Research Article - (2023) Volume 11, Issue 2
Apexogenesis of immature permanent molar using MTA with long term follow up : A case Report
*Correspondence: Esraa Jalal AlShareef, King Fahad armed hospital, Saudi Arabia, Email:
Abstract
The main purpose of treating an immature tooth with an open apex is to maintain vitality and continuity of normal root formation. Vital pulp therapy is aimed at maintaining the pulp's vitality, and dentinogenic potential, inducing complete root growth, formation of reparative dentin, thicker radicular dentin, and apical closure. This article presents the successful apexogenesis of the permanent immature molar of a 7-year-old girl using mineral trioxide aggregate and sodium hypochlorite irrigation and followed up for 4 years.
Keywords
Apexogenesis, Mineral trioxide aggregate, Pulp capping, Sodium hypochlorite, Vital pulp therapy
Introduction
The primary goal of treatment of an immature tooth with an open apex is to maintain the vitality and continuation of normal root formation [1,2]. Pulp capping, partial pulpotomy, and cervical pulpotomy are the different approaches of vital pulp therapy for an immature tooth that is subjected to trauma and deep caries [3,4]. Vital pulp therapy aims to preserve pulp vitality, dentinogenic ability of pulp, induce complete root formation, reparative dentin, thicker radicular dentin, and apical closure, achieve optimum crown-root ratio and enhance the integrity and strength of tooth structure that makes the tooth more resistant to fracture [5]. The pulp vitality, proprioception, and physical properties are diminished during conventional root canal treatment and therefore vital pulp therapy is preferred over root canal treatment [6-8]. Vital teeth have better moisture, and nourishment and withstand forces of mastication by 2.5 N greater than non-vital teeth. However, the fragility of immature teeth, difficulties in clinical and radiographic evaluations, complicated and lengthy procedures, high cost and pain are among the disadvantages of root canal treatment for immature teeth. Certain factors determine the success of vital pulp therapy such as case selection [9], treatment protocol, coronal seal, and clinical and radiographic assessment. The clinical assessment is essential to estimate the extent of pathological and degenerative changes of pulp [10]. At the same time, radiographic evaluation is essential to detect any pathological signs and the extent of root formation and closure. There are many materials used clinically for vital pulp therapy such as calcium hydroxide, glass ionomer, resin-modified glass ionomer, mineral trioxide aggregate (MTA), biological-based scaffolds, zinc oxide eugenol, calcium-enriched mixture, platelet-rich fibrin and triple antibiotic paste [11]. Nevertheless, MTA has shown dramatic success in vital pulp therapy [12]. MTA was approved by the American food and drug administration in 1998 as an obturating material [13,14]. Tricalcium silicate, tricalcium aluminate, tricalcium oxide silicate oxide and bismuth oxide are the main components of MTA [15]. Mineral trioxide aggregate is commonly applied for root perforation repair, apical barrier formation, and as a pulp capping material. Mineral trioxide aggregate is biocompatible, induces dentin formation, has high compressive strength, and possess superior marginal sealing ability [16]. Sodium hypochlorite is considered among the best irrigation agents, and it has good haemostatic properties and its influence on pulp survival range from moderate to high rate. The aim of the present article is to present a case report detailing the management and long-term follow-up of an immature first permanent molar using MTA in conjunction with sodium hypochlorite irrigation.
Case Report
Patient characteristics and chief complaint: A 7- year-old girl attended the dental clinic of paediatric dentistry department with lingering pain while drinking cold water, pain when biting and food impaction in the lower left posterior region. Her medical history was irrelevant. Regarding dental history, the patient discontinued her dental visits at the age of 5 after undergoing full mouth rehabilitation under general anaesthesia at a private clinic.
Clinical examination: Extra-oral examination revealed no signs of swelling or facial asymmetry. On intra-oral examination, the left permanent mandibular first molar had class I cavitated caries. The other permanent molars had superficial non- cavitated occlusal caries and the remaining permanent molars were symptoms free. The tooth in question had lingering response to the cold test (Endo Ice, Coltene/Whaledent Inc. Cuyahoga Falls, OH, USA) and there was no pain on percussion or palpation. An intra-oral periapical radiograph (IOPA) in relation to #36 was obtained, which showed deep occlusal caries and incompletely formed roots with open apices and thin radicular dentin, especially in the distal root (Figure 1).
