Research - (2021) Volume 9, Issue 11
Barriers to Dentist in Management of Patients with Special Health Care Needs
Milind Wasnik1*, Arun Sajjanar1, Suryakant Kumar1, Niharika Gahlod1, Sneha Khekade1, Miranda George2, Durga Bhattad1 and Pratima Kolekar1
*Correspondence: Milind Wasnik, Department of Pedodontics and Preventive Dentistry, Swargiya Dadasaheb Kalmegh Smruti Dental College and Hospital, Wanadongri, Hingna, Nagpur, Maharashtra, India, Email:
Abstract
Background: Special health care needs include one of the physical, behavioural, developmental, sensory, mental, cognitive or emotional impairment or generally a restraining condition that often requires medical management, health care intervention, along with that it also requires use of specialized services or programs. This condition is considered as developmental, congenital, or it may also be acquired through many reasons such as disease, trauma, or any of the environmental cause. The condition may compel limitations in doing daily self-maintenance activities or extensive limitations in a most of the life activity. Aim: The aim of the study was to investigate the barriers to dentist in management of patients with special health care needs. Methods: A self-administered questionnaire including 10 questions was developed and made available in paper formats. The questionnaire was circulated among 100 randomly selected dental practitioners from various parts of the Nagpur region. Results: The most common type of disabilities of children with special needs patients that mostly visited the dental clinic included physical disability (46%) and the preferred way of treatment of children with special healthcare was non pharmacological behaviour management technique (77%).Majority of dentists relied mainly upon general anaesthesia (65.7%) as the adjunct for behaviour management as compared to conscious sedation Conclusion: Training programs should be conducted regarding special needs dentistry which will improve the quality of patient care. The parents as well as the caregivers and the teachers of these children should be efficiently educated and also they must be trained regarding the dental problems, oral hygiene instructions and dietary practice of these children. They must also be trained regarding prevention of or facial trauma and first aid of special health care children.
Keywords
Special Child, Barrier, Dental Treatment, Oral Health, Disability
Introduction
Special health care needs include one of the physical, behavioural, developmental, sensory, mental, cognitive or emotional impairment or generally a restraining condition that often requires medical management, health care intervention, along with that it also requires use of specialized services or programs. This condition is considered as developmental, congenital, or it may also be acquired through many reasons such as disease, trauma, or any of the environmental cause. The condition may compel limitations in doing daily self-maintenance activities or extensive limitations in a most of the life activity. Providing the health care to children with special needs often requires specialized knowledge, as well as increased awareness, attention, accommodative and adaptation measures ahead of what are considered as routine [1].
Special needs is the terminology which is used in clinical, diagnostic as well as the functional development in order to describe individuals who require support for disabilities and these support includes medical, mental, or psychological. These patients who have disabilities have been called as either disabled, impaired, or handicapped. The term disability is been defined as any form of restriction of work or lack of ability in order to perform an activity in a normal way or within the manner which is generally considered as normal for a human being. Impairment refers to any form of loss or malformation in physiologic as well as anatomic structural function. Handicapped is defined as the drawback of a given individual which generally results from an impairment of disability. It generally limits or prevents the implementation of expectation or a role that is considered as normal for an individual.
Oral health is considered as a significant aspect of overall health. Oral health contributes to overall well-being and also the quality of life of each individual’s by certainly affecting physical, appearance, mental well-being and also the interpersonal relations. The oral health is considered as a significant aspect of general health for all children particularly for children with special health needs. As oral hygiene affects most commonly the children’s communication and aesthetics, it has strong biological, psychological as well as social effects [2]. In Children with disabilities oral health care and hygiene is one of the greatest health needs which are left unattended or untreated.
Generally the access of children with special health care needs to dental treatment may be limited either by the capability of their caregivers in order to evaluate their oral condition and/or by the children’s failure to express the pain or discomfort which they are experiencing. It has already been reviewed that Poor oral hygiene leads to greater prevalence and severity of periodontal disease in the disabled children. There are many etiologic factors which contribute to the high incidence of poor periodontal status in the special children. Other contributing factors like abnormal capillary morphology, connective tissue disorders and also the anatomical aspects of teeth, variation in immunological response may play an important role in the prevalence as well as the progression of the periodontal disease process [3,4].
