Research - (2020) Advances in Dental Surgery
Association Between Orthodontics and Temporomandibular Disorders
Nashwah Hinaz1, Sri Rengalakshmi1* and Ashok V2
*Correspondence: Sri Rengalakshmi, Department of Orthodontics, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, Chennai, India, Email:
Abstract
Temporomandibular disorders are muscular and articular disorders. The role of morphological and functional occlusion in the development as a cause for temporomandibular disorder has been a matter of debate for a long time. Occlusal interference, class II, class III malocclusion, anterior open bite, posterior crossbite, and over jet has been related to TMD. The aim of the study is to evaluate the association of orthodontic malocclusion with temporomandibular joint disorder. Data is collected from June 2019 to March 2020 from Saveetha Dental College and hospitals, Chennai. The collected data is tabulated in excel sheet and software analysis using SPSS is done to obtain results. The mean age of participants is 34.86 years. A total of 15 patients were a part of the study. Out of which, 53.33% were males and 46.66% of females. The presence of malocclusion due to TMD was class I (33.33%), class II (46.66%), class III (13.33%). Within limits of the study, there is significant prevalence of TMD in relation to class II Malocclusion.
Keywords
Malocclusion, TMD, Orthodontics, Facial pain, TMD dysfunction
Introduction
Temporomandibular joint disorder is defined as a muscular and articular disorder [1]. The American Association of Dental Research (AADR) recognizes that temporomandibular disorders (TMD) encompass a group of musculoskeletal and neuromuscular conditions that involve the temporomandibular joints, the masticatory muscles, and all associated tissues. They also are frequently associated with acute or persistent pain, and the patients often suffer some other painful disorders. In the chronic forms of TMD, pain may cause work absenteeism or some degree of impairment, resulting in an overall reduction in the quality of life [2]. TMD are considered multifactorial etiology conditions involving trauma, anatomical, pathophysiological, and psychosocial factors [3,4].To diagnose presence of TMD, certain analysis such as softtissue analysis is done which is an important component of orthodontic diagnosis and treatment planning. Photographic evaluation of a patient is considered very essential as well [5]. It is seen that there is an association between TMD and gonial angle, it can be used to assess growth patterns as it acts as a growth indicator [6]. The role of morphological and functional occlusion in their development has been a matter of debate for a long time. Malocclusions are one of the most common factors for TMD. Hence Craniofacial and cephalometric analysis can be done for evaluation of craniofacial, skeletal and dentoalveolar profiles to determine the structural and architectural imbalance and quantify skeletal contribution in malocclusion and assess dental status for class I, II or III status which can contribute to TMD [7].
Occlusal interferences, class II or III malocclusions, anterior open bite, excessive overjet or posterior crossbite have been related to TMD. Furthermore, orthodontic treatment as a contributing factor for the development of TMD has been the subject of many studies [8]. Malocclusions in young individuals can occur as they develop. This could be due to traumatic injury of the deciduous tooth, leading to severe deep bite [9]. Fractures also frequently occur in young patients, thus affecting the temporomandibular joint function [10]. Orthodontic treatments are done for patients with malocclusions and mild TMD.Orthodontic treatment involves the application of forces that are continuous in activity on as many areas of the dentition as possible [11,12]. However, these forces can cause severe stress [13,14]. Hence success and failure of an orthodontic treatment depends on various characteristics during the course of the treatment [15–17]. However orthodontic treatments are contraindicated in case of severe TMD. On the other hand, several studies demonstrate no relation between orthodontics and TMD [18]. Signs and symptoms of TMD are relatively common in adolescents as several longitudinal studies have shown that clinical signs of TMD increase with age, appearing especially during the second decade of life [19,20].
Previous studies have been done to understand the association between malocclusion, and TMD. It also demonstrates the challenges faced by them during the study. In a study by Schmitter M et al, The cause-effect relationship between TMD and malocclusion is difficult to demonstrate because of the incidence of TMD among people of an early age and therefore they could show signs and symptoms of TMD either before, during or after ort-hodontic treatment [19]. Studies show that the duration of orthodontic treatment is increased for patients under Bisphosphonate therapy as the bone turnover is delayed [21]. Studies done by Reynders RM. et al (1988) and Greene et al (2012), demonstrate the complications of conducting the study that includes lack of patient cooperation due to severe pain and dysfunction [22,23]. In a study by Kim et al (2002), the challenges faced is heterogeneity, Because of heterogeneity, a definitive conclusion cannot be drawn for association between malocclusion & Temporomandibular disorders [24].
