Research Article - (2022) Volume 10, Issue 5
Acute Intestinal Obstruction in Adults: Its Management and Outcome at Trihms, Naharlagun
Narayan Das*, Subu Sumpi and Rejum Ronya
*Correspondence: Narayan Das, Department of Surgery, Tomo Riba institute of Health and Medical sciences, Naharlagun, Arunachal Pradesh, India, Email:
Abstract
Background/Aims: Intestinal obstruction is a common surgical emergency and because of its serious nature, it demands
early diagnosis and speedy relief. Intestinal obstruction is responsible for approximately 20% of surgical admissions of
acute abdominal conditions. The objective of the study is to estimate the incidence of clinical presentation, etiology,
management and outcome of acute intestinal obstruction in adults at TRIHMS, Naharlagun.
Materials and methods: This was a prospective descriptive study of 41 patients presenting with symptoms and signs of acute
intestinal obstruction in the department of Surgery at TRIHMS, Naharlagun for a period of 10 months from 01-10-2020 to
31-07-2021. The diagnosis of acute intestinal obstruction was based on clinical history, physical findings, biochemical and
radiological investigations. Patients who met the inclusion criteria were included in this study. The treatment strategy was
planned ranging from conservative treatment to emergency laparotomy after resuscitation and rehydration of the patient.
Causes of obstruction, site of obstruction, and the operative procedure were recorded. Post-operative complications,
mortality and outcome were noted.
Results: Pain abdomen was the most common presenting symptom (95.12%) followed by vomiting (75.60%). The
commonest age group was from 18 years to 27 years (24.39%). Abdominal adhesions and bands was the most common
cause. Bowel resection and anastomosis was the commonest surgical procedure done in adults at TRIHMS.
Conclusion: Acute intestinal obstruction is a common surgical emergency and because of its serious nature, its demands
early diagnosis and speedy relief. Earlier diagnosis and timely intervention are associated with excellent outcome.
Keywords
Acute intestinal obstruction, Clinical presentation, Etiology, Management, Outcome
Introduction
Acute intestinal obstruction is a common surgical emergency and because of its serious nature, it demands early diagnosis and speedy relief. Intestinal obstruction may be classified clinically into two types:
Dynamic or mechanical, in which peristalsis is working against a mechanical obstruction. It may be classified clinically into two types:
- Small bowel obstruction-high or low.
- Large bowel obstruction.
- Adynamic or paralytic, in which there is no mechanical obstruction; peristalsis is absent or inadequate (e.g. paralytic ileus or pseudo-obstruction).
The nature of presentation will also be influenced by whether the presentation is:
- Acute (hours)
- Subacute (days)
- Acute on chronic
- Chronic (weeks)
Acute intestinal obstruction usually occurs in small bowel obstruction with sudden onset of severe colicky central abdominal pain, distension, and early vomiting and constipation. Presentation will be further influenced by whether the obstruction is:
- Simple-Where the blood supply is intact
- Strangulating/Strangulated-Where there is direct interference to blood flow, usually by hernia rings or intraperitoneal adhesions/bands.
The common causes of intestinal obstruction in Western countries and their relative frequency are shown as below (Figure 1) [1].
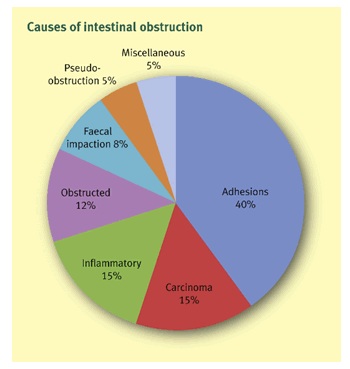
Figure 1: The common causes of intestinal obstruction in Western countries and their relative frequency are shown.
The present study aims to estimate the incidence of common clinical presentation, etiology, management and outcome of acute intestinal obstruction in adults at TRIHMS, Naharlagun.
Materials And Methods
This was a prospective descriptive study of 41 patients presenting with symptoms and signs of acute intestinal obstruction in adults in the department of Surgery at TRIHMS, Naharlagun during a period of 10 months from 01-10-2020 to 31-07-2021.
