Research - (2021) Volume 9, Issue 8
Assessment of Knowledge, Attitude and Practices toward Infection Control Measures among Medical Students
Khaled Seetan1*, Sahem Ghraibeh1, Adel Alsharei1, Almuatasim Khamees1, Batool Alhasan1, Khayry Al-shami2, Hala Arabyat1 and Ali Guboug1
*Correspondence: Khaled Seetan, Department of Clinical Sciences, Faculty of Medicine, Yarmouk University, Jordan, Email:
Abstract
Background: Infection prevention and control (IPC) measures are essential to control healthcare-associated infections (HCAIs), which pose a significant risk for healthcare workers. Medical students have a significant role in applying IPC practices. This study evaluates medical students' knowledge and attitude in clinical years towards Jordan's IPC measures. Materials and methods: A cross-sectional survey was conducted to assess medical students' Knowledge and attitudes toward IPC measures in Jordanian medical schools. Students were selected using proportionate simple random sampling. An online questionnaire was sent to students, inquiring about students' knowledge and attitude were assessed using scores with a total of 24 and 12, respectively. Results: The study included 605 students, with a mean age of 22.2 ± 1.1 years, and an equal male: female ratio, 35.5%, 37%, and 27.4% of students were enrolled in the fourth, fifth, and sixth years, respectively Most students claimed good Knowledge about standard isolation protocols and showed good Knowledge about hand hygiene, cough etiquette and respiratory hygiene, and transmission of infections through hospital attire and equipment. A significant difference in attitude was noted between different genders, while both Knowledge and attitudes differed among different medical schools. Conclusion: Medical students showed variable Knowledge and attitudes towards infection prevention and control measures, with areas of good Knowledge and attitudes including cough etiquette, and respiratory hygiene, hand hygiene, infection transmission through hospital attire and equipment, while some misconceptions were noted regarding transmission and action against diseases such as HIV and TB.
Keywords
Infection prevention and control (IPC), Healthcare-associated infection (HCAI), Standard isolation precaution, Medical studentsIntroduction
Healthcare-associated infections (HCAIs) are considered a significant burden on public health, with the influence encompassing increased mortality and morbidity in both developing and developed countries, in addition to the increase in the length of hospital stay [1,2], and the emergence of multi-drug resistant strains of microorganisms [3], which all summit to the increase in health care costs.
HCAIs pose a significant risk to patients admitted to acute care health facilities, as 5-10% of them acquire an infection, while generally; one out of every 20 admitted patients develops an HCAI. Moreover, this risk is not only limited to patients but also extends to compromise health care workers (HCWs) and medical students, especially if there is a lack of adherence to infection prevention and control (IPC) precautions [4-6].
Infection prevention and control (IPC) precautions are essential in mitigating the spread of communicable diseases, and these measures are of utmost importance, especially in the era of COVID-19, which has mainly influenced many aspects of living. The influence of COVID-19 on students' education has been detrimental, with many measures being instituted to counteract adverse outcomes of the pandemic on education [7,8].
Compliance with IPC precautions and hand hygiene by health care workers and medical students has been shown to prevent and control HCAIs [9], and the benefits of these practices encompass more than just patients and their families, including HCWs and medical students [10].
Acquiring Knowledge about IPC during the undergraduate years of study is the optimal approach as medical students can apply the newly learned concepts and integrate them into their practice later on. However, explicit training targeting IPC is often lacking in most medical schools [11], which is worsened by the hectic schedules and congested curricula of medical schools [12].
In Jordan, the evidence is scarce on medical students' knowledge and attitudes, especially those in their clinical years of study towards IPCs. So, this study aims to reflect the level of awareness and attitudes of medical students studying in clinical yeas in Jordan regarding ICPs and assess the educational approaches adopted to improve students' awareness and attitudes.
Materials and Methods
A descriptive cross-sectional survey was conducted among medical students currently enrolled in Jordan's medical schools in their clinical years of study (fourth, fifth, and sixth years).
