Research Article - (2022) Volume 10, Issue 5
Assessment of Rate of Wound Healing in Patients Using rh- EGF dressing for the Management of Diabetic Foot Ulcers
Karan Kumar Jain*, Raghuram and Baskaran PK
*Correspondence: Karan Kumar Jain, Department of General Surgery, Sree Balaji Medical College and Hospital, Bharath University, Chennai, Tamil Nadu, India, Email:
Abstract
Background: Diabetic foot ulcers are the most common cause of chronic, non healing ulcers. These foot ulcers are the cause for majority of the amputations. Management of these ulcers require a multidisciplinary approach. The field of wound management has evolved considerably after the understanding of the role of growth factors in wound healing. EGF is available commercially and has shown to promote wound healing.
Methods: This is a descriptive study which was performed prospectively at Sree Balaji medical College and Hospital during the period of June 2018 to December 2018. 100 patients meeting the inclusion criteria where included in the study. The surface area of the ulcers of these patients who were using rh-EGF dressing were measured at the start of the study, at 1 week and at 2 weeks to assess the rate of wound healing.
Results: Most patients belonged to 61-70 years of age. In this study the most patients affected were males. The most common site of ulcer was on the plantar aspect. The most common cause was found to be traumatic. The percentage of wound contraction at 1 week found to be 10.21% and at two weeks was found to be 26.77%.
Conclusion: The use of rh-EGF gel is safe and effective form of dressing and it promotes wound healing.
Keywords
Diabetic foot ulcer, EGF, DressingIntroduction
Diabetes mellitus directly or indirectly is a cause of lot of morbidity and mortality all around the world. Diabetic patients through various mechanisms are prone to infections which necessitates hospital admission. Foot infections, Ulcerations and gangrene are well documented complications of diabetes mellitus. Diabetic foot ulcers are the most common cause of chronic, non healing wounds which occur in approximately 10% to 15% of the patients. Among them about 12% to 24% individuals undergo amputations [3]. These diabetic foot ulcers are resistant to heal due to various factors like presence of infections and micro vascular complications [1,2].
Management of such ulcers is challenge and requires multidisciplinary approach and various modalities of treatment. The treatments of such ulcers consist of removal of necrotic tissue, growing infections and to make the conditions inside the wound environment favourable to facilitate healing. This consists of various types of debridement, proper use of antibiotics, creating proper moisture balance, correct use of various types of dressings and topical agents, glycaemic control, offloading etc. [3]. With advances in materials and tissue science, and improved knowledge in the concepts of wound healing and cell types involved, the field of wound management has evolved considerably. The understanding of the role of various growth factors in wound healing over recent years has brought an interest in their usage in chronic ulcer management [4].
These growth factors are polypeptides similar to hormones and control the growth differentiation and metabolism of cells and regulate the process of wound healing. These growth factors have proven their role in cell proliferation, angiogenesis and wound healing [5]. With the advent of recombinant technology it is now possible to generate required quantity of these growth factors for usage in the management of diabetic foot ulcer management [6]. They are produced by various cells like platelets, macrophages, fibroblasts etc. and they also act as chemo-attractants for neutrophils, macrophages etc. They bind to specific receptors on the cell surface and exert their effects. Epidermal growth factor acts by binding with high affinity to epidermal growth factor receptors present in the cell surface, which in turn stimulates ligand-induced dimerization. It was reported that Recombinant human epidermal growth factor can be used effectively in the management of diabetic foot ulcers. Recombinant epidermal growth factors act by increasing the rate of wound healing in patients with diabetic foot ulcers.
Materials and Methods
This is descriptive study which was performed prospectively in the Department of General Surgery of Sree Balaji Medical College and Hospital, Chennai during the period of June 2018 to December 2019.
Inclusion Criteria
• Age between 20 to 80 years
• Ulcers falling under grade 1 and 2 of Wagner’s classification
• Ulcers with adequate perfusion
• Patients using rh-EGF dressing for the management of ulcers
Exclusion Criteria
• Patients below 20 years and above 80 years of age
• Poor glycaemic control (HbA1 c>10%)
• Severe anaemia (Hb<7 gm/dl)
• Ulcers falling under grade 3,4,5 of Wagner classification
• Ischemic ulcers with Doppler proven occlusion of the vessels
• Osteomyelitis of the foot with ulcers
• Malignant ulcers
• Patients using any other modality of dressing or topical agents
100 patients undergoing treatment for the diabetic foot ulcer in the form of rh-EGF dressing meeting the mentioned criteria were selected for the study after obtaining written and informed consent. All the patients were advised diabetic diet. Good glycaemic control was achieved either through oral hypoglycaemic agents or insulin. Wound swab was taken at the start of the study and was sent for culture and antibiotics were started according to the sensitivity reports. The ulcers were cleaned with normal saline first and then a commercially available preparation of rh-EGF topical application gel was applied over it. Moist Gauze piece was placed over the ulcer and covered with pad and roller bandage. Dressings were changed daily.