Inclusion criteria- Male and female- both gender of patients in the age group 18 years and above admitted in the department of surgery at TRIHMS and diagnosed as acute intestinal obstruction on the basis of history, clinical examination and radiological investigations.
- Address for surgical intervention at TRIHMS.
- Patients have given their consent for anesthesia for Surgery at TRIHMS.
- Patients admitted in the department of surgery at TRIHMS with acute abdominal causes other than acute intestinal obstruction.
- Patients with acute intestinal obstruction below the age group 18 years.
- Patients with acute intestinal obstruction not willing for surgery at TRIHMS.
A detailed history of all patients who met the inclusion criteria was taken and through clinical examination was done. Written consent was taken from study subjects or their relatives. Investigations of routine blood test include- HB%, TC, DC, ESR, Urine RE, X-ray abdomen, ultrasonography of abdomen/pelvis, CT scan of abdomen were performed. Preoperative management include nil orally, nasogastric aspiration, intravenous fluids and electrolytes, analgesic and antibiotics. All patients predicted to be having simple obstruction put on conservative management. Failure of relief of obstruction on this conservative treatment for more than 48 hours or development of signs of perforation/gangrene or strangulation was followed by laparotomy. Causes of obstruction, site of obstruction and the operative procedure done are recorded and biopsy was taken where required for histopathological confirmation. Post-operative complications, outcome and mortality are noted. The study was approved by the institutional ethical committee [2].
Results
A total of 41 patients admitted with acute intestinal obstruction in the department of surgery at TRIHMS, Naharlagun were included in the study (Table 1).
Table 1: Age and gender distribution of acute intestinal obstruction.
| Age in years | Number of patients | Percentage |
|---|---|---|
| 18-27 | 10 | 24.39 |
| 28-37 | 6 | 14.63 |
| 38-47 | 7 | 17 |
| 48-57 | 4 | 9.75 |
| 58-67 | 6 | 14.63 |
| 68-77 | 8 | 19.51 |
| Total | 41 | 100 |
| Male patients | 24 | 58.53 |
| Female patients | 17 | 41.47 |
The most common age group was between 18 and 27 years followed by 68 and 77 years. The younger patient was 18 years of age and the eldest patient was 77 years. The mean age of incidence was 44.05 years.
There was 24 (58.53%) of males and 17 (41.47%) of female patients in this study. Male patients were more commonly affected compared to females (Table 2).
Table 2: Incidence of previous abdominal surgery and site of obstruction.
| Site of intestinal obstruction | Number of patients | Percentage |
|---|---|---|
| Small bowel obstruction (SBO) | 32 | 78.05 |
| Large bowel obstruction (LBO) | 9 | 21.95 |
| Total | 41 | 100 |
| History of previous abdominal operation | 6 | 14.63 |
| No history of previous abdominal operation | 35 | 85.37 |
There were 32 patients (78.05%) of obstruction in the small bowel and 9 patients (21.95%) of obstruction in the large bowel in the study. There was history of previous abdominal surgery in 14.63% of cases in the study (Table 3).
Table 3: Clinical features.
| Clinical features | Number of patients | Percentage |
|---|---|---|
| Abdominal pain | 39 | 95.12 |
| Vomiting | 31 | 75.6 |
| Abdominal distension | 25 | 60 |
| Constipation | 13 | 54 |
The most common clinical feature was abdominal pain (95.12%), vomiting (75.60%), abdominal distension (60%) and constipation (54%) of cases in this study (Table 4).
Table 4: Etiology of intestinal obstruction.
| Etiology | Number of patients | Percentage |
|---|---|---|
| Abdominal adhesions and bands | 21 | 51.21 |
| Hernia | 2 | 4.88 |
| Intestinal tuberculosis | 3 | 7.31 |
| Intussusception | 3 | 7.31 |
| Malignancy | 8 | 19.51 |
| Meckel’s diverticulosis | 1 | 2.44 |
| Impacted hard stool | 1 | 2.44 |
| Trichobezoar | 1 | 2.44 |
| Inflammatory bowel disease( crohn’s disease) | 1 | 2.44 |
| Total | 41 | 100 |
Abdominal adhesions and bands (51.21%) and malignancy (19.51%) were the most common causes of intestinal obstruction in this study (Table 5).
