Research - (2022) Volume 10, Issue 9
A YOUNG FEMALE WITH SEVERE FATIGUE
Kosuri Akhila*, Suresh Kanna S, Goutham Kumar AP, Keerthana I and Kunduru Dinesh Reddy
*Correspondence: Kosuri Akhila, Department of General Medicine, Sree Balaji Medical College and Hospital, India, Email:
Abstract
Rare clinical illness known as Plummer-Vinson syndrome manifests as a triad of symptoms including difficulty swallowing, anaemia, and esophageal webs. Plummer-Vinson syndrome is characterized by the presence of thin mucosal folds known as oesophageal webs, which are best, visualized in lateral views during barium, swallow or during an Oesophagoscopy procedure. It has been found that people with Plummer Vinson syndrome are more likely to develop squamous cell carcinoma of the pharynx and proximal oesophagus. This is a case of 27 year old female who was hospitalized in our hospital with fatiguability and giddiness. An Upper gastrointestinal intestinal endoscopy shows cricopharygeal webs, linear furrows and exudates in distal esophagus. Bougie dilatation was done and tissue sent for biopsy which showed reflux esophagitis, indicating Plummer Vinson syndrome.
Keywords
Plummer vinson syndrome, Dysphagia, anaemia, Oesophageal webs
Case Presentation
Plummer-vinson syndrome [1] is most commonly seen in white women, thin built, 4th to 5th decade of life. Rare in men. The triad of dysphagia, anaemia from iron deficiency, and oesophageal webs [2] in the postcricoid area is diagnostic of Plummer-vinson syndrome. Plummer-Vinson syndrome has a mysterious backstory. Iron deficiency anaemia is a major etiological cause; malnutrition, genetic predisposition, and autoimmune mechanisms also play a role.
Two doctors, Henry Stanley Plummer and Porter paisley Vinson, are credited with the identification of this condition. As a result of its association with two British laryngologists, the syndrome has been given their names: Paterson- Brown-Kelly syndrome and Donald Ross Paterson-Adam Brown Kelly syndrome. As far as we know, Dr. Paterson was the first medical professional to indicate a link between Plummer-Vinson syndrome and carcinoma.
Case Report
A 27yr old female came to the hospital with c/o fatiguability and giddiness for 2months.She also had complaints of difficulty in swallowing since 1month first to solid foods then gradually developed difficulty in swallowing to semisolid foods. She also had complained of breathlessness on exertion. On general examination, patient was conscious, oriented, afebrile, pulse rate 102/ min, blood pressure 110/70mmHg. On examination pallor is present and no icterus, Pedal edema present and JVP rose. Cardiovascular, respiratory, abdominal, neurological examinations were normal.
All necessary investigations were done and showed haemoglobin of 6.1gm/dl, MCV 55.6fl, MCH 15.7pg, MCHC 28.2% WBC and platelet count was normal. Iron studies were suggestive of iron deficiency anaemia. Liver function tests and renal function tests were normal. 1 Unit of packed red blood cells was transfused. Haemoglobin level elevated. Iron deficit was calculated using Gazoni’s formula. Patient was started on ferric carboxylate maltose every week. Upper GI endoscopy showed cricopharygeal webs, linear furrows and exudates in distal oesophagus. Bougie dilatation was done and tissue was sent for biopsy which showed reflux oesophagitis. Patient was diagnosed with Plummer Vinson syndrome. Patient improved symptomatically and her haemoglobin was 9gm/dl Serum iron and ferritin levels came back to normal and patient was discharged (Table 1 and Figure 1).
| Hb | 6.1gm/dl |
| RBC | 3.1 million/cumm |
| WBC | 3960 cells/cumm |
| Platelets | 1.98 lakh/cumm |
| Serum Iron | 37 ug/dl |
| Serum ferritin | 3.91 ng/ ml |
| TIBC | 256 mg/dl |
Table 1: Shows values of complete blood counts and serum iron studies.
