Case Series - (2022) Volume 10, Issue 5
Adverse Cutaneous Drug ReactionsâCase Series
Sukanya M, Shreya Srinivasan, Nehete Sanket Sanjay* and Ashok kumar N
*Correspondence: Nehete Sanket Sanjay, Department of Dermatology, Venereology and Leprosy, Sree Balaji Medical College and Hospital, Chrompet, Chennai, India, Email:
Abstract
Adverse reactions are response to a drug in humans which are unintended and noxious which can occur at any dose or due to overuse, misuse or abuse of a drug. Severe form of adverse cutaneous reactions can represent variants of the same disease ranging from less severe Erythema Multiform to severe drug reactions like Stevens – Johnson Syndrome or Toxic Epidermal Necrosis. Here, we report 7 cases of various drug reactions.
Keywords
Adverse Cutaneous Drug Reaction, Fixed Drug Eruption, Stevens – Johnson Syndrome, Toxic Epidermal Necrosis
Introduction
Drug reactions range from nuisance maculopapular rash to rare and severe life threatening drug induced diseases [1]. Drug reactions may be only limited to the skin or may manifest a systemic reaction such as drug hypersensitivity syndrome or toxic epidermal Necrolysis. Thus for all cases of drug reactions, systematic approach is needed in management [2]. Here we present total 7 cases including fixed drug eruption (FDE), Erythema Multiform (EMF), Steven Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN).
Case Reports
Case 1: An 80-year-old female patient came with chief complaints of fluid filled itchy lesions over upper and lower limbs bilaterally since 2 weeks. History of fever 2 days prior for which intravenous medications were given. No mucosa involvement was seen. On examination, multiple tense blisters were present all over the body predominantly over limbs. (Figure 1) Multiple lesions with central pigmentation and surrounding pallor and erythema i.e., target lesions were seen. Few lesions were surrounded by multiple small vesicles. Diagnosis of Erythema Multiform Minor was made.
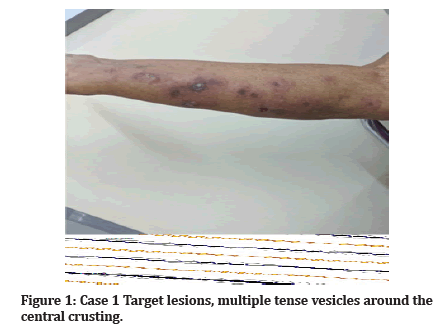
Figure 1: Case 1 Target lesions, multiple tense vesicles around the central crusting.
Case 2: A 60-year-old female patient came with complaints of multiple lesions with central pigmentation and surrounding erythema (Figure 2) since 10 days and redness of eyes since a week. History of over the counter use of Paracetamol for headache was present. On examination, multiple target lesions were seen all over the body. Non suppurating conjunctivitis was seen. No other mucosae were involved. Diagnosis of EM major was made.

Figure 2:Case 2 Target lesions.
Histopathology of both the cases of EM showed focal aggregates of apoptotic cells and interface dermatitis with perivascular inflammatory infiltrates.
Case 3: A 45-year-old female patient came with complaints of painful erosions of the buccal mucosa and lips (Figures 3 and 4) since 2 days and erythematous dusky red lesions over the face. History of intake of levofloxacin for lower respiratory tract infection was present. On examination, multiple dusky macules, patches were seen. Erosions over the lip and hard palate were seen. No lesions were seen elsewhere on the body. Diagnosis of SJS was made.
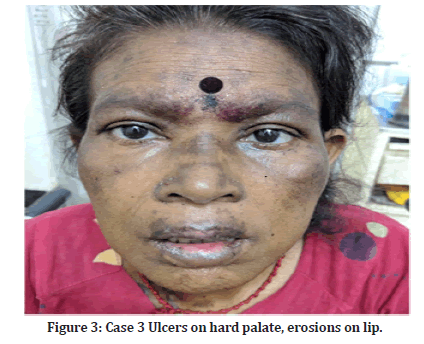
Figure 3:Case 3 Ulcers on hard palate, erosions on lip.
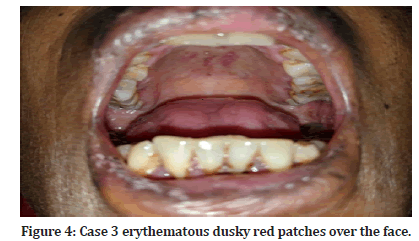
Figure 4:Case 3 erythematous dusky red patches over the face.
Case 4: A 55-year-old female came with complaints of diffuse erythematous rash over face, trunk, extremities and erosions over the lips (Figures 5 and 6) since 2 days. History of unknown antibiotics intake for last 5 days was present. On examination, multiple erythematous rashes with exfoliation of the skin at some areas were seen. Approximately 25% of body surface area was involved. Buccal mucosa and lips showed erosions. Diagnosis of SJS-TEN overlap was done.