Table 5: Management option of intestinal obstruction.
| Management option | Number of patients | Percentage |
|---|---|---|
| Conservative management | 14 | 34.14 |
| Surgical management | 27 | 65.86 |
| Total | 41 | 100 |
| Surgical procedure | Number of patients | Percentage |
| Adhesiolysis and release of bands | 9 | 33.33 |
| Resection of bowel and anastomosis | 12 | 44.44 |
| Repair of hernia | 2 | 7.4 |
| Ostomy | 3 | 11.11 |
| Other | 1 | 3.7 |
In this study, 27 (65.86%) patients require surgical intervention and 34.14% of cases response to conservative treatment of intestinal obstruction in adults. Resection of bowel and anastomosis (44.44%) and adhesion lysis and release of bands (33.33%) were the common surgical procedures in the study (Table 6).
Table 6: Outcome.
| Outcome | Number of patients | Percentage |
|---|---|---|
| Uneventful recovery | 33 | 80.48 |
| Morbidity | 7 | 17.07 |
| Mortality | 1 | 2.43 |
Most of the patients recovered without any complications (80.48%). Infection was the major cause of morbidity (17.07%) and there was 2.43% of mortality in this study
Discussion
Acute intestinal obstruction is a common surgical problem and is associated with significant morbidity and mortality. Intestinal obstruction is responsible for approximately 20% of surgical admissions of acute abdominal conditions [3]. The small bowel is a site of obstruction in 60-80% of cases. The commonest cause of small bowel obstruction is adhesions, usually secondary to prior abdominal operations. The other common causes are neoplasms and incarceration in hernia. All three combined account for 70-80% of all cases of small bowel obstruction. The other causes of small bowel obstruction include tuberculosis of intestine, Crohn’s disease, and strictures secondary to ischaemia, radiation injury, intussusception or inflammation [4]. More generally, the etiology of SBO can be considered in term of the underlying abnormality (a) Mechanical obstruction or (b) Paralytic obstruction.
The cardinal features of acute intestinal obstruction include- acute abdominal pain, distension, vomiting and constipation. Although symptoms of Small Bowel Obstruction(SBO) and Large Bowel Obstruction (LBO) are similar, etiologies, diagnostic approach and therapeutic considerations are quite different. Sources of acute LBO can be separated into mechanical (Colorectal Carcinoma (CRC) (50-80%)), diverticulitis, volvulus, fecal impaction, Inflammatory Bowel Disease (IBD) and non-mechanical causes (acute colonic pseudo-obstruction [5]. In the diagnosis of intestinal obstruction, the important elements to obtain in history include prior abdominal operations (suggesting the presence of adhesions) and the presence of abdominal disorders (e.g. intra-abdominal cancer or inflammatory bowel disease). On examination, a meticulous search for hernias (particularly in the inguinal and femoral regions) should be conducted. The stool should be cheeked for gross or occult blood, the presence of which is suggestive of intestinal strangulation. In the blood tests the white cell count is important to identify the deteriorating patient-while this may initially be normal or slightly raised, marked elevation suggests infarction and perforation. Careful monitoring of renal function is essential, with daily or even twice daily biochemistry.
Gastrointestinal fluid losses deplete sodium and chloride levels, which will need correction. The diagnosis of SBO is usually confirmed with radiographic examination. The abdominal series consists of a radiograph of the abdomen with the patient in a supine position, a radiograph of the abdomen with the patient in an upright position, and a radiograph of the chest with the patient in an upright position. The finding most specific for SBO is the triad of dilated small bowel loops (>3 cm in diameter), air-fluid levels seen on upright films, and a paucity of air in the colon. The sensitivity of abdominal radiographs in the detection of SBO ranges from 70 to 80% [6]. Computed Tomography (CT) Scanning is 80 to 90% sensitive and 70 to 90% specific in the detection of SBO. CT scan helps identify the exact location of colonic and other intra-abdominal malignancies, their extent, presence of metastatic disease and other organ involvement. Ultrasonography- presence of abundant gas in the bowel limits its use in bowel obstruction. It can delineate, fluid filled loops, extra luminal fluid. It is helpful in differentiating mechanical SBO from paralytic ileus by detection of peristalsis [7]. It is useful in pregnant women since there is no risk of radiation exposure. Endoscopy Endoscopic evaluation can be both diagnostic and therapeutic in LBO. Insufflation during endoscopy can lead to perforation and is generally contraindicated in cases where acute LBO is already suspected. The cardinal features of acute intestinal obstruction include- abdominal pain, distension, vomiting and absolute constipation [8].