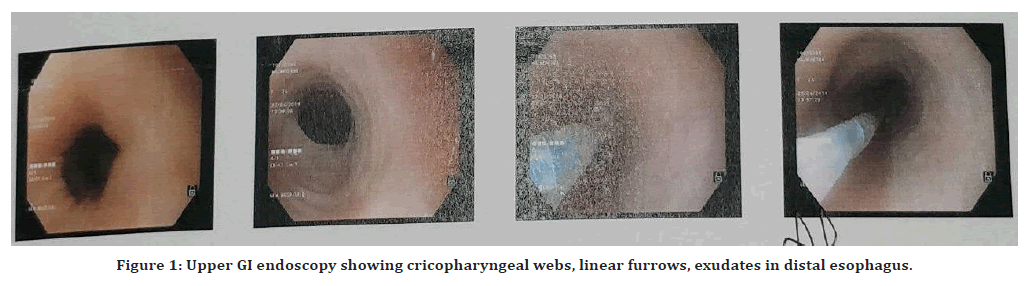
Figure 1. Upper GI endoscopy showing cricopharyngeal webs, linear furrows, exudates in distal esophagus.
Discussion
Due to its rarity, information on the frequency with which Plummer-Vinson syndrome [1] occurs is scarce. The emphasis of the majority of the cases is on case reports. Plummer- Vinson syndrome has been reported more frequently in temperate northern countries previously. Due to advances in diet and the treatment of iron deficiency anaemia, its prevalence has reduced. Furthermore, barium swallow or esophagoscopy [2] may detect webs, however only a small percentage of individuals have any symptoms. Interesting research was undertaken in South Wales in the 1960s; one population-based study found that post-cricoid webs were present in 0.3% and 1.1% of women, and in 8.4% and 22.4% of women with dysphagia [3], respectively, but were not found in any male participants. Patients with the Plummer-Vinson syndrome typically exhibit symptoms of iron deficiency anaemia, dysphagia, and upper oesophageal webs. On longstanding Iron deficiency anaemia presents as weakness, pallor, dyspnea, tachycardia, and koilonychia. Additional features are glossitis and angular chelitis. Dysphagia at first it is painless, gradually progressive, first to solid food and then develops difficulty in swallowing to liquids over years. Dysphagia is usually grade-1 or grade-2 in Plummer- Vinson syndrome.
Iron deficiency anaemia can be investigated by haematological profile. Radiological methods such as the barium swallow and esophagoscopy [4] can be used to detect oesophageal webs. Oesophagoscopy [4] is a double-edged sword, with diagnostic and therapeutic applications. Fibre optic endoscopy [5] is the gold standard for examining the digestive system since it is both safe and effective. In this case, iron supplements are used as treatment. If iron deficiency is treated, the mucosal abnormalities may disappear, and the risk will decrease. Patients with webs were managed with endoscopic dilation followed [4] by iron supplements.
Conclusion
Although Plummer-Vinson syndrome is uncommon, it can be efficiently treated with iron supplements and mechanical dilatation. Patients with Plummer-Vinson syndrome should be constantly monitored due to their higher risk of developing squamous cell carcinoma of the pharynx and oesophagus.
References
- Novacek G. Plummer-vinson syndrome. Orphanet J Rare Dis 2006; 1:36.
- Plummer H. Diffuse dilatation of the esophagus without anatomic stenosis (cardiospasm): A report of 91 cases. JAMA 1912; 58:2013-2015.
- Vinson P. A case of cardiospasm with dilatation and angulation of the esophagus. Med Clin North Am 1919; 3:623-627.
- Kelly A. Spasm at the entrance of the esophagus. J Laryngol Rhinol Otol 1919; 34:285-289.
- Paterson D. Clinical type of dysphagia. J Laryngol Rhinol Otol 1919; 34:289-291.
Indexed at, Google Scholar, Cross Ref
Author Info
Kosuri Akhila*, Suresh Kanna S, Goutham Kumar AP, Keerthana I and Kunduru Dinesh Reddy
Department of General Medicine, Sree Balaji Medical College and Hospital, Chrompet, IndiaReceived: 20-Aug-2022, Manuscript No. jrmds-22-75298; , Pre QC No. jrmds-22-75298(PQ); Editor assigned: 22-Aug-2022, Pre QC No. jrmds-22-75298(PQ); Reviewed: 06-Sep-2022, QC No. jrmds-22-75298(Q); Revised: 09-Sep-2022, Manuscript No. jrmds-22-75298(R); Published: 16-Sep-2022