The poor oral hygiene can be due to essential disabilities which ultimately reduce manual dexterity. The poor oral hygiene may also be the result of side effects of certain medications [5]. The indicators of poor oral health in children with disabilities includes decayed teeth, missing teeth, periodontal disease, mal-aligned or supernumerary teeth, malocclusion and prolonged retention of primary teeth [6]. Poor oral health has overall undesirable impact on nutrition, digestion and missing teeth ultimately affecting speech [7,8].In the children with who are having upper limb disability, the individual’s capability is affected in order to maintain proper and effective oral hygiene. Those children, who are dependent for proper oral hygiene, completely depend on the proper knowledge as well as the skills of their caregivers [9].
Pediatric health care provider has a vital and important role in behind the health and also the well-being of children and adolescents with special health care needs in all stages which include including early intervention (EI), preschool and also the school environments. It is also estimated that approximately 15% of children in the United States have a disability. Individuals with Disabilities Education Act (IDEA) entitle the entire affected children in the United States ranging from infancy to young adulthood to provide a free and suitable public education. These services strengthen the overall development of children along with it also improves the learning of children with various disabilities.
The categories of special education as defined by the Individuals with Disabilities Education Act (IDEA) 8 includes:
• Blindness.
• Intellectual disability.
• Emotional disturbance.
• Multiple disabilities.
• Autism.
• Orthopaedic impairment.
• Deafness.
• Hearing impairment.
• Specific learning disability.
• Speech or language impairment.
• Traumatic brain injury.
• Visual impairment.
• Other health impaired.
The three main factors including lack of information, access to dental clinic and transport facilities are consistently quoted by people with disabilities as being the key and important point to independence and choice of the proper dental treatment. For years children’s with Impaired mobility often leads to social isolation which eventually tends the people to have an inferior expectations regarding services. Along with this the physical environment and architectural infrastructure have been most of the time constructed without any reference to the needs of physically disabled people. Frequently the main problem is associated by stairs and other physical barriers which are normally present within the buildings. The barriers in provision of necessary dental care generally range from physical barriers in dental practices [9,10] economics [11] to inadequate education [12]. McIver described five key barriers to access dental care for children with SHCNs [13]. The key barriers were:
• The primary medical care system.
• The child’s parents.
• The child himself.
• The dentist.
• Payment for dental care.
Hence, this study was undertaken with the important aim of investigating the barriers to dentist in management of patients with special health care needs in various parts of the Nagpur region.
Methods
The difficulty faced by practitioners in providing adequate care to special children was produced by including variables on the location of the dental practice, accessibility to the clinic, suitable equipment for patient management, and readiness of practitioner and associate staff in the dental clinic to treat such individuals. A cross sectional study was done where a self-administered questionnaire including 10 questions was developed and made available in paper formats. The questionnaire was distributed among 100 randomly selected dental practitioners from various parts of the Nagpur region. The study was approved from institutional ethical committee and informed consent was taken before the study. The sample size was calculated by using convenient random sampling method. The Questionnaire was validated with two to three experts from subjects and with similar articles with modifications. The study was started from June 2019 to March 2020. The study extended for a total duration of 10 months. The responses were collected from the dentist in paper format.
Statistical analysis
Statistical analysis was done by using descriptive statistics using frequency and percentages. Data was entered in Excel sheet and software used for analysis was SPSS 27.0 version and p<0.05 is considered as level of significance.
