Research - (2021) Volume 9, Issue 2
Assessment of Mean Glandular Dose and Entrance Surface Dose in Mammography
Yousif M Abdallah3*, Nouf H Abuhadi1 and Hanan A. Aldousari2
*Correspondence: Yousif M Abdallah, Department of Radiological Science and Medical Imaging, College of Applied Medical Science, Majmaah University, Saudi Arabia, Email:
Abstract
X-ray diagnostic tests are important for public health. Such tests may involve significant patient irradiation and may be the population’s largest radiation source. X-ray mammograms show different female lesions using ionizing radiation. The result is exposure to a small amount of increased radiation. This study was performed during mammograms to determine the average absorbed dose of x-rays and factors influencing the breast 's median glandular dose (MGD). The study was conducted in Khartoum, Sudan, mammography patients. Sample size was 300 patients with different disease types. This study was in two Khartoum Hospitals. This study evaluated Robson’s Mean Glandular Dose (MGD) and additional mammographic dance tests. Patient age, breast thickness, tube filter and exposure factors (mAs and kVp) were study parameters. Calculated MGD results show that patient exposure was significantly lower than standard IAEA dose. For Craniocaudal and Oblique projections, the average MGD values were 1.54 + 0.17 (p<.05) and 1.58 + 0.22 (p<0.05). This study documented patient characteristics and radiation exposure factors. For international agencies (IAEA, NCRP and ACR), these results should be less than the standard dose.
Keywords
Mean Glandular Dose, Entrance, Mammography
Introduction
Mammography is an energy-saving process for human breast diagnostics and X-ray screening. By detecting different masses or micro calcifications, mammograms usually detect early breast cancer [1,2]. Mammograms, like any x-ray, use imageionizing radiation. Images are then analyzed for unusual results. Compared to bone radiation, less energy is often used, typically Mo and Rh. Ultrasound is generally used for further mass evaluation in mammography or palpable masses [3-5]. The breast is placed on a flat support plate during a mammogram and is coated with a parallel plate. An x-ray machine causes a slight explosion of rays passing through the breast to the opposite sensor [6,7]. The detector can be either a photographic film platform that captures an X-ray image or a solid-state sensor that transmits signals to a digital image computer. The pictures are called mammograms. Low density tissue (e.g. fat) appears transparent on a film mammogram (e.g. dense gray shadow approaching the darker background); whiter appears on a gray background, dense tissue area, e.g. connective and glandular or tumor. Standard mammograms are at the top and side of each breast, although the suspected breast area may be further investigated [8-10]. A mammogram will be carefully examined by a radiologist for areas of high density that appear differently from normal tissue or unusual configuration areas. Many types of anomalies, including cancer tumors, non-cancer masses known as benign tumors, fibro adenomas, or complex cysts, may occur in these areas. Radiologists analyze the unusual size, shape, contrast and appearance of the region at the edges of the area (i.e. cancer). They also look for small pieces of calcium that appear to be very bright spots on a mammogram called microcalcifications. Although a specific type of cancer is usually benign [11,12], it is sometimes seen at a microcalcification site. If a mammogram has one or more suspected noncancer areas, a radiologist may order another mammogram view, with or without additional magnification or compression. Another type of non-invasive imaging study may be conducted. Breast cancer is the most common form of cancer in women. It can often be treated if detected promptly. The diagnosis of cancer of the breast is based on mammography. X-ray radiation is a radiation ionizer that may increase the risk of cancer in patients [13-15]. Given that the GT (acinar, canal epithelium and stroma) is a radiosensitive organ [16], the risk of mammographic tissue damage is an important way to study it. Dosimetrics for boobs [17,18]. Average absorbed dose of central glandular breast tissue (MGD). The 2018 ICRP states that MGD is best suited to radiation risk in the breast under the European Protocol. MGD is the average energy that is deposited in all breast glandular tissues per unit mass of glandular tissue. The MGD assessment assumes that the breast tissue is homogeneous [19-21]. Due to the low risk of cancer, the energy absorbed by adipose tissues and skin is not included in the MGD calculation. According to ALARA, the total absorbed dose in the glandular tissue should be kept as low as possible [22,23]. The IAEA also recommends that the 50 per cent glandular tissue and 50 per cent compressed breast adipose MGD be less than 3.0 mGy [24,25].