The Purpose of this study is to understand the relationship between malocclusions and the temporomandibular disorder. Various categories of malocclusion contribute to temporomandibular disorders. This includes class I malocclusion with crowding, deep bite, retroclination, edge to edge contact, scissor bite , class II malocclusions (class 2 div 1, class 2 div 2, subdivision) class III malocclusions. Aim of this study is to evaluate the association of malocclusion with temporomandibular disorders.
Materials and Methods
Study setting
University based study was conducted from June 2019 to March 2020 where two people are involved (one guide and one researcher). This enables easy retrieval of data over a specific period of time. However the data collection is not location specific. The study was conducted with the approval of the Institutional Ethics Committee [SDC/SIHEC/2020/DIASDATA/0619-0320]. It involves one guide and one researcher to carry the study.
Sampling
The cross verification of data is done using photographs. Sampling bias is minimised by inclusion of all the data and exclusion of the inappropriate data. Internal validity consists of samples from the University which provides proper records and enables better recall and review results. External validity is that the results can be generalised as samples of one ethnic group.
Data collection and statistical analysis
Data is collected by reviewing the patient records and analysing the data of patients reporting to the institute. Excel tabulation is done and data is entered as age of the patient, name of the patient, type of malocclusion, presence of TMD. Results are generated using the statistical software SPSS Windows version 20 (IBM). Incomplete/ censored data is managed by excluding from data. Descriptive analysis by mean, range with tables and charts are obtained using the SPSS software. The independent variables include age and sex of the patient. The dependent variable is the type of malocclusion and the type of analysis is correlation and association.
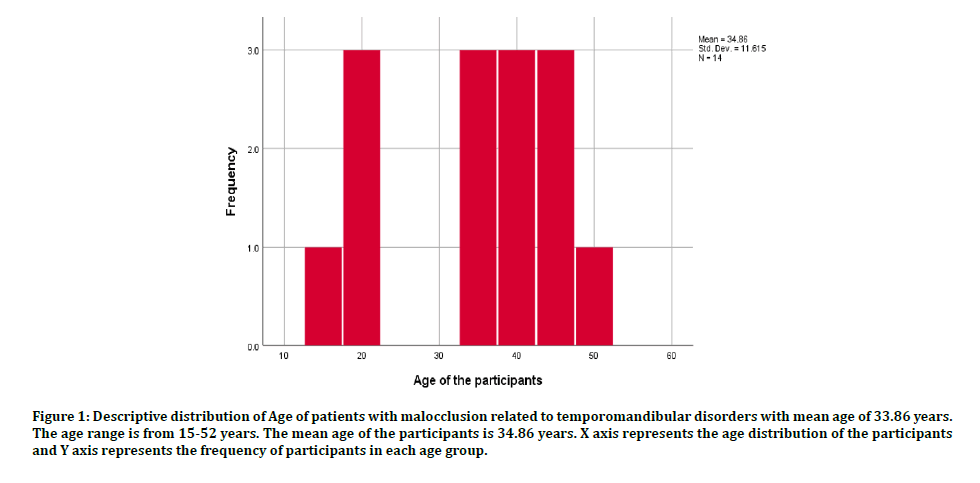
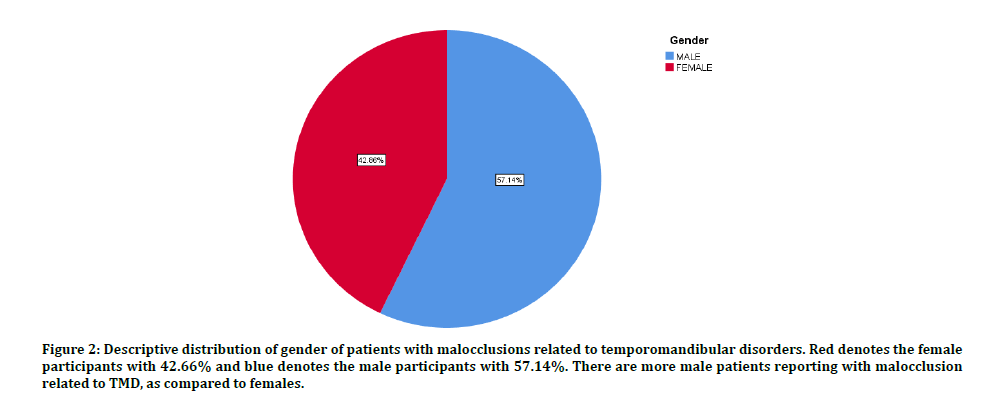
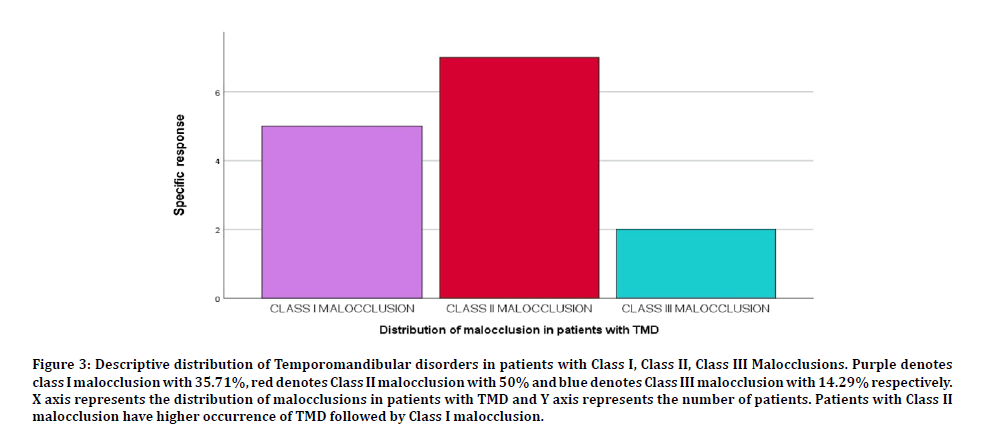
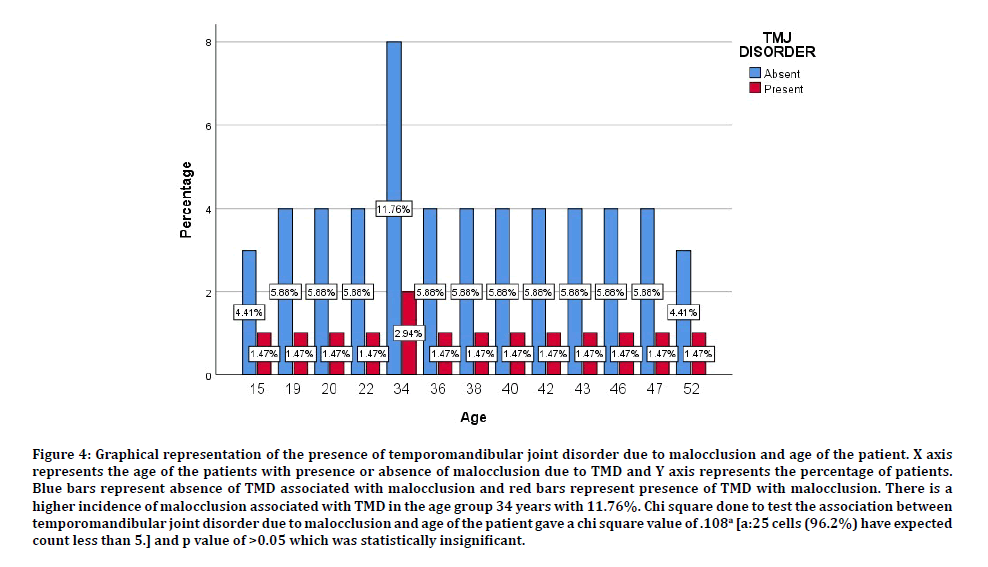
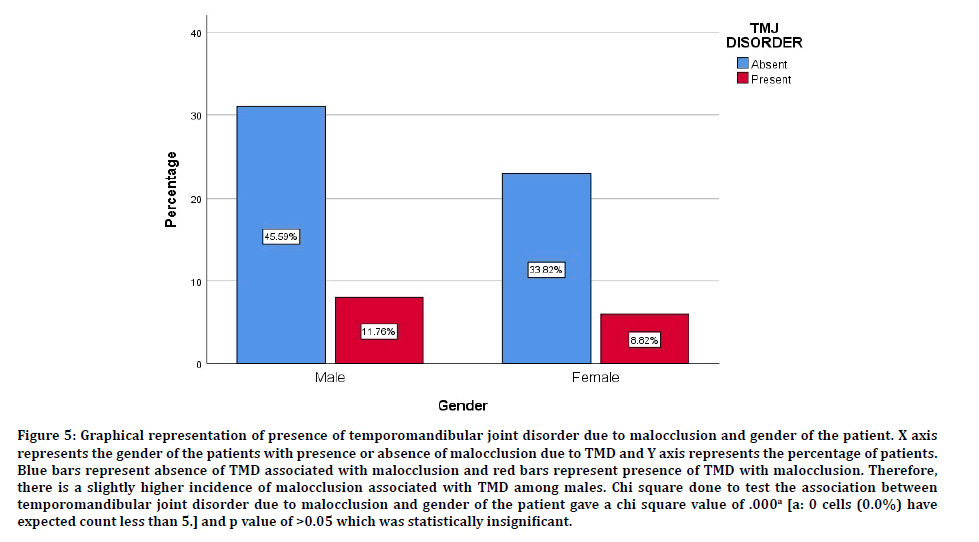
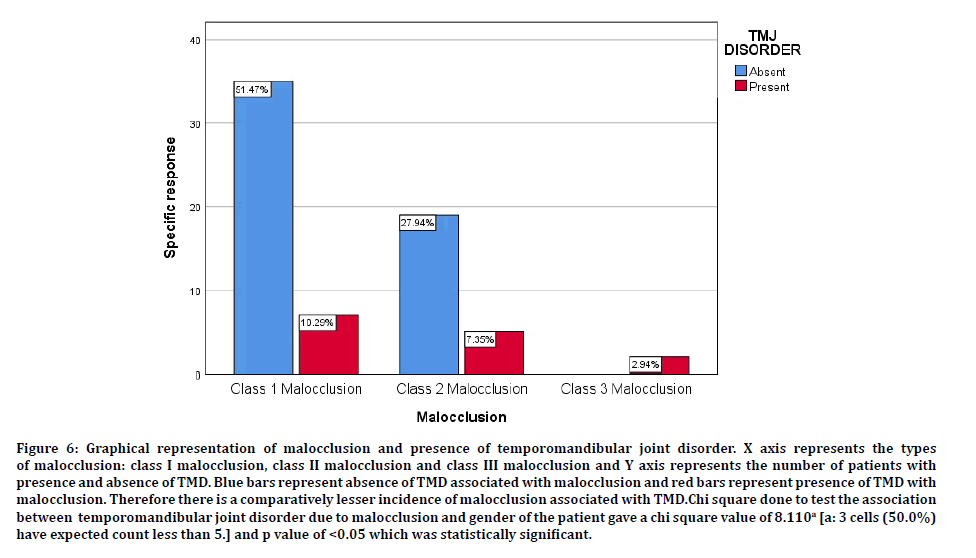
A total of 69 patients had temporomandibular joint disorder out of which 15 participants had TMD due to malocclusion. The mean age of the participants is 34.86 years. The age range is between 15-52 years as shown in Figure 1. Out of the 15 participants, 8 were male (57.14%) and 7 were female (42.66%) as shown in (Figure 2). The presence of various malocclusions related to temporomandibular disorder was seen as Class I (35.71 %) which included patients having crowding, deep bite, retroclination, edge to edge contact, scissor bite, Class II (50%) amd Class III (14.29%) as shown in (Figure 3). There is no significant association between the presence of temporomandibular joint disorder due to malocclusion with age and gender of the patient as shown in Figures 4 and 5. There is association between the malocclusion and presence of temporomandibular joint disorder as shown in Figure 6.
Figure 1: Descriptive distribution of Age of patients with malocclusion related to temporomandibular disorders with mean age of 33.86 years. The age range is from 15-52 years. The mean age of the participants is 34.86 years. X axis represents the age distribution of the participants and Y axis represents the frequency of participants in each age group.
Figure 2: Descriptive distribution of gender of patients with malocclusions related to temporomandibular disorders. Red denotes the female participants with 42.66% and blue denotes the male participants with 57.14%. There are more male patients reporting with malocclusion related to TMD, as compared to females.
Figure 3: Descriptive distribution of Temporomandibular disorders in patients with Class I, Class II, Class III Malocclusions. Purple denotes class I malocclusion with 35.71%, red denotes Class II malocclusion with 50% and blue denotes Class III malocclusion with 14.29% respectively. X axis represents the distribution of malocclusions in patients with TMD and Y axis represents the number of patients. Patients with Class II malocclusion have higher occurrence of TMD followed by Class I malocclusion.