Table 7: The studies of clinical features by various authors are as follows.
| Authors | Year | No. of patients | Pain of abdomen | Vomiting | Distension of abdomen | Constipation |
|---|---|---|---|---|---|---|
| J.S. Khan et al. | 2007 | 100 | 1 | 0.92 | 0.97 | 0.91 |
| S. Adhikari et al. | 2010 |
367 |
0.72 |
0.91 |
0.93 |
0.82 |
| A. M. malik et al. | 2010 | 229 | 0.75 | 0.73 | 0.87 | 0.88 |
| T. Deepak et al. | 2014 | 50 | 0.88 | 0.78 | 0.66 | 0.54 |
| P.B. Ooko et al. | 2015 | 445 | 0.894 | 0.78 | 0.654 | 0.508 |
| S.B. Priscilla et al. | 2017 | 100 | 0.94 | 0.69 | 0.52 | 0.58 |
| Present study | 2021 | 41 | 0.9512 | 0.756 | 0.6 | 0.54 |
There are three main measures used to treat acute intestinal obstruction (i) Gastrointestinal drainage via nasogastric tube, (ii) Fluid and electrolyte replacement and (iii) Relief of obstruction, usually by operation. Surgical treatment is necessary for most cases of intestinal obstruction but should be delayed until resuscitation is complete, provided there is no sign of strangulation or evidence of closed-loop obstruction. The three principles of surgical intervention are-management of: (i) The segment of the site of obstruct ion, (ii) The distended proximal bowel and (iii) The underlying cause of obstruction. The timing of surgical intervention is dependent on the clinical picture. The classic clinical advice that “the Sun should not both rise and set” on a case of unrelieved acute intestinal obstruction is sound and should be followed unless there are positive reasons for delay [9].
The most common age group was between 18 to 27 years followed by 68 to 77 years in this study. In this study of 41 patients with acute intestinal obstruction, 58.53% were males and 41.47% were females which are consistent with gender incidence of the similar study conducted by 2000. In this study, the site of obstruction was small intestine in 78.05% and large bowel in 21.95% of cases which was comparable to the study conducted by 2017. In this study, the most clinical feature was abdominal pain (95.12%) followed by vomiting (75.60%), abdominal distension (60%) and constipation in 54% of cases which was comparable to the study conducted by 2010 [10].
In this study, the common causes of acute intestinal obstruction were abdominal adhesions and bands (51.21%) followed by malignancy of instestine in 19.51% of cases. The study conducted by 2013 and reported adhesions in 40%, malignancy in 14% and obstructed hernia in 30% of cases. Although the incidence of obstructed/strangulated hernia is more in the developing countries, but in our study only 4.88% cases due to hernia. It may be because of the awareness of public, the availability of surgical facilities in the periphery for the hernia repair, the hernias are treated early. In this study, 34% of patient’s response in conservative treatment, but AM Malik et al. reported that 76% of patients responded in conservative treatment [11].
In this study, the most common surgical procedures were bowel resection and anastomosis (44.44%) followed by ostomy in 11.11% of cases, but PB Ooka et al. reported resection and anastomosis of bowel in 47.10% and adhesiolysis in 14.10% of patients in their study [12]. Outcome- most of the patients recovered without any complications (80.48%). Infection was the major cause of morbidity (17.07%) and mortality was 2.43% in this study. SB Pricilla et al. reported 76% of patients recovered without any complications, morbidity mainly wound infection in 18% and mortality in 6% of cases. PB Ooka et al. reported that overall morbidity and mortality rates were 15% and 4.5% respectively in their study [13].