Results
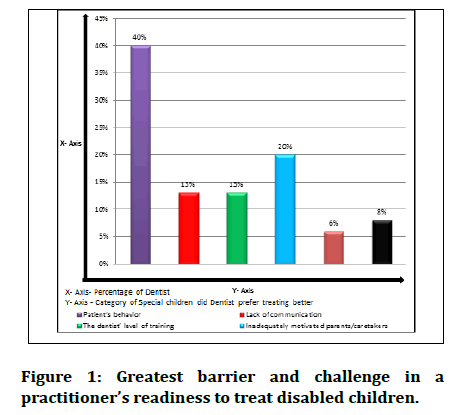
Majority of Dentist participating in the study have been practicing for 5-10 years. (66% Among the number of Pediatric Patients with Special needs per week visited their clinics 76% dentist said that it were less than 3 (Table 1. About 53% of dentists consider their Undergraduate dental education preparation as poor for managing patients with special needs (Table 1 and most of dentist preferred consulting Pediatric Dentist for treatment of children with special needs (78%. The most common type of disabilities of special needs patients that mostly visited the clinic included physical disability (46% and the preferred way of treatment of children with special healthcare was non pharmacological behavior management technique (77% (Table 2. The greatest barrier and challenge to treat disabled children experienced by all dentists was patient’s behavior (40%) (Figure 1)
| Sr. No. | Number of pediatric patients per week | Number of pediatric patients with special needs per week |
|---|---|---|
| 1 | 0 | Less than 3 |
| 21 (21%) | 76 (76%) | |
| 2 | 01-10 | More than 3 |
| 72 (72%) | 0 | |
| 3 | More than 10 | None |
| 7 (7%) | 24 (24%) |
Table 1: Data showing number of pediatric patients and pediatric patients with special needs visiting dental clinic per week.
| Sr. No. | Question | Options | Percentage |
|---|---|---|---|
| 1 | Undergraduate dental education preparation for managing patients with special needs | Excellent | 7 (7%) |
| Good | 23 (23%) | ||
| Fair | 20 (20%) | ||
| Poor | 53 (53%) | ||
| 2 | Clinic accessibility to special needs patients | Yes | 64 (64%) |
| No | 36 (36%) | ||
| 3 | Consulting Pediatric Dentist for treatment of children with special needs | Yes | 78 (78%) |
| No | 22(22%) | ||
| 4 | Types of disabilities of special needs patients that mostly visit clinic | Physical disabilities | 46(46%) |
| Mental disabilities | 23 (23%) | ||
| Medically impaired | 31 (31%) | ||
| 5 | Preferred way of treatment of children with special healthcare | Using Non-Pharmacological behavior management techniques | 77 (77%) |
| Conscious sedation | 15 (15%) | ||
| Under general | 8 (8%) |
Table 2: Data showing undergraduate dental education preparation, clinic accessibility, types of disabilities of special needs patients and preferred way of treatment for treating children with special needs.
Figure 1:Greatest barrier and challenge in a practitioner’s readiness to treat disabled children.
Discussion
The present study was conducted by collecting the data from dental practitioners who were randomly selected from various parts of the Nagpur region, India in order to determine the barriers observed by them in providing best possible dental care for children with special health care needs. The results of this study showed that maximum practitioners found that the lack of training is a prime barrier in providing dental care to children with and without special needs. In current study we found that about 13% practitioner found that lack of training also acts as a barrier in order to provide dental care to children with special needs which were in similar to the study of Bindal etal. [14], Rao et al. [15] and Daoet al. [16].
According toBindaletal14 dentists are generally prepared to provide treatment just at initial stage. So the dental practitioners should be trained properly during undergraduate programme regarding management of children with special health care needs and also dentist should be motivated in order to attend continuing dental education programme so that they can be able manage children’s with special health care needs in a effective and comprehensive manner. In spite of lack of training and also the other obstacles that dentists face while providing dental treatment to special children, most of the dental practitioners are willing to treat the children with special health care needs [14]. Similarly according to Rao etal15it is an obvious conclusion that variability in management has contributed to inequalities in oral health care for children with disabilities. Even though the dental profession wants to treat these children thecapability is sometimes constrained just because of a lack of knowledge and experience, and also a constrained work environment (including restricted financial resources) [15].
In the current study about 20% of the participants suggested that inadequately motivated caretaker’s acts as a relevant barrier and this observation was similar to that of findings conducted by Vignehsa et al. [17]. Russell and Kinirons et al. [18] and Owens et al. [19]. According to Edwards DM et al (2002); vast majority of dental professional reported that they treated patients with physical impairments, learning difficulties or mental health problems. This is similar to our study where we found that most common patients reported to the clinic were with Physical disabilities (46%), Mental disabilities (23%), medically impaired (31%). According to Adyanthaya et al. inaccessibility to the dental clinic was reported to be the main physical barrier to access to dental care.(71%). The inaccessibility to the dental clinic may be due to various factors such as clinic not being located on the ground floor, or if there is absence of ramp/lift facilities for wheelchair, etc. While in our study most dental professional said that there clinic was accessible to special needs patients (64%).