Figure 4: Graphical representation of the presence of temporomandibular joint disorder due to malocclusion and age of the patient. X axis represents the age of the patients with presence or absence of malocclusion due to TMD and Y axis represents the percentage of patients. Blue bars represent absence of TMD associated with malocclusion and red bars represent presence of TMD with malocclusion. There is a higher incidence of malocclusion associated with TMD in the age group 34 years with 11.76%. Chi square done to test the association between temporomandibular joint disorder due to malocclusion and age of the patient gave a chi square value of .108a [a:25 cells (96.2%) have expected count less than 5.] and p value of >0.05 which was statistically insignificant.
Figure 5: Graphical representation of presence of temporomandibular joint disorder due to malocclusion and gender of the patient. X axis represents the gender of the patients with presence or absence of malocclusion due to TMD and Y axis represents the percentage of patients. Blue bars represent absence of TMD associated with malocclusion and red bars represent presence of TMD with malocclusion. Therefore, there is a slightly higher incidence of malocclusion associated with TMD among males. Chi square done to test the association between temporomandibular joint disorder due to malocclusion and gender of the patient gave a chi square value of .000a [a: 0 cells (0.0%) have expected count less than 5.] and p value of >0.05 which was statistically insignificant.
Figure 6: Graphical representation of malocclusion and presence of temporomandibular joint disorder. X axis represents the types of malocclusion: class I malocclusion, class II malocclusion and class III malocclusion and Y axis represents the number of patients with presence and absence of TMD. Blue bars represent absence of TMD associated with malocclusion and red bars represent presence of TMD with malocclusion. Therefore there is a comparatively lesser incidence of malocclusion associated with TMD.Chi square done to test the association between temporomandibular joint disorder due to malocclusion and gender of the patient gave a chi square value of 8.110a [a: 3 cells (50.0%) have expected count less than 5.] and p value of <0.05 which was statistically significant.
Discussion
In this study, the mean age of the participants is 34.86 years with the age range between 15-52 years. Similarly in study by Sim- Hye-Young, et al (2019), the mean age of participants was 46.6 years. Importantly, most patients are children and adolescents, such age- and gender-related coincidences cause difficulty in defining the relationship between malocclusion and TMD [25]. Similarly, Longitudinal studies by Egermark et al (2003) and Macfarlane et al (2009), have shown an increase in the prevalence of signs and symptoms of TMD with age, with a greater prevalence of signs than symptoms. Therefore, it is important to include a comprehensive physical examination as part of the diagnostic process For the early detection of TMD and well-being of the patient [26,27]. In this study males have a higher prevalence 53.33% and females contribute 46.66% of total number of participants. In this study, class I comprises 33.33% of malocclusion due to temporomandibular disorders, and class II has 46.6% followed by class III with 13.33% respectively. The class I malocclusion encountered included patients with crowding , deep bite, retroclination, edge to edge contact, scissor bite and class II malocclusions included class 2 division 1, class 2 division 2, subdivision). Similarly, Paulsen Hu et al (2002) and Henrikson et al (2000), demonstrated that subjects with untreated crossbite, crowding or large overjet showed a higher prevalence of signs and symptoms of Temporomandibular disorder [28,29]. Henrikson et al. in a study conducted on 183 patients, reported lower prevalence of signs and symptoms of TMD in patients with class I malocclusion than in those with class II malocclusion [30]. Additionally, Egemark et al. analysed the influence of TMDs in three samples of children of 7, 11 and 15 years, reporting morphological criteria such as class II, class III, anterior open bites and posterior crossbites as potential factors of predisposition to TMDs associated with functional malocclusions [31]. Deep bite correction with mini implants will result in effective bite opening through true intrusion of incisors [32]. Thus, preventing TMD. Furthermore, Kim TW et al, showed subjects with Class II malocclusion had increased rates of TMD among orthodontic treatment patients [33]. Several studies have associated unilateral posterior crossbite in children with an increased probability of developing signs and symptoms of TMD [34]. It is also seen that Obstructive sleep apnea has a significant correlation to temporomandibular joint dysfunction, the presence of risk factors such as age, gender and obesity increased the incidence of OSA [35].