Materials and Methods
In this study, an X-ray generator (SIEMENS, Mammomat 3000) with a 23-50 kV tube potential was used. 650 mm Film Focusing Distance (FFD) and 3 combinations of filter and anode: Molybdenum/molybdenum (Mo/ Mo). Automatic Exposure Management (AEC) feature used in routine mammographic testing. Automatic selection of an appropriate combination of anode/filter/tube based on pre-exposure compressed breast thickness correlated with the position of the plate compression. Four combinations of different anodine/filter/tube compressed breasts. Out of 45 standard films, 300 women have received 60 films in our study. Extra 60° films have been obtained to clarify suspected or indefinite focal lesions or microcalcifications. After informed consent, further oblique films have been made (we explained to our patients the potential benefit of early cancer detection versus a small carcinogenic risk related to the additional exposure).
The sample of the study
Samples ranged from 50.3+5.1 to 44-62 years of age (p>0.05) to 300 patients in age groups. Patients in this study were 40, ranging from 46 to 63 years of age. Women with breast implants, prior lumpectomy and radiation therapy were excluded from the study. Using a computer model, we generated data that can be calculated for a range of conditions for tube output and a half-value layer under clinical conditions.
Dose measurement methods
Using the computer model, we generated data to calculate the range of conditions for tube output and half-value layer under clinical conditions. The equations below are the same.
log 10 (ESAK)=nlog10(kV)+log10(A) (1)
HVL=a(kV)2+b(kV)+c (2)
Where calculated values for a, b, n calculated using tabulated values. We calculated mean glandular breast dose using Dance equation:
MGD=K•g (3)
Where the entry was K to the Air Kerma surface, and g was the HVL-dependent conversion factor, the breasts were 50 percent glandular/ adiposous.
MGD = K•g•c•s (4)
If K and g were the same as before, all 50 percent differences in breast composition were corrected by factor c and any difference in breast composition was rectified as the x-ray spectrum was used. Rh-Rh, Rh-Al and W-Rh are spectrum tables. A typical breast is calculated using the following formulation to calculate the glandular dose (GDD) equal to the PMMA thickness tested.
MGD = K•g•c•s (5)
When K comes in, Kerma (back-scatter) on the upper surface of PMMA is calculated. Factor g is 50 percent glandular, with typical breasts being between 50 and 64 c.
Results and Discussion
Test data analyzed to detect importance between breast thickness and dose in the window. In this study, Table 1 and Figure 1 shows the patients. At a 60 ° angle, the mean time product (mA) was substantially lower than the 45 ° angle in Table 2. The average kilovoltage, as shown in Table 2, was lower at 60-26.4 vs 28.4, p>0.05. The mean 60-angle exposure was significantly below 45 angles: 0.74 vs. 0.82, p<0.01, as shown in Table 2. A 45° versus 60° dose of craniocaudal projection was observed in Table 3. Table 4 shows the estimated corrections for ESAK (mGy), ESD(mGy), MGD(mGy) and breast thickness (cm). Due to the risk of breast-related carcinogenesis, the estimated glandular average dose (MGD) and input surface dose (ESD) have been assessed in recent years. The study was conducted in Khartoum Hospitals, Sudan to evaluate Robson's mean glandular dose (MGD) and extra mammography dance variables. Patient's age, breast thickness, tube destination filter and exposure factors (mAs and kVp) (Table 5).
| Characteristic | Value (N= 300) |
|---|---|
| Mean+ SD (range) | |
| Age (years) | 50.8+8.5 (45- 68) |
| 40-45 | 72 (24) |
| 46-50 | 120 (40) |
| 51-55 | 48 (16) |
| 56-60 | 42 (14) |
| 61-65 | 18 (6) |
| Breast thickness (cm) | 5.2+1.42 (4.2 -7.8) |
| Applied KVps | 28.6+5.3 (26-32) |
| Tube current (mAs) | 108.8+12.4 (100-126) |
Table 1: The characteristics of the sample.
| Characteristics | Craniocaudal projections | |
|---|---|---|
| 45º angle | 60º angle | |
| Mean ± SD (min.-max.) | Mean ± SD (min.-max.) | |
| breast thickness (cm) | 5.6 ±1.2 (4.7-6.7) | 5.1 ± 1.1 (4.8-5.8) |
| KVps | 27.4 ± 4.8 (26-31) | 28.4 ± 4.6 (27-31) |
| mAs | 114.8 ± 16.6 (110-122) | 112.4 ± 14.9) (110-121) |
| exposure | 0.82 ± 0.09 (0.57 -1.04) | 0.74 ± 0.08 (0.48-1.02) |
| Significance | P<0.05 | |
Table 2: The results of breast thickness, KVps, mAs and exposure in both Craniocaudal projections 45º and 60º angles, respectively.