Proportionate simple random sampling was employed to select students in each medical school to participate in the study, and students were contacted via email after arranging with class representatives in each medical school. A total of 605 students enrolled in six medical schools returned the completed questionnaire and were included in the study.
Data was collected through an electronic questionnaire using the google forms service, which was emailed to the students. The questionnaire was adapted from a previous study conducted in a similar setting and modified by the author's accordingly [13] with the final questionnaire consisting of 28 items.
The questionnaire design aimed to cover areas of infection control guidelines, including hand hygiene, Knowledge about standard isolation precautions, respiratory hygiene, cough etiquette, use of personal protective equipment, cleaning and disinfection of medical equipment, and students' satisfaction with their IPC teaching and education.
Knowledge of the students was assessed through 14 items of the questionnaire, while items covering students' attitude comprised nine items. Knowledge and attitude scores were computed as correct answers were awarded a score of "1", and wrong answers were given a score of "0", with the highest possible knowledge and attitude scores 24 and 12.
Data were imported into Microsoft Excel sheet and then entered and analyzed using statistical package of social sciences (SPSS) version 25. Descriptive statistics were performed and expressed as means and standard deviations for continuous data, frequencies, and percentages for categorical data.
Students' knowledge and attitude scores were compared between different genders, medical schools, and years of study using independent-samples t-test and one-way analysis of variance (ANOVA).
Results
The study included 605 students with a mean age of 22.2 ± 1.1 years, with 304 (50.2%) males and 301 (49.8%) females. Students in the sixth year were 166 (27.4%), while those in the fourth and fifth year constituted 215 (35.5%), and 224 (37%) students, respectively.
Only 55 (8.8%) students reported a lack of awareness regarding standard isolation precautions within the health care setting and 466 (77%) students were aware that standard precautions apply to all patients regardless of their diagnosis.
Regarding hand hygiene, about two-thirds (66.6) of the students were exposed to hand hygiene training, although 453 (74.9%) students admitted that hand hygiene is part of the clinical training in hospitals and health centers, and the majority (92.7%) claimed to have sufficient Knowledge about hand hygiene.
However, only less than one-third (31.2%) recognized the minimum time needed for handwashing, while the majority (75.4%) of students correctly identified that micro-organisms are not destroyed by the use of clean water only (Table 1).
Table 1: Students’ responses to questions regarding standard precautions and hand hygiene.
| N | % | ||
|---|---|---|---|
| Are you aware of the standard isolation precautions within the health care setting? | No | 53 | 8.80% |
| Yes | 552 | 91.20% | |
| I was exposed to hand hygiene training | No | 202 | 33.40% |
| Yes | 403 | 66.60% | |
| I have sufficient knowledge about hand hygiene | No | 44 | 7.30% |
| Yes | 561 | 92.70% | |
| Hand hygiene is embedded in my clinical training in hospitals and health centers | No | 152 | 25.10% |
| Yes | 453 | 74.90% | |
| The minimum time needed for handwashing is: | 3 seconds | 5 | 0.80% |
| 10 seconds | 41 | 6.80% | |
| 15 seconds | 59 | 9.80% | |
| 20 seconds | 189 | 31.20% | |
| 30 seconds | 154 | 25.50% | |
| 60 seconds | 126 | 20.80% | |
| more than 60 seconds | 31 | 5.10% | |
| Micro-organisms are destroyed by using clean water | FALSE | 456 | 75.40% |
| TRUE | 77 | 12.70% | |
| Don't know | 72 | 11.90% | |
| Standard precautions apply to all patients regardless of their diagnosis. | FALSE | 83 | 13.70% |
| TRUE | 466 | 77.00% | |
| Don't know | 56 | 9.30% | |
Regarding Knowledge about communicable diseases transmission and prevention, the great majority of students (96.7%) reported that contaminated patientcare equipment results in an increased transmission risk of communicable diseases, and 563 (93.1%) students identified that medical equipment (syringes, needles, and catheters) are potential routes through which hospitalacquired infections can be transmitted.
However, only 100 (16.6%) correctly identified the definition of the term "nosocomial infection." Less than one-third (28.1%) were aware of HIV transmission odds after a single contaminated needle stick injury, and 234 (38.7%) students were aware that TB has the highest transmission rate via saliva (Table 2).