The ulcer area was measured by cutting a gauze piece to its size and measuring the surface area using plannimeter. Initial area of the ulcer was measured at the start of the study. Then the area measurement was repeated again at 1 week and 2 weeks. The reduction in area of the wound over time is the rate of wound healing and it was calculated using the following formula.
Percentage of area reduction=(initial area at repeat measurement )/initial area x 100
Statistical analysis
The outcome of the study was analysed statistically to reach a conclusion. Data entry was done using MS excel 2016. Demographics of the study such as Age, Gender, and Mode of onset, Site of ulcer and Anti Diabetic agent used were also assessed.
Results
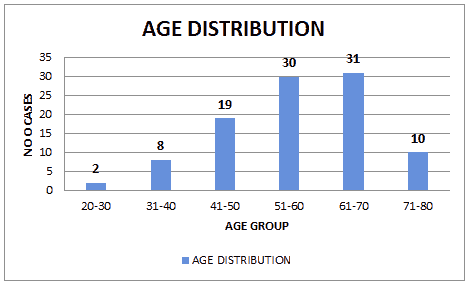
Figure 1: Age distribution
As shown in Figure 1, most of the patients in our study belonged to the age group between 61 to 70 years of age with youngest patient being 26 years and oldest patient being 79 years and an average age of 60.9 years.
Table 1: Gender distribution.
| Gender | Male | Female |
|---|---|---|
| NO OF CASES | 65 | 35 |
As shown in Table 1, Diabetic foot ulcers were most commonly seen in males (65%) than in females (35%).
Table 2: Distribution based on site of the ulcer.
Site of the ulcer |
No of cases |
|---|---|
PLANTAR |
70 |
DORSAL |
30 |
As shown in Table 2, the most common site of ulcer in our study was in the plantar aspect of the foot (70%) compared to the dorsal aspect of the foot (30%).
Table 3: Distribution based on type of onset.
| Type of onset | No of cases |
|---|---|
| Traunatic | 68 |
| Spontaneous | 32 |
| Total | 100 |
As shown in Table 3, in our study traumatic type of onset (68%) was more common than spontaneous onset (32%).
Table 4: Distribution based on type of anti-diabetic agent used.
| Anti-diabetic agent | No of cases |
|---|---|
| Insulin | 71 |
| Oral hypoglycaemic agent | 29 |
| Total | 100 |
As shown in Table 4, most patients in our study used insulin (71%) for glycaemic control as compared to oral hypo glycaemic agents (29%).
Table 5: Mean surface area of the ulcers.
| Size of the ulcer (in cm2) | Mean | Standard deviation | Median |
|---|---|---|---|
| 34.29 | 8.4 | 35.43 |
Table 6: Percentage of area reduction of ulcer at 1 week.
| Percentage of area reduction of ulcer | Mean | Standard deviation | Median |
|---|---|---|---|
| 10.21 | 1.7 | 10.55 |
Table 7: Percentage of area reduction of ulcer at 2 weeks.
| Percentage of area reduction of ulcer | Mean | Standard deviation | Median |
|---|---|---|---|
| 26.77 | 2.61 | 25.61 |
As shown in Table 5, the mean size of the ulcers in our study was 34.29 cm2. There was a 10.21% of area reduction in patients using rh-PDGF gel topical application at 1 week and 26.77% of area reduction at 2 weeks (Tables 6 and Table 7).
Discussion
DM foot ulcers are chronic non healing ulcers which show a long inflammatory phase and there is a halt in the epidermal growth. This none healing of the ulcers are also due to the growth of multi drug resistant organisms and also due to micro vascular complications of diabetes mellitus [6].
This study was conducted at Sree Balaji Medical College and hospital, Chennai to assess the rate of wound healing in patients using rh-EGF dressing.
In this study most patients belonged to the age group of 61-70 years in both the groups. The mean age of all the patients was 60.9 years. These findings are similar to the findings of studies conducted in India by experts [7] and studies conducted in other parts of the world by experts [8-10].