| Characteristics | 45º angle | 60º angle |
|---|---|---|
| Mean ± SD (min.-max.) | Mean ± SD (min.-max.) | |
| Scale (0-3) | 1.86 ± 0.07 (0.87-2.32) | 1.84 ± 0.07 (0.84-2.40) |
| Contrast resolution | 1.92 ± 0.9 (0.9 -2.04) | 1.88 ± 0.9 (0.89-2.04) |
| Significance | P<0.05 | |
Table 3: The assessed image spatial resolution of craniocaudal projections (45° versus 60°).
| Measured dose | ESAK | ESD | MGD | Corrected breast thickness (cm) |
|---|---|---|---|---|
| 45º angle | 8.2 ± 3.3(7.5-9.1) | 9.2 ± 2.03 (8.4-9.7) | 1.5 ± 0.03(0.8-1.4) | 5.2 ± 1.1 (4.9-6.3) |
| 60º angle | 7.9 ± 3.1(6.7-9.9) | 8.9 ± 3.08 (7.5-9.7) | 1.4 ± 0.07 (0.7-1.7) | 5.1 ± 1.2 (4.7-6.4) |
Table 4: the estimated ESAK, ESD, MGD (mGy) and Corrected breastthickness (cm), respectively.
| Scientists | Sample size | Breast thickness (cm) | Conversion factors | MDG (mGy) |
|---|---|---|---|---|
| This study | 300 | 5.2 ± 1.42 (4.2 -7.8) | Dance [5] | 1.5 ± 0.3 |
| Abdallah and Mohamed [21] | 50 | 5.1 ± 0.1 | Rosen et al [1985] | 1.62 ± 0.5 |
| Whall and Roberts [23] | 130 | 5.5 ± 0.1 | Dance [5] | 2.0 ± 0.4 |
| Moran et al [26] | 345 | 5.2 ± 0.1 | Dance [5] | 0.4-5.4 |
| Bulling and Nicoll [3] | 310 | 4.9 ± 0.2 | Dance [5] | 0.7-8.5 |
| Klein et al. [19] | 1678 | 5.6 ± 0.2 | Klein et al [19] | 1.6 ± 0.6 |
| Dong et al. [8] | 120 | 3.7 ± 0.1 | Dance [5] | 1.7 |
Table 5: The measured dose of Craniocaudal projection 45° versus 60°.
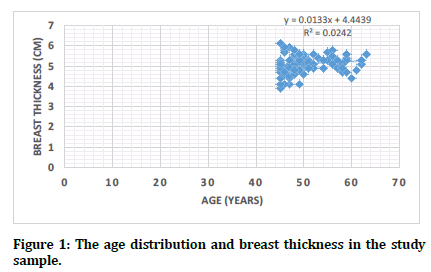
Figure 1. The age distribution and breast thickness in the study sample.
Discussion
All demographic data and exposures amount were documented. Then those amounts were compared with the similar international scholars results such as [3,8,19,21,26]. Some scientists reimbursed the tube current in the tabulated exposure equations. While other scientists compared fixed exposure factors with variable breast thickness. This study was revealed that estimated dose in mammography was lower than the other studies such as [3,8,19,21,23]. This study was revealed also that usage of W-RH target tubes can give higher dose MGD and ESAK, respectively. In this study the authors estimate that breast radiation exposure was recorded indirectly with study results corresponding to 60° film differences. The kVp fixed protocol was used in both studies: constant tube voltage, mAs for varying breast width. Dong et al. [8] examined the kVp dose for the kVp protocol and identified a lower dose of thicker bridle radiation when using the kVp protocol. However by reducing the patient dose, we used a fixed kVp protocol and believe this should not affect image quality. We conclude that 60° films were produced with more compression than 45°, resulting in less product time and exposure to the same or better visualization.
References
- Beckett JR, Kotre CJ. Dosimetric implications of age related glandular changes in screening mammography. Phys Med Biol 2000; 45:801.
- Bower MW, Hintenlang DE. The characterization of a commercial MOSFET dosimeter system for use in diagnostic x ray. Health Phys 1998; 75:197-204.
- Bulling SM, Nicoll JJ. Level and distribution of the radiation dose to the population from a mammography screening programme in New Zealand. Radiation Protection Dosimetry 1995; 57:455-458.
- Butson MJ, Rozenfeld A, Mathur JN, et al. A new radiotherapy surface dose detector: The MOSFET. Med Phys 1996; 23:655-658.
- Dance DR. Monte-carlo calculation of conversion factors for the estimation of mean glandular breast dose. Phys Med Biol 1990; 35:1211.