Conclusion
Acute intestinal obstruction is a common surgical emergency and can arise from a wide range of etiologies. It is important that all potential diagnoses are considered and that active management and resuscitation is commenced early. Those patients managed non-operatively need close ongoing assessment. The operative management continues to evolve towards single- stage procedures; however, the patient’s physiology should be taken into account when planning surgical procedures.
References
- Williams NS, Bulstrode CJK, O’Connell PR, et al. Intestinal obstruction. Baily Love Short pract Surg 2013; 70:1181-1198.
[Google Scholar] [Pubmed]
- Kukor JS, Dent TC, Nelson RL, et al. Small intestinal obstruction. In; surgery of the Small intestine. Norw Appl Lange 1987; 267-282
[Crossref] [Google Scholar] [Pubmed].
- Palanivelu C. Laparoscopy in small bowel obstruction. Art Laparo Surg 2007; 59:971-988. [Crossref]
[Google Scholar] [Pubmed]
- Brooks A, Bryan AC, Negel T, et al. Small bowel obstruction. Emer Surg 2010; 14:74-91.
- Maglinte DD, Heitkamp DE, Howard TJ, et al. Currents concepts in imaging of small bowel obstruction. Radiol Clin North Am 2003; 41:263-69.
[Crossref] [Google Scholar] [Pubmed].
- Suri S, Gupta S, Sudhakar PJ, et al. Comparative evaluation of plain films, Ultrasound and CT in the diagnosis of intestinal obstruction. Acta Radiol 1999; 40:422-28.
[Crossref] [Google Scholar] [Pubmed]
- Ogata M, Mateer JR, Condon RE, et al. Prospective evaluation of abdominal Sonography for the diagnosis of bowel obstruction. Ann Surg 1996; 223:237-41.
[Crossref] [Google Scholar] [Pubmed]
- Khan JS, Alam J, Hassan, et al. Pattern of intestinal obstruction a hospital based study. Pak Armed Forces Med J 2007; 57:295-299. [Crossref]
[Google Scholar] [Pubmed]
- Adikari S, Hossen MZ, Das A, et al. Etiology and outcome of acute intestinal obstruction. A review of 367 patients in Eastern India. Saudi J Gastroenterol 2010; 16:285-287.
[Crossref] [Google Scholar] [Pubmed]
- Malik AM, Shah M, Pathan R, et al. Pattern of acute intestinal obstruction: Is There a change in the underlying etiology? Saudi J Gastroenterol 2010; 16:272-74.
[Crossref] [Google Scholar] [Pubmed]
- Thampi D, Tukka VN, Bhlki N Sreekanta, et al. A clinical study of surgical management of acute intestinal obstruction. Int J Res Health Sci 2014; 2:299-308. [Crossref]
[Google Scholar] [Pubmed]
- Ooko PB, Sirera B,Saruni S, et al. pattern of adult intestinal obstruction at Tenwek hospital, in south-western kenya. Pan African Med J 2015; 20:31.
[Crossref] [Google Scholar] [Pubmed]
- Priscilla SB, Edwin IA, Kumar K, et al. A clinical study on acute intestinal obstruction. Int J SCi Stud 2017; 5:107-110. [Crossref]
[Google Scholar] [Pubmed]
Author Info
Narayan Das*, Subu Sumpi and Rejum Ronya
1Department of Surgery, Tomo Riba institute of Health and Medical sciences, Naharlagun, Arunachal Pradesh, IndiaCitation: Narayan Das, Subu Sumpi, Rejum Ronya, AAcute Intestinal Obstruction in Adults: Its Management and Outcome at Trihms, Naharlagun , J Res Med Dent Sci, 2022, 10(5): 129-133.
Received: 21-Feb-2022, Manuscript No. 48668; , Pre QC No. 48668; Editor assigned: 23-Feb-2022, Pre QC No. 48668; Reviewed: 09-Mar-2022, QC No. 48668; Revised: 22-Apr-2022, Manuscript No. 48668; Published: 09-May-2022