The sex distribution of the patients suffering from DM foot ulcer in this study was predominantly males (65%) as compared to the females (35%). These results are similar to the study conducted by experts [11] in which DM foot ulcer was significantly associated with male gender. The male to female ratio was 1.8:1 which is similar to the results of experts. They attributed this increased incidence in males due to largely indoor existence of females in the rural part of the country.
The most common site of ulcer in this study in the foot was in the plantar aspect (70%) as compared to the dorsal aspect (30%). These results were similar to the results in a study conducted by experts which showed majority of the ulcers developed in the plantar aspect of the foot [12]. This was mostly due to poor attention to the care of the foot, altered biomechanics and excessive or repeated pressure over the neuropathy affected areas of the foot.
In this study the major type of onset in both the groups was traumatic (68%) where the patient had a history of some type of trauma like RTA etc. which developed into a non healing DM foot ulcer. Rest other patients in both the groups had a spontaneous onset (32%) where they developed blister which broke to form ulcers or they may have had un-noticed small trauma.
Patient in this study used commonly used Insulin (71%) for diabetic control rather than OHA’s (29%) in both the groups.
The mean area of the ulcers under study at the start of the study was 34.29 cm2 (SD-8.4). At 1 week the mean percentage of area reduction is 10.21% (SD-1.7). At 2 weeks the mean percentage of area reduction is 26.77% (SD-2.61).
Similar results were found in the study conducted by experts who compared rh-EGF dressing with normal saline dressing [13]. Their study showed the patients who used rh-EGF dressing developed granulation tissue faster with increased rate of epithelisation and reduction in discharge when compared to the patients who used conventional normal saline dressing. Safety and efficacy of rh-EGF gel was evaluated by experts and it was found that the rate of healing was enhanced in patients using rh-EGF gel when compared to placebo [14]. These observations were similar to the present study. In a study conducted by experts, 90% of the study group which used rh-EGF gel showed decrease in wound soakage and size and increase in granulation tissue. Experts concluded in their study that wound closure in the rh-EGF group was significantly higher in comparison to the placebo group after 4 weeks [15,16]. Similar conclusions were drawn from the studies done by experts [17-20] rh-EGF enhanced wound healing significantly in patients suffering from venous ulcerations in the lower limb. Experts [21] studied that with rh-EGF concentrations of 1 and 5 µg/g rate of epithelisation were the fastest.
Overall, the use of rh-EGF dressing is found to increase the rate of healing in DM foot ulcer. In the study group, there were no observed adverse effects of this gel. And the literature has not documented any such side effects. Therefore, the morbidity and extended hospital stay needed for the treatment of DM foot ulcers may be minimised by the use of rh-EGF dressing. In addition to the different types of dressings, effective glycaemic control, pressure relief over the foot, suitable antibiotic therapy and proper debridement must be emphasised for enhancing the healing rate of the ulcers.
Conclusion
The rate of wound healing in diabetic foot ulcer patients using rh-EGF gel topical application was evaluated in this study. This rh-EGF gel topical application is a safe and effective form of dressing which facilitates granulation tissue formation epithelisation and wound healing.
References
- James RG, Alberti M, Mayer B, et al. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997; 20:1183-1197.
- Reiber GE, Ledoux WR. Epidemiology of Diabetic Foot Ulcers and Amputations: Evidence for Prevention. Evidence base diabetes care. 2002; 28:641-665.
- Raj CLR, Chand RA, Kumar S, et al. Management of Diabetic Foot Ulcer with Recombinant Human Epidermal Growth Factor Versus Conventional Dressing Method. J Evid Based Med Healthc 2019;6:2856-2860.
- Gluud C, Nicola S, Racines DS, et al. Growth Factors for Treating Diabetic Foot Ulcers. Cochrane Database Syst Rev 2015.
[Crossref] [Google Scholar] [Indexed]
- Vachhrajani V, Khakhkhar P. Growth Factors (Third Generation Wound Healing Agents) and Hormones. In Science of Wound Healing and Dressing Materials. 2020;113-118.
- Kateel R, et al. Clinical and microbiological profile of diabetic foot ulcer patients in a tertiary care hospital. Diab Met Syndr:Clin Res Rev. 2017.
[Crossref] [Google Scholar] [Indexed]
- Rangaswamy P, Rubby S, Prasanth K, et al. Prospective Study of Platelet Derived Growth Factor in Wound Healing of Diabetic Foot Ulcers in Indian Population. Int Surg J 2016;4:194-199.