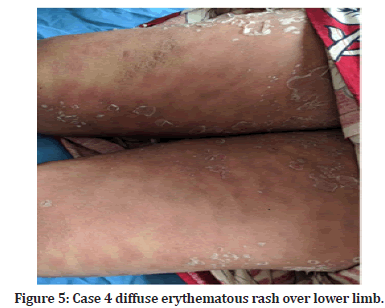
Figure 5:Case 4 diffuse erythematous rash over lower limb.

Figure 6:Case 4 erosions on lip.
Histopathology of both the cases of SJS and SJS-TEN showed necrosis of keratinocytes at all levels of the epidermis. Sub epidermal split is seen in the overlap case. Multiple eosinophils are seen in upper dermis.
Case 5: A 38-year-old male came with complaints of diffuse erythematous rashes since 1 day. It started as erythematous macule which later progressed into flaccid blisters following exfoliation of skin involving bilateral lower and upper limbs, back, and abdomen. He complained of painful erosions over the lips and buccal muscosa too. History of sudden onset of these lesions after dose of Trimethoprim-sulfamethoxazole was present. On examination, multiple eroded erythematous lesions with extensive detachments of skin (Figures 7 and 8) were seen. Few flaccid intact bullae over legs seen. Biopsy was done which showed diffuse necrosis of epidermis with sub epidermal split. Multiple eosinophilic infiltrates seem in upper dermis. Diagnosis of TEN was made.
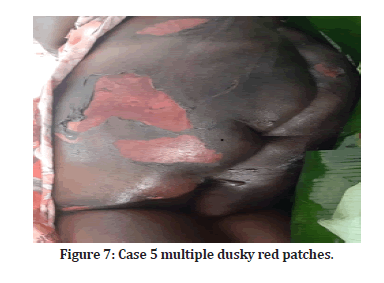
Figure 7:Case 5 multiple dusky red patches.
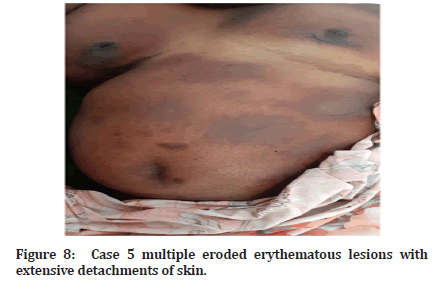
Figure 8:Case 5 multiple eroded erythematous lesions with extensive detachments of skin.
Case 6: A 28-year-old male came with chief complaints of multiple hyper pigmented erythematous patches (Figure 9) with burning sensation over trunk since 2 days. History of drug intake for abdominal pain was present. History of similar lesions at same sites 5 months back. On examination multiple hyper pigmented lesions were seen over the trunk. No mucosa involvement. Diagnosis of fixed drug eruption was made.
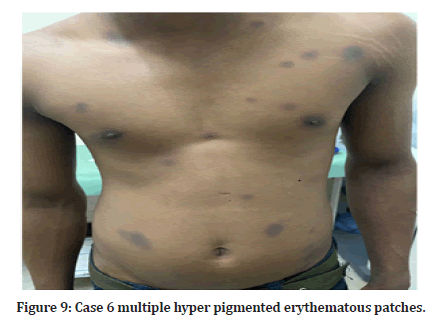
Figure 9:Case 6 multiple hyper pigmented erythematous patches.
Case 7: A 60-year-old male came with complaints of pigmented patches (Figure 10) with itching since 2 days on left forearm and on trunk. History of intake of diabetic drugs since 4 days was present. On examination, multiple hyper pigmented patches were seen over forearm and trunk. No mucosae were involved. Biopsy was done. Diagnosis of fixed drug eruption was made.

Figure 10:Case 7 multiple hyper pigmented erythematous patches.
Histopathology of both the cases of FDE showed hydropic degeneration of basal cell layer with pigmentary incontinence with multiple eosinophils in the upper dermis with lichenoid lymphocytic infiltrates (Figures 11 and 12).
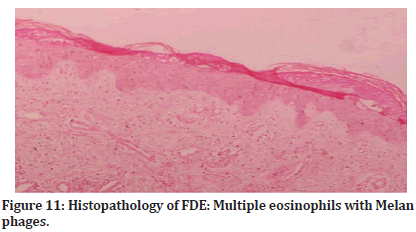
Figure 11:Histopathology of FDE: Multiple eosinophils with Melan phages.
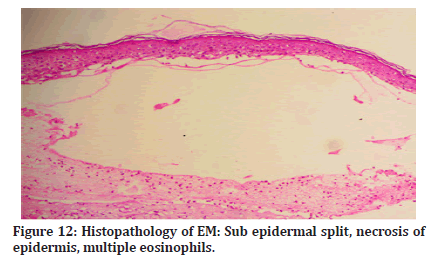
Figure 12:Histopathology of EM: Sub epidermal split, necrosis of epidermis, multiple eosinophils.
In all the cases, for management, after taken general measures like maintaining hemodynamics and serum electrolyte imbalance, offending drugs were stopped and short course of corticosteroids was given. Later, in severe cases, immunomodulatory drugs like cyclosporine were started.