In a study contradicting to our findings by Fernández-González et al. demonstrated that majority of the results showed a relationship between TMD and female sex and a fluctuation of its manifestations over time [36]. In a study by Tanne et al. no significant differences in the prevalence of TMD were observed between the sexes [37]. Some studies show that the major problems when interpreting associations between malocclusion and TMD is whether the recorded variables represent a severe enough condition to motivate patients to seek treatment for the functional problems [29].
On correlating this study with previous literatures, it is seen that differences in results based on gender is present. The major factor influencing this could be due to the variation in the sample size and population. It is also seen this study is in accordance with previous literatures based on association of TMD and malocclusions, there is a relationship between the class I, class II and class III malocclusion with the prevalence of temporomandibular joint disorders among patients. Therefore these conditions require treatment so as to avoid further complications due to malocclusion and associated pain and complications due to temporomandibular disorder. There are certain limitations of the study, due to the limited sample size and population. There could also be a subjective error or bias during the study. Future scope of the study is that the other parts of the population should be covered and study should be conducted for a larger group of people to obtain better results.
Conclusion
Within the limits of this study, there is a significant Association between malocclusion and temporomandibular joint disorders which is greatly influenced by the age of the individual and the type of malocclusion present.
References
- Laplanche O, Pedeutour P, Duminil G, et al. L’urgence des dysfonctionnements de l’appareil manducateur. Rev Orthop Dento Faciale 2011; 45:159–174.
- Klasser GD, Greene CS. Predoctoral teaching of temporomandibular disorders. J Am Dent Assoc 2007; 138:231–237.
- Liu F, Steinkeler A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent Clin North Am 2013; 57:465–479.
- Caroline Ceneviz, Noshir Mehta, Steven Scrivani, et al. Incidence of bruxism in TMD population. N Y State Dent J 2011; 77:54.
- Saravana Pandian K, Krishnan S, Aravind Kumar S, et al. Angular photogrammetric analysis of the soft-tissue facial profile of Indian adults. Indian J Dent Res 2018; 29:137.
- Rubika J, Sumathi Felicita A, Sivambiga V, et al. Gonial angle as an indicator for the prediction of growth pattern. World J Dent 2015; 6: 161–163.
- Felicita A, Shanthasundari KK, Chandrasekar S, et al. Determination of craniofacial relation among the subethnic Indian population: A modified approach-(Sagittal relation). Indian J Dent Res 2012; 23: 305.
- Luther F. TMD and occlusion part I. Damned if we do? Occlusion: The interface of dentistry and orthodontics. Br Dent J 2007; 202:E2.
- Felicita AS, Sumathi Felicita A. Orthodontic management of a dilacerated central incisor and partially impacted canine with unilateral extraction–A case report. Saudi J Dent Res 2017; 29:185–193.
- Felicita AS, Sumathi Felicita A. Orthodontic extrusion of ellis class VIII fracture of maxillary lateral incisor–The sling shot method. Saudi J Dent Res 2018; 30:265–269.
- Dinesh SPS, Arun AV, Sundari KKS, et al. An indigenously designed apparatus for measuring orthodontic force. J Clin Diagn Res 2013; 7:2623.
- Felicita AS, Sumathi Felicita A. Quantification of intrusive/retraction force and moment generated during en-masse retraction of maxillary anterior teeth using mini-implants: A conceptual approach. Dental Press J Orthod 2017; 22:47–55.
- Vikram NR, Prabhakar R, Kumar SA, et al. Ball headed mini implant. J Clin Diagn Res 2017;11: ZL02.
- Sivamurthy G, Sundari S. Stress distribution patterns at mini-implant site during retraction and intrusion—A three-dimensional finite element study. Prog Orthod 2016; 17:4.
- Kumar KRR, Ramesh Kumar KR, Shanta Sundari KK, et al. Depth of resin penetration into enamel with 3 types of enamel conditioning methods: A confocal microscopic study. Am J Orthodont Dentofac Orthop 2011; 140: 479–485.
- Samantha C, Sundari S, Chandrasekhar S, et al. Comparative evaluation of two Bis-GMA based orthodontic bonding adhesives-A randomized clinical trial. J Clin Diagn Res 2017; 11:ZC40.
- Kamisetty SK, Verma JK, Arun SS, et al. SBS vs inhouse recycling methods-An invitro evaluation. J Clin Diagn Res 2015; 9:ZC04.