Priyadarshni Bindal et al., (2015) founded that Lack of training (60.8%), Financial issues (57.8%), Physical barriers (53.9%), Patient’s behavior (50%), Communication (44.1%), Dental treatment relapse (48%), Time constraint (48%) were the common challenges faced while treating special needs patients whereas in our study the most common barrier found by practitioners was Patient Behaviour (40%) and Least was Time constraints (8%).
Majority of dentists relied mainly upon general anaesthesia (65.7%) as the adjunct for behavior management compared to conscious sedation (2.9%). Dao et al. [16], Vignehsa et al. [17], Russell et al. [18]. It is contradictory to the fact where we found that most of the dental professionals preferred Non Pharmacological behavior management (80%) preferred way of treatment of children with special healthcare and least was general anaesthesia. (5%).Most commonly the attitudes to oral care and the knowledge of health professionals and health care workers are commonly identified as the principle barriers to oral health for people who are completely dependent for oral hygiene. All health professionals should primarily receive a supplementary training to support the primary concept of primary oral health care. There may be various limitations on the type as well as the quality of dental care that can be delivered at home but this may be the ultimate location to provide oral health advice to the individual and carers [19].
According to American Academy of Pediatric Dentistry Non-pharmacologic interventions may be effective alone in providing dental treatment or it may act as a adjuncts to pharmacological interventions in managing the pain, anxiety, and discomfort related to dental procedure along with minimal risk of adverse effects. By Creating a friendly environment in the dental clinic the child feels more comfortable and also less stressed. The American Academy of Paediatrics (AAP) and the American Pain Society (APS) also advise that reducing the stimulation which are distress-producing and providing a peaceful environment for all the dental procedures will improve in pain management. Principle key component in creating a comfortable environment is Emotional support. According to American Academy of Pediatric Dentistry Distraction of child is a very effective method in management of pain in the pediatric population. Distraction can be cognitive or behavioural. The main aim of both is to relocate attention away from pain. Various Distraction techniques can be used such as bubbles, conversation, counting, television, music, toys and video games. These techniques may be used by health care providers or the child’s caregiver to distract the child from pain. Imagery techniques in combination with distraction have been shown to be very helpful in reducing the postoperative pain in children [20].
According to Yi-Chia Wang et al Sedation and General Anaesthesia can help those children’s who are not capable to tolerate the dental treatment pain, such as children’s who experience anxiety and fear during dental visits. It is also helpful in those children who having cognitive impairment or any form of motor dysfunction. General anaesthesia is also useful in those children who are unable to tolerate physical stress. Proper preanaesthetic evaluation and preparations are important. There is certain form Mild anaesthetic complications in children with special health care needs who are treated with general anaesthesia. There should be full cooperation between Caretaker and Dentist. The most common indications for dental anaesthesia in patients who are younger than 14 years include lack of cooperation of child, multiple morbidities present and autism [21].
Conclusion
There are various factors which govern the dentist’s decision in providing care for children with special health care needs including financial, educational constraints, time and physical barriers in accessibility to a dental office which maybe worsened by insufficiently motivated primary caretakers. Training programs should be their regarding special needs dentistry in order to improve the quality of patient care. There should be effective education and training to parents, caregivers, and teachers of these children about the dental problems, along with the oral hygiene instructions and dietary practice and prevention of orofacial trauma and first aid of special health care children.
References
- American academy of pediatric dentistry definition of special health care needs. The Reference Manual of Pediatric Dentistry 2106- 19.
- Mitsea A, Karidis A, Donta-Bakoyianni C, et al. Oral health status in Greek children and teenagers, with disabilities. J Clin Pediatr Dent 2002; 26:111-8.
- Hennequin M, Faulks D, Roux O. Accuracy of estimation of dental treatment need in special care patients. J Dent 2000; 28:131-6.