Table 2: Students’ responses to questions assessing knowledge about communicable diseases transmission.
| N | % | ||
|---|---|---|---|
| Does contaminated patient-care equipment result in an increased risk of communicable diseases? | No | 20 | 3.30% |
| Yes | 585 | 96.70% | |
| Which of the following has the highest rate of transmission via saliva? | Hepatitis B | 105 | 17.40% |
| Hepatitis C | 48 | 7.90% | |
| HIV | 90 | 14.90% | |
| TB | 234 | 38.70% | |
| Don't know | 128 | 21.20% | |
| Odds of HIV transmission after a single contaminated needle stick injury? | 0.1%-0.4% | 170 | 28.10% |
| 1%–4% | 195 | 32.20% | |
| 10%–40% | 164 | 27.10% | |
| 70%–90% | 76 | 12.60% | |
| Hospital acquired infection can be transmitted by medical equipment such as syringes, needles, catheters, stethoscopes, thermometers etc. | No | 26 | 4.30% |
| Yes | 563 | 93.10% | |
| Don't know | 16 | 2.60% | |
| Nosocomial infection is an infection that the patient comes with from home. | No | 454 | 75.20% |
| Yes | 100 | 16.60% | |
| Don't know | 50 | 8.30% | |
About half of the students (50.8%) knew that an N95 mask must not be thrown away after each use, while 250 (41.4%) were aware that a wet N95 mask could not be used; however, only 240 (39.7%), and 179 (29.6%) students correctly identified that an N95 mask can be reused if stored in a sealed plastic bag, and that mask fit test should be done at least once a year, respectively (Figure 1).
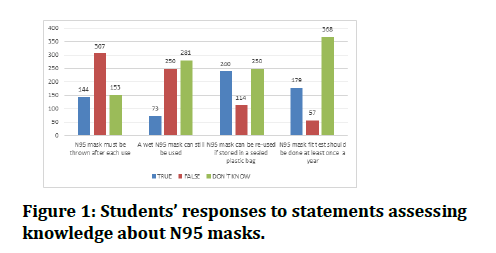
Figure 1: Students’ responses to statements assessing knowledge about N95 masks.
Additionally, most students were aware of the effect of wearing white coats or scrubs outside the hospital setting and jewelry, artificial nails, and neckties in the hospital setting.
Regarding respiratory hygiene and cough etiquette, a sizeable percentage of students endorsed the practice of coughing/sneezing on a disposable napkin (93.7%), or over the shoulder (63.8%), and keeping a distance of three feet from others when coughing (75.4%).
In comparison, 66.2% identified the practice of wiping hands on the inside of the white hospital coat after coughing/sneezing as false (Figure 2 and Table 3).
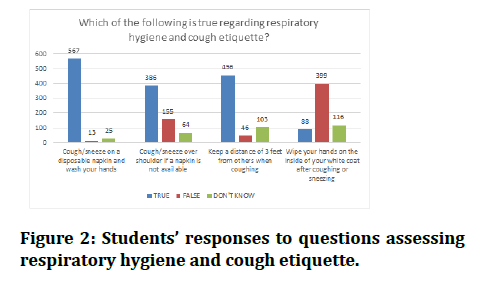
Figure 2: Students’ responses to questions assessing respiratory hygiene and cough etiquette.
Table 3: Students’ responses to questions assessing the risk of spread of diseases through cloths and accessories in the hospital setting.