- Bourzgui F, Sebbar M, Nadour A, et al. Prevalence of temporomandibular dysfunction in orthodontic treatment. Int Orthod 2010; 8:386–398.
- Schmitter M, Rammelsberg P, Hassel A, et al. The prevalence of signs and symptoms of temporomandibular disorders in very old subjects. J Oral Rehabil 2005; 32:467–473.
- Kindler S, Schwahn C, Bernhardt O, et al. Association between symptoms of posttraumatic stress disorder and signs of temporomandibular disorders in the general population. J Orofac Pain 2019; 33:67–76.
- Krishnan S, Saravana Pandian AKS. Effect of bisphosphonates on orthodontic tooth movement—An update. J Clin Diagn Res 2015; 9:ZE01.
- Reynders RM. Orthodontics and temporomandibular disorders: A review of the literature (1966–1988). Am J Orthod Dentofac Orthop 1990; 97:463–471.
- Greene CS, Stockstill J, Rinchuse D, et al. Orthodontics and temporomandibular disorders: A curriculum proposal for postgraduate programs. Am J Orthod Dentofacial Orthop 2012; 142:18–24.
- Kim M-R, Graber TM, Viana MA. Orthodontics and temporomandibular disorder: A meta-analysis. Am J Orthod Dentofacial Orthop 2002; 121:438–446.
- Sim HY, Kim HS, Jung DU, et al. Investigation of the association between orthodontic treatment and temporomandibular joint pain and dysfunction in the South Korean population. Korean J Orthod 2019; 49:181–187.
- Egermark I, Magnusson T, Carlsson GE, et al. A 20-year follow-up of signs and symptoms of temporomandibular disorders and malocclusions in subjects with and without orthodontic treatment in childhood. Angle Orthod 2003; 73:109–115.
- Macfarlane TV, Kenealy P, Kingdon HA, et al. Twenty-year cohort study of health gain from orthodontic treatment: Temporomandibular disorders. Am J Orthod Dentofacial Orthop 2009; 135:692.e1–692.e8.
- Paulsen HU, Karle A. Computer tomographic and radiographic changes in the temporomandibular joints of two young adults with occlusal asymmetry, treated with the Herbst appliance. Eur J Orthod 2000; 22:649–656.
- Henrikson T, Nilner M, Kurol J, et al. Signs of temporomandibular disorders in girls receiving orthodontic treatment. A prospective and longitudinal comparison with untreated Class II malocclusions and normal occlusion subjects. Eur J Orthod 2000; 22:271–281.
- Henrikson T, Nilner M. Temporomandibular disorders, occlusion and orthodontic treatment. J Orthod 2014; 16.
- Egermark I, Carlsson GE, Magnusson T, et al. A 20-year longitudinal study of subjective symptoms of temporomandibular disorders from childhood to adulthood. Acta Odontol Scand 2001; 59: 40–48.
- Jain RK, Kumar SP, Manjula WS, et al. Comparison of intrusion effects on maxillary incisors among mini implant anchorage, j-hook headgear and utility arch. J Clin Diagn Res 2014; 8:ZC21.
- Kim TW, Byun ES, Baek SH, et al. MRI study of temporomandibular joint disorder in orthodontic patients. Korean J Orthod 2000; 30:235–243.
- McNamara JA. Early intervention in the transverse dimension: Is it worth the effort? Am J Orthod Dentofacial Orthop 2002; 121:572–574.
- Viswanath A, Ramamurthy J, Dinesh SPS, et al. Obstructive sleep apnea: Awakening the hidden truth. Niger J Clin Pract 2015; 18:1–7.
- Fernández-González FJ, Cañigral A, López-Caballo JL, et al. Influence of orthodontic treatment on temporomandibular disorders. A systematic review. J Clin Exp Dent 2015; 7:e320.
- Tanne K, Tanaka E, Sakuda M, et al. Association between malocclusion and temporomandibular disorders in orthodontic patients before treatment. J Orofac Pain 1993; 7.
Author Info
Nashwah Hinaz1, Sri Rengalakshmi1* and Ashok V2
1Department of Orthodontics, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, Chennai, India2Department of Prosthodontics, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, Chennai, India
Citation: Nashwah Hinaz, Ashok V, Sri Rengalakshmi, Association Between Orthodontics and Temporomandibular Disorders, J Res Med Dent Sci, 2020, 8 (7): 371-377.
Received: 29-Sep-2020 Accepted: 04-Nov-2020 Published: 11-Nov-2020