Discussion
Adverse cutaneous drug reactions (ACDR) can clinically presented in different types. Morphologically it can be classified into: exanthemata’s, urticarial, pustular, bullous, papulosquamous, purpuric, lichenoid. The spectrum is vast including various entities like, FDE, EM, SJS, TEN, SJS-TEN overlap, acute generalized exanthematous pustulosis. Drugs can even precipitate several immuno bullous disorders. The drugs causing ADCR are antibiotics (sulfonamides, tetracyclines, beta lactams, NSAIDs, barbiturates, allopurinol.
Fixed drug eruption is a type of ACDR in which the lesions keep on recurring at the same site each time when particular offending drug is taken. The number of involved sites may increase over the time. Clinically it presents as purpuric, hyper pigmented, edematous patches or plaques anywhere on the skin or mucosae [1]. Sometimes flaccid bullae are also seen which rupture easily. On histopathology, superficial and deep interstitial and perivascular lymphocytes, eosinophils and neutrophilic infiltrate is seen. Extensive epidermal Necrolysis is also seen.
Erythema Multiform is an acute, self-limited skin disease characterized by abrupt onset of symmetric fixed erythematous papules which might evolve into typical or atypical target lesions. Typical target lesion is round, well defined lesion with central bulla or crust surrounding by pallor and dusky red halo [2]. It is mainly divided into EM major and EM minor depending on mucosal involvement. EM major is supposed to have severe mucosal involvement. Etiology for EM includes Herpes simplex virus, mycoplasma pneumoniae, histoplasma infection, exposure to poison ivy. Histopathology of early lesions show focal sites of apoptotic keratinocytes with an interface dermatitis and perivascular infiltrates and in late lesions, more confluent necrosis of keratinocytes is seen.
SJS and TEN are two rare, potentially fatal drug reactions which are characterized by erythema and tenderness followed by diffuse exfoliation. Both can involve mucosae [3]. The differentiation is done based on the body surface area (BSA) involved. If BSA is < 10 % then it is SJS, if 10-30% then SJS-TEN overlap and if >30% BSA is involved then it is TEN. Initial symptoms of both can be fever, burning eyes, pain on swallowing which can precede cutaneous manifestation by 2-3 days. Cutaneous features tend to appear first on trunk which later can progress to any area. Many times it starts with palm plantar involvement. They are characterized by painful, edematous dusky red patches with exfoliations. Pseudo nikolsky sign is positive. Various mucosae like buccal, ocular and genital and rarely respiratory mucosae can be involved. Systemic manifestations like fever, lymphadenopathy, hepatitis and cholestasis can be present. Prognostic scoring system for TEN known as SCORTEN is useful to check prognosis which include factors like age, heart rate, association with cancer, BSA, sr. urea level, Sr bicarbonate level, Serum glucose levels.
Histopathology shows single or clusters of apoptotic keratinocytes with subtle vacuolar degeneration of basal cell layer. Diffential diagnosis includes EM, generalized FDE and lupus erythematous.
In the management of all ACDR, after stopping the offending drug, hemodynamics and serum electrolytes levels are to be maintained. Short course of corticosteroids can be given followed by systemic drugs like IVIg, Cyclosporine, TNF alfa inhibitors, can be given according to the severity of the disease. FDE can be managed with topical corticosteroids. If infective etiology for EM is suspected, it should be treated first.
Conclusion
Drug reactions can range from harmless maculopapular rashes to fatal SJS/TEN. Thus systematic evaluation of the patient is compulsory. Thorough history taking is very important to make sure the causative drug is avoided later. Our case series shows how over the counter drugs also can cause cutaneous adverse drug reaction. Thus, more awareness regarding the use of over the counter drugs should be done.
References
- Bastuji-Garin S, Rzany B, Stern RS, et al. Clinical classification of cases of toxic epidermal Necrolysis, Stevens-Johnson syndrome, and erythema multiforme. Arch Dermatol 1993; 129:92-6.
- Khan DA, Solensky R. Drug allergy. J Allergy Clin Immunol 2010; 125:S126-37.
- Fouchard N, Bertocchi M, Roujeau JC, et al. SCORTEN: a severity-of-illness score for toxic epidermal necrolysis. J Investig Dermatol 2000; 115:149-53.
Indexed at, Google Scholar, Cross Ref
Author Info
Sukanya M, Shreya Srinivasan, Nehete Sanket Sanjay* and Ashok kumar N
Department of Dermatology, Venereology and Leprosy, Sree Balaji Medical College and Hospital, Chrompet, Chennai, IndiaCitation: Sukanya M, Shreya Srinivasan, Nehete Sanket Sanjay, Ashok kumar N, Adverse Cutaneous Drug Reactions – Case Series, J Res Med Dent Sci, 2022, 10 (5):32-35
Received: 01-May-2022, Manuscript No. JRMDS-22-41491; , Pre QC No. JRMDS-22-41491 (PQ); Editor assigned: 05-Mar-2022, Pre QC No. JRMDS-22-41491 (PQ); Reviewed: 17-May-2022, QC No. JRMDS-22-41491; Revised: 21-May-2022, Manuscript No. JRMDS-22-41491 (R); Published: 28-May-2022