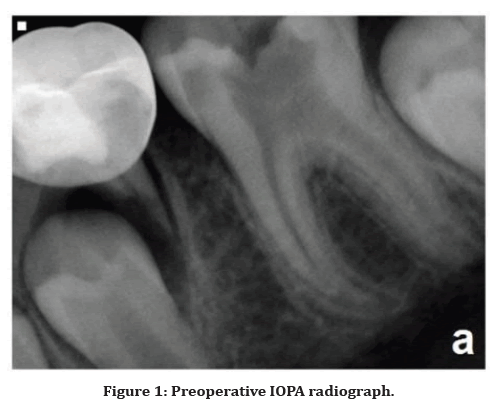
Figure 1. Preoperative IOPA radiograph.
Diagnosis and treatment planning: Based on the clinical and radiographic examinations, the patient had irreversible pulpitis in relation to tooth #36. After discussion with the parents, it was decided to do vital pulp therapy to promote apexogenesis followed by the placement of stainless steel crown. The parent signed the informed consent form before proceeding with the treatment.
Treatment
The tooth was isolated using a rubber dam after anesthetizing the inferior alveolar nerve and long buccal nerve using local anaesthesia. Next, the caries was removed by low-speed round carbide round bur (Hager & Meisinger GmbH, Neuss, Germany) with water coolant. Pulp was extirpated using a round and flame-shaped diamond bur and the extent of pulp tissue removal was determined by the extent of bleeding. After conventional pulpotomy was performed and hemostasis was achieved, sodium hypochlorite (NaOCL, 2.5%) was used for irrigating the pulp chamber. A 2-mm of pro root MTA (Dentsply Tulsa Dental Specialties, Johnson City, TN, USA) was condensed and applied. A cotton pellet was placed on top to allow MTA to reach the complete setting. The tooth was restored temporarily with glass ionomer cement (Ketac Fill, 3M Espe, St. Paul, MN, USA). Following restoration, the rubber dam was removed and the patient was discharged. During the follow-up visit after 10 days, the MTA had achieved a complete set and the patient did not show any pain or swelling. In the same session, the cotton pellet was removed and the cavity was filled with glass ionomer restoration and the tooth received a stainless steel crown. During the entire treatment procedure, the patient was cooperative.
Follow-up
Periodic periapical radiographs in addition to clinical examination were performed after 15 months (Figure 2a) with no abnormality detected. Then, the maintenance visits were discontinued for a year and 2 months due to COVID- 19 restrictions but still followed up via teledentistry. However, following the resumption of clinical visits post-COVID-19 restrictions, the tooth was followed up clinically and radiographically 30 months’ post- treatment (Figure 2b). The patient was recalled after 6-months from the last visit to replace the stainless steel crown as the mandibular permanent left first molar ends its active eruption stage and reaches its maximum intercuspation (Figure 2c). Finally, the last follow-up was performed 48 months after the actual treatment time. During this visit, the tooth had no clinical signs or symptoms such as swelling, pain, and abscess. The tooth achieved successful apexogenesis in length, and radicular dentin thickness especially in the distal root, apex closure, and dentinal bridge formed. No apical radiolucency was detected (Figure 2d).
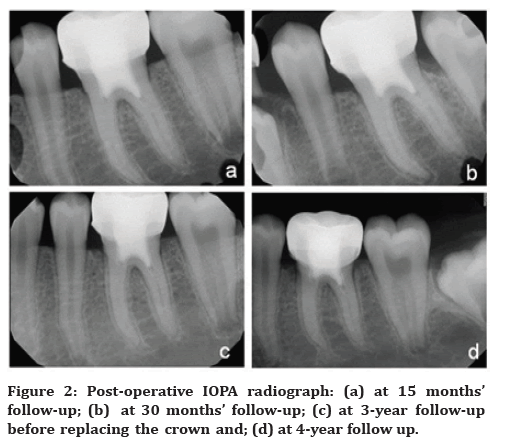
Figure 2. Post-operative IOPA radiograph: (a) at 15 months’ follow-up; (b) at 30 months’ follow-up; (c) at 3-year follow-up before replacing the crown and; (d) at 4-year follow up.