| Strongly disagree | Disagree | Agree | Strongly agree | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| The following is associated with an increased risk for spread of diseases: | Wearing jewelry in a hospital setting | 56 | 9.30% | 172 | 28.40% | 267 | 44.10% | 110 | 18.20% |
| Wearing your white coat or scrubs outside the hospital setting (lunch, gym, home) | 53 | 8.80% | 65 | 10.70% | 193 | 31.90% | 294 | 48.60% | |
| Wearing artificial fingernails | 65 | 10.70% | 92 | 15.20% | 205 | 33.90% | 243 | 40.20% | |
| Wearing a necktie | 66 | 10.90% | 240 | 39.70% | 210 | 34.80% | 88 | 14.60% | |
When assessing students' attitudes toward infection control practices, 400 (66.1%) reported washing their hands before and after a patient encounter, 526 (86.9%) recognized the importance of hand washing even when gloves have been used, and 462 (76.4%) students reported that body fluids should not be handled with bare hands if gloves are not available. About two-thirds of students (65.5%) reported knowing or following strict infection control practices when dealing with TB patients, while only 63 (10.4%) would follow the correct immediate action of administering anti-HIV drugs in case of direct blood contact with an HIV patient. Moreover, 513 (84.8%) recognized their responsibility of complying with hospital-acquired infection guidelines (Table 4).
Table 4: Students’ responses to questions assessing attitudes toward infection control practices.
| N | % | ||
|---|---|---|---|
| Do you wash your hands before and after each patient encounter? | Yes | 400 | 66.10% |
| No | 31 | 5.10% | |
| Only after | 71 | 11.70% | |
| Only before | 3 | 0.50% | |
| Sometimes I forget | 100 | 16.50% | |
| Do you know or follow strict infection control practices when dealing with TB patients | No | 209 | 34.50% |
| Yes | 396 | 65.50% | |
| What immediate action should be taken in case of direct blood contact with an HIV patient? | Anti-HIV drugs | 63 | 10.40% |
| Anti-HIV immunoglobulins | 255 | 42.10% | |
| Blood tests | 111 | 18.30% | |
| don't know | 176 | 29.10% | |
| If there is limited beds available, patients with communicable diseases may be admitted in the same ward with other patients | FALSE | 435 | 71.90% |
| TRUE | 93 | 15.40% | |
| Don't know | 77 | 12.70% | |
| You can handle body fluids with bare hands if gloves are not available | FALSE | 462 | 76.40% |
| TRUE | 57 | 9.40% | |
| Don't know | 86 | 14.20% | |
| I do not have to wash hands if I used gloves | FALSE | 526 | 86.90% |
| TRUE | 46 | 7.60% | |
| Don't know | 33 | 5.50% | |
| It is not my responsibility to comply with hospital-acquired infection guidelines | FALSE | 513 | 84.80% |
| TRUE | 62 | 10.20% | |
| Don't know | 30 | 5.00% | |
| I feel that needles should be recapped after use and before disposal | FALSE | 141 | 23.30% |
| TRUE | 391 | 64.60% | |
| Don't know | 73 | 12.10% | |
Overall, the mean knowledge score of students was 13.9 ± 3.2 ranging from 6 to 23, with the knowledge score being significantly associated with students' medical college (p = 0.007). In contrast, the mean attitude score was 7.8 ± 1.8, ranging from 0 to 12, with a significant association with gender (p = 0.048) and medical college of students (p = 0.016) (Table 5).
Table 5: Knowledge and attitude scores of students towards infection prevention and control precautions.
| Knowledge score | Attitude score | ||||
|---|---|---|---|---|---|
| Mean (SD) | p (t/F) | Mean (SD) | p (t/F) | ||
| What is your gender? | Female | 14.1 (3.2) | 0.112 (1.6) | 8.0 (1.7) | 0.048* (2.0) |
| Male | 13.7 (3.2) | 7.7 (1.8) | |||
| In which medical ccollege do you study in Jordan? | AL-Balqa applied university | 13.6 (3.0) | 0.007* (3.25) | 7.6 (1.7) | 0.016* (2.8) |
| Hashemite University | 13.6 (3.0) | 7.5 (2.0) | |||
| Jordan University | 15.2 (3.1) | 8.4 (1.6) | |||
| Jordan University of Science and Technology | 13.63 (3.2) | 7.8 (1.7) | |||
| Mutah University | 13.7 (3.2) | 7.9 (2.2) | |||
| Yarmouk University | 14.0 (3.5) | 7.9 (1.6) | |||
| What is your year in medical school? | Fourth year | 13.8 (2.9) | 0.51 (0.67) | 7.7 (1.7) | 0.6 (0.51) |
| Fifth year | 13.8 (3.2) | 7.9 (1.9) | |||
| Sixth year | 14.1 (3.4) | 7.9 (1.7) | |||
| Total | 13.9 (3.2) | 7.8 (1.8) | |||
Discussions
This study presented an assessment of Jordanian medical students' knowledge, perception, and attitudes that are enrolled in clinical study years in medical school toward infection control measures and an overview of the educational approach taken toward infection control measures among medical students.