- Dance DR, Skinner CL, Carlsson GA. Breast dosimetry. Applied Radiation Isotopes 1999; 50:185-203.
- Dance DR, Skinner CL, Young KC, et al. Additional factors for the estimation of mean glandular breast dose using the UK mammography dosimetry protocol. Phys Med Biol 2000; 45:3225-3240.
- Dong SL, Chu TC, Lan GY, et al. Characterization of high-sensitivity metal oxide semiconductor field effect transistor dosimeters system and LiF: Mg, Cu, P thermoluminescence dosimeters for use in diagnostic radiology. App Radiation Isotopes 2002; 57:883-891.
- Faulkner K, Law J, Robson KJ. Assessment of mean glandular dose in mammography. Br J Radiol 1995; 68:877-881.
- Baek JE, Kang BJ, Kim SH, et al. Radiation dose affected by mammographic composition and breast size: First application of a radiation dose management system for full-field digital mammography in Korean women. World J Surg Oncol 2017; 15:38.
- Geeraertt N, Klausz R, Muller S. A large sample worldwide survey IAEA 2012. International conference on radiation protection in medicine, Bonn, Germany. CN-192 (7) 2012.
- Pasicz K, Fabiszewska E, Grabska I, et al. Mean glandular doses in mammography: A comparison of values displayed by a mammography unit with in-house values, both using the method proposed by Dance. J Radiol Protection 2016; 36:709.
- Gentry JR, DeWerd LA. TLD measurements of in vivo mammographic exposures and the calculated mean glandular dose across the United States. Med Phys 1996; 23:899-903.
- Stuhrmann M, Aronius R, Schietzel M. Tumor vascularity of breast lesions: potentials and limits of contrast-enhanced doppler sonography. Am J Roentgenol 2000; 175:1585-1589.
- Ries L, Melbert D, Krapcho M, et al. SEER cancer statistics review, 1975-2004, National Cancer Institute. Bethesda, MD.
- Soliman K, Bakkari M. Examination of the relevance of using radiochromic films in measuring entrance skin dose distribution in conventional digital mammography. Radiation Protection Dosimetry 2015; 165:373-375.
- Warren LM, Dance DR, Young KC. Radiation risk of breast screening in England with digital mammography. Br J Radiol 2016; 89:20150897.
- International Commission on Radiological Protection. Recommendations of international commission on radiological protection. ICRP Publication 20180
- https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/602233/Breast_screening_commission_and_test_small_field_mammography_ARCHIVED_22.03.2017.pdf
- Klein R, Aichinger H, Dierker J, et al. Determination of average glandular dose with modern mammography units for two large groups of patients. Phys Med Biol 1997; 42:651.
- Quach KY, Morales J, Butson MJ, et al. Measurement of radiotherapy x-ray skin dose on a chest wall phantom. Med Phys 2000; 27:1676-80.
- Behrouzkia Z, Zeinali A, Mohammady MH, et al. An investigation of mean glandular dose from routine mammography in Urmia, Northwestern Iran and the factors affecting it. Res J App Sci Eng Technol 2012; 4:3348-3353.
- Bor D, Tükel S, Olgar T, et al. Variations in breast doses for an automatic mammography unit. Diagnostic Interventional Radiol 2008; 14:122.
- Bosmans H, Marshall N. Radiation doses and risks associated with mammographic screening. Current Radiol Reports 2013; 1:30-38.
- Ciraj-Bjelac O, Rehani MM, Sim KH, et al. Risk for radiation-induced cataract for staff in interventional cardiology: Is there reason for concern? Catheterization Cardiovascular Interventions 2010; 76:826-834.
- Wambani JS, Korir GK, Shyanguya MN, et al. Assessment of patient doses during mammography practice at Kenyatta National Hospital. Breast Cancer Res 2011; 13:1-3.
Author Info
Yousif M Abdallah3*, Nouf H Abuhadi1 and Hanan A. Aldousari2
1Department of Radiological Science and Medical Imaging, College of Applied Medical Science, Majmaah University, 11952, Majmaah, Saudi Arabia2Department Diagnostic Radiology, College of Applied Medical Sciences, Jazan University, Jazan, Saudi Arabia
3Department of Medical Physics Jaber Alahmad Center for Molecular Imaging, Kuwait
Citation: Yousif M Abdallah, Nouf H Abuhadi, Hanan A Aldousari, Assessment of Mean Glandular Dose and Entrance Surface Dose in Mammographyts, J Res Med Dent Sci, 2021, 9 (2): 8-11.
Received: 03-Dec-2020 Accepted: 18-Jan-2021