Discussion
The main goal of vital pulp therapy of immature teeth with open apex is to preserve pulp vitality and achieve apexogenesis when these teeth are subjected to trauma and deep caries. According to the American Academy of Paediatric Dentistry (AAPD), pulp capping, and partial or conventional pulpotomy are the treatment options to achieve apexogenesis for an immature tooth with an open apex [17]. The selection of partial or complete pulpotomy depends on the amount of inflamed and infected (diseased) pulp and the remaining healthy pulp. Mineral trioxide aggregate is a non-toxic, biocompatible material with pulp inductive ability to form hard tissue. MTA has an initial and post-setting pH of 10.2 and 12.5, respectively. It has an initial compressive strength of 40 MPa and reaches up to 67.3 to 70 MPa after final setting [18]. Due to setting expansion, MTA has excellent marginal adaptation and the setting is not interrupted by blood or water. When one of the major components of MTA, tricalcium oxide, is hydrated, it is converted to calcium hydroxide, which raises the pH of the material. Previous in-vitro studies have shown that MTA has antibacterial action against Enterococcus faecalis, Streptococcus sanguis, and other facultative species [19]. Mineral trioxide aggregate releases calcium and hydroxyl ions which destruct bacterial cell membrane and prevents bacterial replications through their action on bacterial DNA. Mineral trioxide aggregate has better physical properties and low solubility compared to calcium hydroxide. Furthermore, it shows less inflammation and better bridge formation than calcium hydroxide. The dentinal bridge formed by MTA is faster and better compared to calcium hydroxide [18]. The bridge formed by calcium hydroxide has tunnel defects in reparative dentin that may lead to bacterial micro leakage [3,7,12,16]. In addition, calcium hydroxide does not have bactericidal action on Enterococcus fecalis [7] and has a caustic effect on pulp [16]. Pro Root MTA was the first introduced MTA product in 1999 and has a long setting time of 2-3 hours [14,18]. A germ-free procedure is one of the important determinants of success in vital pulp therapy. The use of an aseptic procedure, rubber dam, is essential to achieve successful vital pulp therapy [7,9]. The diamond bur to amputate the pulpal tissue was selected to minimize pulpal bleeding as it cauterizes the tissue during cutting [14]. The hemostasis is critical for the success of vital pulp therapy [8,10,16,20]. In this study, sodium hypochlorite possessing antimicrobial and hemostatic properties was used as an irrigation solution [20,21]. Furthermore, NaOCL disinfects the dentin via saponification and chloramination actions on necrotic pulp tissue and collagen fibers causing disinfection and debridement of dentin [21]. A NaOCL (0.12% and 5.25%) concentration is used in direct pulp capping and vital pulp therapy. The coronal seal is another important factor to achieve successful vital pulp therapy [22,23] and in this study, the best coronal seal was achieved via the use of stainless steel crown and MTA. The present case was followed up for a total of 48 months. During all the followup visits, the tooth had no clinical signs or symptoms such as swelling, pain, and abscess.
Conclusion
The successful outcome of vital pulp therapy can be achieved by combining the best protocol in conjunction with ideal materials. Based on the outcome of the current treatment outcome, the treated tooth achieved successful apexogenesis in length, radicular dentin thickness, especially in the distal root, apex closure, and formation of the dentinal bridge. The selection of the best treatment protocol in conjunction with ideal materials provides satisfactory outcomes.
References
- Nabi S, Ajaz M, Khalid A, et al. MTA pulpotomy associated apexogenesis of human permanent molar with irreversible pulpitis: A case report. Int J Dent Health Sci 2015; 2:1389-1393.
- Sabbagh S, Sarraf Shirazi A, Eghbal MJ. Vital Pulp Therapy of a Symptomatic Immature Permanent Molar with Long-Term Success. Iran Endod J 2016; 11:347-349.
- Chandak M, Chandak M, Rathi C, Chandak P, Relan K. The Mineral Trioxide Aggregate in Vital Pulp Therapy of Permanent Teeth - A Systematic Review. J Evol Med Dent Sci 2021; 10:34-8.
- Van der Vyver P, Potgieter N, Selvan B. Apexogenesis treatment with mineral trioxide aggregate: long-term follow-up of two cases. S Afr Dent J 2018; 73:78-82.