It is speculated that the nature of teaching IPC precautions that is dependent mainly on theoretical knowledge, on top of the demanding class schedule and the possibility of overlooking practical matters may lead to a lack of practice integration and critical thinking, which overall might affect the quality of the teaching process and learning by medical students [14] .A Japanese study conducted among nursing students showed that delivering a practical session in microbiology has significantly improved students' awareness of bacterial traits and infection spread [15].
Most of the students (91.2%) reported that they are aware of standard isolation precautions, and although self-reported awareness and actual knowledge and application may differ in students, this percentage is much higher than the self-reported rate among students in Qatar (48.4%) [13]. The finding consolidates this disparity between self-reported awareness and medical students' knowledge; fewer medical students reported correct responses to specific questions in hand hygiene, transmission of communicable diseases, and infection control measures.
Additionally, the timing during which this study is conducted is critical as the current COVID-19 pandemic should positively influence the knowledge and attitudes toward IPC measures among the population, especially healthcare-related personnel [7]. However, students still had several misconceptions regarding N95 masks and hand hygiene, while better knowledge was reported regarding respiratory hygiene, cough etiquette, and transmission of infections through hospital attire.
About one-third of the students reported not being exposed to hand hygiene training and that hand hygiene is not embedded in their clinical training. Nevertheless, most of the students (92.7%) claimed to have sufficient knowledge about hand hygiene, which is comparable to a medical student in Qatar [13], and slightly lower compared to findings among nursing students in Ireland16, considering that nearly all of their students (99%) have received hand hygiene training.
Medical students are at high risk of acquiring hepatitis B and HIV through their exposure to patients, possibly contaminated equipment, and the hospital environment. Therefore, adequate knowledge about these diseases is substantial in preventing transmission [17]. Only 170 (28.1%) were aware of the transmission rate of HIV following a contaminated needle stick injury, while 17.4% and 14.9% misidentified hepatitis B, and HIV, respectively, as having the highest rate of transmission via saliva, instead of Tuberculosis, which was identified by 38.7%. Additionally, worrying findings were observed as 34.5% did not know or follow strict infection control practices when dealing with TB patients, while only 10.4% were aware of the correct immediate action of administering anti-HIV drugs in case of direct blood contact with an HIV patient.
Female students showed slightly better attitude scores toward IPC precautions (p = 0.048) compared to males. In contrast, both knowledge and attitude of students differed significantly between students of various medical schools, as students enrolled in Jordan University recorded higher knowledge (0.007) and attitude (0.016) scores compared to students of other medical schools. Therefore a more extensive assessment of these medical schools' curricula and administrative measures to adopt the most optimum teaching methods and standardize learning tools that have been proven to be effective [18].
Conclusion
Medical students showed variable knowledge and attitudes towards infection prevention and control measures, with good knowledge and attitudes, including cough etiquette, respiratory hygiene, hand hygiene, and infection transmission through hospital attire and equipment. Simultaneously, some misconceptions were noted regarding transmission and action against diseases such as HIV and TB. Additionally, a significant difference in attitude was noted between different genders, while both knowledge and attitudes differed among different medical schools. A more thorough assessment of curricula and possible predictors of students' knowledge and attitudes is advocated, in addition to employing continuous measures to improve students' knowledge and attitudes.
References
- Zilberberg MD, Shorr AF. Economic aspects of preventing health care-associated infections in the intensive care unit. Crit Care Clin 2012; 28:89–97.
- Rosenthal VD, Guzman S, Migone O, et al. The attributable cost, length of hospital stay, and mortality of central line-associated bloodstream infection in intensive care departments in Argentina: A prospective, matched analysis. Am J Infect Control 2003; 31:475–480.
