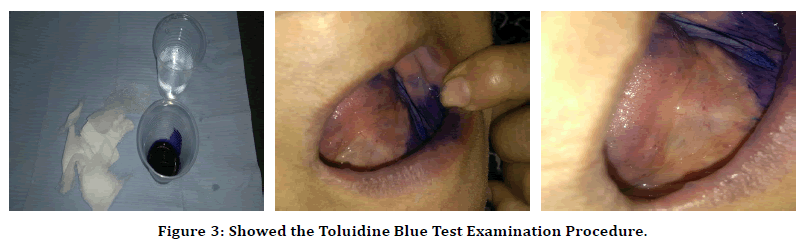
Figure 3. Showed the Toluidine Blue Test Examination Procedure.
Discussion
Leukoplakia is considered the most prevalent potentially malignant disorder of the oral cavity. This case highlights the importance of routine oral examinations, especially for asymptomatic lesions, which can be easily overlooked by patients. The presence of risk factors such as age, smoking history, and delayed dental care increases the need for early detection and intervention. While most cases of leukoplakia remain benign, the potential for malignant transformation makes it essential to utilize adjunct diagnostic tools, such as Toluidine Blue staining, and follow-up biopsies. Non-dysplastic leukoplakia, as seen in this patient, carries a lower malignant risk but still necessitates careful monitoring. The patient’s medical history, including past Hepatitis C infection, did not present an increased risk factor in this case, underscoring that leukoplakia can develop in patients without overt systemic contributors. This case illustrates how early diagnosis and appropriate follow-up can ensure better outcomes, particularly in preventing malignant transformation. Moreover, it emphasizes the need for patient education regarding the importance of regular dental visits, especially in edentulous patients, to identify potentially malignant lesions before symptoms arise.
Conclusion
This case report underscores the critical importance of regular dental check-ups and thorough intraoral examinations, particularly in asymptomatic edentulous patients. The identification of leukoplakia, even in the absence of symptoms, highlights the need for vigilant monitoring and timely intervention to mitigate the risk of malignant transformation. By employing adjunct diagnostic tools, such as Toluidine Blue staining, dental practitioners can enhance the accuracy of their assessments and ensure that potentially malignant lesions are appropriately addressed. The findings from this case emphasize the necessity of educating patients about the significance of routine dental visits, as early detection plays a pivotal role in preventing the progression of lesions to oral cancer. Regular follow-ups were recommended for the patient to monitor any changes in the leukoplakic lesion, reinforcing the idea that proactive management is essential in safeguarding oral health. This case not only illustrates the clinical approach to diagnosing asymptomatic leukoplakia but also serves as a reminder of the broader implications of preventive dental care in the early identification of oral diseases.
References
- Warnakulasuriya S, Johnson NW, Van der Waal I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. J Oral Pathol Med. 2007; 36:575-80.
- Aguirre‐Urizar JM, Lafuente‐Ibáñez de Mendoza I, Warnakulasuriya S. Malignant transformation of oral leukoplakia: systematic review and meta‐analysis of the last 5 years. Oral Dis. 2021; 27:1881-95.
- Sundberg J, Korytowska M, Holmberg E, et al. Recurrence rates after surgical removal of oral leukoplakia—a prospective longitudinal multi-centre study. PLoS One. 2019; 14:e0225682.
- Warnakulasuriya S, Ariyawardana A. Malignant transformation of oral leukoplakia: a systematic review of observational studies. J Oral Pathol Med. 2016; 45:155-66.
- Maloney B, Galvin S, Healy C. Oral leukoplakia: an update for dental practitioners. JIDA. 2024.
- van der Waal I. Historical perspective and nomenclature of potentially malignant or potentially premalignant oral epithelial lesions with emphasis on leukoplakia—some suggestions for modifications. Oral Surg, Oral Med and Oral Radiol. 2018; 125:577-81.
- Holmstrup P, Vedtofte P, Reibel J, Stoltze K. Oral premalignant lesions: is a biopsy reliable?. J Oral Pathol Med. 2007; 36:262-6.
- van der Waal I. Oral leukoplakia: present views on diagnosis, management, communication with patients, and research. Curr. Oral Health Rep. 2019; 6:9-13.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