- Murray PE. Review of guidance for the selection of regenerative endodontics, apexogenesis, apexification, pulpotomy, and other endodontic treatments for immature permanent teeth. Int Endod J 2022.
- Asgary S, Fazlyab M, Sabbagh S, et al. Outcomes of different vital pulp therapy techniques on symptomatic permanent teeth: a case series. Iran Endod J 2014;9:295-300.
- Hanna SN, Perez Alfayate R, Prichard J. Vital Pulp Therapy an Insight Over the Available Literature and Future Expectations. Eur Endod J 2020; 5:46-53.
- Taha NA, Ahmad MB, Ghanim A. Assessment of Mineral Trioxide Aggregate pulpotomy in mature permanent teeth with carious exposures. Int Endod J 2017; 50:117-25.
- Anu B, Yosef N. Vital Pulp Therapy Using MTA: A Case Series. Oral Health 2014; 70-4.
- Asgary S, Parhizkar A. Importance of 'Time' on 'Haemostasis' in Vital Pulp Therapy - Letter to the Editor. Eur Endod J 2021; 6:128-129.
- Chen Y, Chen X, Zhang Y, et al. Materials for pulpotomy in immature permanent teeth: a systematic review and meta-analysis. BMC Oral Health. 2019; 19: E227.
- Zhu C, Ju B, Ni R. Clinical outcome of direct pulp capping with MTA or calcium hydroxide: a systematic review and meta-analysis. Int J Clin Exp Med 2015; 8:17055-60.
- Malhotra N, Agarwal A, Mala K. Mineral trioxide aggregate: a review of physical properties. Compend Contin Educ Dent 2013; 34: E25-32.
- Tawil PZ, Duggan DJ, Galicia JC. Mineral Trioxide Aggregate (MTA): its history, composition, and clinical applications. Compend Contin Educ Dent 2015; 36:247-52.
- Rao A, Rao A, Shenoy R. Mineral trioxide aggregate--a review. J Clin Pediatr Dent 2009, 34:1-7.
- Qudeimat MA, Alyahya A, Hasan AA. Mineral trioxide aggregate pulpotomy for permanent molars with clinical signs indicative of irreversible pulpitis: a preliminary study. Int Endod J 2017; 50:126-34.
- American Academy of Pediatric Dentistry. Pulp Therapy for Primary and Immature Permanent Teeth. Pediatr Dent 2022; 415-423.
- Macwan C, Deshpande A. Mineral trioxide aggregate (MTA) in dentistry: A review of literature. J Oral Res Rev 2014; E6.
- Jain A, Gupta A, Agarwal R. Comparative evaluation of the antibacterial activity of two Biocompatible materials i.e. Biodentine and MTA when used as a direct pulp capping agent against streptococcus mutans and Enterococcus faecalis - An in vitro study. Endodontology. 2018; 30:66-8.
- George B. Clinical guidelines for vital pulp therapy. Endod Pract Today. 2019; 13:283–286.
- Machareonsap H, Chompu-inwai P, Manmontri C, et al. Which Irrigant Should be used for Vital Pulp Therapy in Permanent Teeth?- A Review of the Literature. Chiang Mai Dent J 2021; 42:20-31.
- Matsuo T, Nakanishi T, Shimizu H, Ebisu S. A clinical study of direct pulp capping applied to carious-exposed pulps. J Endod 1996; 22:551-556.
- Trope M: Regenerative potential of dental pulp. Pediatr Dent 2008, 30:206-210.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
King Fahad armed hospital, Saudi ArabiaCitation: Esraa Jala AlShareef. Apexogenesis of Immature Permanent Molar Using MTA with Long Term Follow Up: A Case Report J Res Med Dent Sci, 2023, 11[2]:29-31.
Received: 30-Jan-2023, Manuscript No. jrmds-23-88230; Accepted: 02-Feb-2023, Pre QC No. jrmds-23-88230; Editor assigned: 02-Feb-2023, Pre QC No. jrmds-23-88230; Reviewed: 16-Feb-2023, QC No. jrmds-23-88230; Revised: 21-Feb-2023, Manuscript No. jrmds-23-88230; Published: 28-Feb-2023