- Rosenthal VD, Maki DG, Mehta Y, et al. International nosocomial infection control consortiu (INICC) report, data summary of 43 countries 2007-2012. Device-associated module. Am J Infect Control 2014; 42:942–956.
- Ayub A, Goyal A, Kotwal A, et al. Infection control practices in health care: Teaching and learning requirements of medical undergraduates. Med J Armed Forces India 2013; 69:107–112.
- Roberts RR, Scott RD, Hota B, et al. Costs attributable to healthcare-acquired infection in hospitalized adults and a comparison of economic methods. Med Care 2010; 48:1026–1035.
- Vincent JL. Nosocomial infections in adult intensive-care units. Lancet 2003; 361:2068–2077.
- Norton EJ, Georgiou I, Fung A, et al. Personal protective equipment and infection prevention and control: a national survey of UK medical students and interim foundation doctors during the COVID-19 pandemic. J Public Health 2020.
- Fox MD, Bailey DC, Seamon MD, et al. Response to a COVID-19 outbreak on a university campus-Indiana, August 2020. Morb Mortal Wkly Rep 2021; 70:118–122.
- Clarke SP, Rockett JL, Sloane DM, et al. Organizational climate, staffing, and safety equipment as predictors of needlestick injuries and near-misses in hospital nurses. Am J Infect Control 2002; 30:207–216.
- Garner JS. Guideline for Isolation Precautions in Hospitals. Infect Control Hosp Epidemiol 1996; 17:53–80.
- Mary Rocha-Carneiro Garcia-Zapata, Adenícia Custódia Silva e Souza, Janaína Valadares Guimarães, et al. Standard precautions: Knowledge and practice among nursing and medical students in a teaching hospital in Brazil. Int J Infect Control 2010; 6:1.
- Melenhorst WB, Poos HP, Meessen NE. Medical students need more education on hygiene behavior. Am J Infect Control 2009; 37:868–869.
- Ibrahim AA, Elshafie SS. Knowledge, awareness, and attitude regarding infection prevention and control among medical students: A call for educational intervention. Adv Med Educ Pract 2016; 7:505–510.
- Kawashima A. Critical thinking integration into nursing education and practice in Japan views its reception from foreign-trained Japanese nursing educators. Contemp nurse a J Aust Nurs Prof 2003; 15:199–208.
- Yano R, Okubo T, Shimoda T, et al. A simple and short microbiology practical improves undergraduate nursing students' awareness of bacterial traits and ability to avoid spreading infections. BMC Med Educ 2019.
- Kingston LM, O'Connell NH, Dunne CP. Survey of attitudes and practices of Irish nursing students towards hand hygiene, including hand rubbing with alcohol-based hand rub. Nurse Educ Today 2017; 52:57–62.
- Khandelwal V, Khandelwal S, Gupta N, et al. Knowledge of hepatitis B virus infection and its control practices among dental students in an Indian city. Int J Adolesc Med Health 2018; 30:1–6.
- Nobile M, Agodi A, Barchitta M, et al. The effectiveness of educational interventions in university training on hospital hygiene: Results of action research. Ann diig 2018; 30:111–120.
Author Info
Khaled Seetan1*, Sahem Ghraibeh1, Adel Alsharei1, Almuatasim Khamees1, Batool Alhasan1, Khayry Al-shami2, Hala Arabyat1 and Ali Guboug1
1Department of Clinical Sciences, Faculty of Medicine, Yarmouk University, Irbid, Jordan2Jordan University Hospital, Amman, Jordan
Citation: Khaled Seetan, Sahem Ghraibeh, Adel Alsharei, Almuatasim Khamees, Batool Alhasan, Khayry Al-shami, Hala Arabyat, Ali Guboug,Assessment of Knowledge, Attitude and Practices toward Infection Control Measures among Medical Students, J Res Med Dent Sci, 2021, 9(8): 185-191
Received: 02-Aug-2021 Accepted: 17-Aug-2021