- Yazdanpanah L, Shahbazian H, Nazari I, et al. Incidence and Risk Factors of Diabetic Foot Ulcer: A Population Based Diabetic Foot Cohort (ADFC Study)-Two-Year Follow-Up Study. Int J Endocrinol 2018;1-9.
[Crossref] [Google Scholar] [Indexed]
- Abdissa D, Adugna T, Gerema U, et al. Prevalence of Diabetic Foot Ulcer and Associated Factors among Adult Diabetic Patients on Follow-Up Clinic at Jimma Medical Center, Southwest Ethiopia. 2019: An Institutional Based Cross-Sectional Study. J Diabetes Res 2020; 1-6.
[Crossref] [Google Scholar] [Indexed]
- Banik PC, Barua L, Moniruzzaman M, et al. Risk of Diabetic Foot Ulcer and its Associated Factors Among Bangladeshi Subjects: A Multicentric Cross Sectional Study. BMJ Open 2020; 10:34058.
[Crossref] [Google Scholar] [Indexed]
- Bakri FG, Allan AH, Khader YS, et al. Prevalence of Diabetic Foot Ulcer and its Associated Risk Factors Among Diabetic Patients in Jordan. J Med J 2012;46:118-125.
- Galea AM, Springett K, Bungay H, et al. Incidence and location of Diabetic Foot Ulcer Recurrence. Diabetic Foot Ulcer 2009; 12:181-189.
- Raj RC, Chand AR, Kumar S, et al. Management of Diabetic Foot Ulcer with Recombinant Human Epidermal Growth Factor versus Conventional Dressing Method. J Evidence Based Med Healthcare 2019;6:2856-2860.
- Viswanathan V, Pendsey S, Sekar N, et al. A Phase iii Study to Evaluate the Safety and Efficacy of Recombinant Human Epidermal Growth Factor (Regen-DTm150) in Healing Diabetic Foot Ulcers. Wounds Compendium. Clin Res Practice 2006; 18:186-196.
- Singla S, Singla M, Kumar A, et al. Role of epidermal growth factor in healing of diabetic foot ulcers. Indian J Surg 2012; 74:451-455.
[Crossref] [Google Scholar] [Indexed]
- Afshari M, Larijani B, Fadayee M, et al. Efficacy of Topical Epidermal Growth Factor in Healing Diabetic Foot Ulcers. Therapy 2005; 2:759-765.
- Villa RG, Rebolledo FA, Platonoff AL, et al. Efficacy of Intralesional Recombinant Human Epidermal Growth Factor in Diabetic Foot Ulcers in Mexican Patients: A Randomized Double Blinded Controlled Trial. Wound Repair Regen 2014; 22:497-503.
[Crossref] [Google Scholar] [Indexed]
- Tsang MW, Wong WK, Hung CS, et al. Human Epidermal Growth Factor Enhances Healing of Diabetic Foot Ulcers. Diabetes Care 2003; 26:1856-1861.
[Crossref] [Google Scholar] [Indexed]
- Silva CMV, Iglesias ADT, Iglesias EG, et al. Granulation Response and Partial Wound Closure Predict Healing In Clinical Trials on Advanced Diabetes Foot Ulcers Treated With Recombinant Human Epidermal Growth Factor. Diabetes Care 2013; 36:210-215.
[Crossref] [Google Scholar] [Indexed]
- Falanga V, Eaglstein WH, Bucalo BB, et al. Topical Use of Human Recombinant Epidermal Growth Factor (h-EGF) in Venous Ulcers. J Dermatol Surg Oncol 1992; 18:604-606.
[Crossref] [Google Scholar] [Indexed]
- Hong JP, Kim YW, Jung HD, et al. The effect of Various Concentrations of Human Recombinant Epidermal Growth Factor on Split Thickness Skin Wounds. Int Wound J 2006; 3:123-130.
Author Info
Karan Kumar Jain*, Raghuram and Baskaran PK
Department of General Surgery, Sree Balaji Medical College and Hospital, Bharath University, Chennai, Tamil Nadu, IndiaCitation: Karan Kumar J, Raghuram, Baskaran PK. Assessment of Rate of Wound Healing in Patients using rh-EGF dressing for the Management of Diabetic Foot Ulcers. J Res Med Dent Sci, 2022, 10 (5):22-26.
Received: 23-Feb-2022, Manuscript No. 41493; , Pre QC No. 41493; Editor assigned: 25-Feb-2022, Pre QC No. 41493; Reviewed: 11-Mar-2022, QC No. 41493; Revised: 25-Apr-2022, Manuscript No. 41493; Published: 02-May-2022