- Rao D, Hegde A, Munshi AK. Periodontal status of disabled children in South Canara, Karnataka. J Indian Dent Assoc 2003; 74:559-62.
- Altun C, Guven G, Akgun OM, et al. Oral health status of disabled individuals oral health status of disabled individuals attending special schools. Eur J Dent 2010; 4:361-6.
- Gordon SM, Dionne RA, Snyder J. Dental fear and anxiety as a barrier to accessing oral health care among patients with special health care needs. Spec Care Dentist 1998; 18:88-92.
- Scott A, March L, Stokes ML. A survey of oral health in a population of adults with developmental disabilities: Comparison with a national oral health survey of the general population. Aust Dent J 1998; 43:257-61.
- Lipkin PH, Okamoto J. The individuals with disabilities education act (IDEA) for children with special educational needs. Pediatrics 2015; 136:e1650-62.
- Oliver CH, Nunn JH. The accessibility of dental treatment to adults with physical disabilities in northeast England. Spe Care Dentis 1996; 16:204-9.
- Merry AJ, Edwards DM. Disability Part 1: The disability discrimination act (1995)–implications for dentists. Br Den J 2002; 193:199-201.
- O’Donnell D, Sheiham A, Yeung KW. The willingness of general dental practitioners to treat people with handicapping conditions: The Hong Kong experience. J R SocPromot Health 2002; 122:175-80.
- Smith CS, Ester TV, Inglehart MR. Dental education and care for underserved patients: an analysis of students’ intentions and alumni behavior. J Den Edu 2006; 70:398-408.
- McIver FT. Access to care: A clinical perspective. In: Mouradian W. Proceedings: Promoting oral health of children with neurodevelopmental disabilities and other special health care needs: A meeting to develop training and research agendas, center on human development and disability. Seattle, Washington: University of Washington 2001; 167-71.
- Bindal P, Chai WL, Bindal U, et al. Dental treatment and special needs patients (SNPs): Dentist's point of view in selected cities of Malaysia. Biomed Res 2015; 26:152-6.
- Rao D, Amitha H, Munshi AK. Oral hygiene status of disabled children and adolescents attending special schools of South Canara, India. Hong Kong Dent J 2005; 2:107-2.
- Dao LP, Zwetchkenbaum S, InglehartMR. General dentists and special needs patients: Does dental education matter? J Dent Educ 2005; 69:1107-15.
- Vignehsa H, Soh G, Lo GL, et al. Dental health of disabled children in Singapore. Aust Dent J 1991; 36:151-6.
- Russell GM, KinironsMJ. A study of the barriers to dental care in a sample of patients with cerebral palsy. Community Dent Health 1993; 10:57-64.
- Owens J. Barriers to oral health promotion in the Republic of Ireland. Scand J Public Health 2011; 39:93-97.
- Merry AJ, Edwards DM. Disability part 1: The disability discrimination act (1995)–Implications for dentists. Br Dent J 2002; 193:199-201
- Adyanthaya A, Sreelakshmi N, Ismail S, et al. Barriers to dental care for children with special needs: General dentists’ perception in Kerala, India. J Indian Soc Pedod Prev Dent 2017; 35:216-222.
Author Info
Milind Wasnik1*, Arun Sajjanar1, Suryakant Kumar1, Niharika Gahlod1, Sneha Khekade1, Miranda George2, Durga Bhattad1 and Pratima Kolekar1
1Department of Pedodontics and Preventive Dentistry, Swargiya Dadasaheb Kalmegh Smruti Dental College and Hospital, Wanadongri, Hingna, Nagpur, Maharashtra, India2Department of Pedodontics and Preventive Dentistry, Pushpagiri College of Dental Sciences, Thiruvalla, India
Citation: Milind Wasnik, Arun Sajjanar, Suryakant Kumar, Niharika Gahlod, Sneha Khekade, Miranda George, Durga Bhattad, Pratima Kolekar Barriers to Dentist in Management of Patients with Special Health Care Needs, J Res Med Dent Sci, 2021, 9(11): 217-222
Received: 30-Sep-2021 Accepted: 10-Nov-2021