Research - (2021) Volume 9, Issue 8
A Three Step Screening Protocol for Early Detection of Renal Abnormalities in Asymptomatic Indian School Children
Ashish Kumar Goyal1, Pratik Akhani2 and Vijay Nayak3*
*Correspondence: Vijay Nayak, Department of Anatomy, Government Medical College, India, Email:
Abstract
Background & Objectives: Early screening of asymptomatic school children is of paramount important in the early detection and treatment of silent renal diseases. The purpose of this study was to find out the prevalence of renal abnormalities in asymptomatic school going children using a three step screening protocol of dipstick, microscopy and renal ultrasound examination. Methods: A total of 2722 school children (1638 boys and 1084 girls), aged 5–19 years, were screened for urinary abnormalities using dipstick, microscopy and renal ultrasound examination. 77 children found positive by dipstick, were screened by microscopy after 2-4 weeks and 44 children, found positive by microscopy, were screened by Renal Ultrasound Examination. Results: Most common abnormality found by dipstick method and microscopy was isolated pyuria followed by isolated haematuria. Renal ultrasound detected 2 children (1 male, 1 female) with hydro ureter with hydronephrosis, 1 female child with small concretion in kidney, and 1 male child with generalised enhancement of echo texture in kidney. Conclusion: Isolated pyuria, followed by isolated haematuria was the most common abnormalities. Such a three step screening protocol if routinely employed for early detection and treatment of renal abnormalities can decrease the incidence CKD and ESRD.
Keywords
Hematuria, Pyuria, Ultrasonography, Urogenital abnormalities, Chronic kidney failure
Introduction
The incidence of Chronic kidney disease (CKD) is on the rise worldwide, especially in paediatric population [1,2]. Early diagnosis and treatment of renal disorders is of utmost importance to prevent and in turn to reduce the disease burden of CKD in the community [3].
Screening for asymptomatic urinary abnormalities (AUA) is useful for early detection of renal diseases and asymptomatic infections, particularly among children [4]. Urinalysis, a simple and inexpensive test, remains to be a cornerstone in the diagnostic evaluation of kidney [5]. Many low cost screening programmes have been conducted using urinalysis for detection of kidney diseases [6,7].
Renal diseases are often accidentally discovered during routine urine analysis in asymptomatic healthy individuals [8]. With the aid of routine dipstick examinations early symptoms of diseases of the kidneys and the urinary tract (Pyuria, hematuria and proteinuria) can be identified [9]. An abnormal urinary test may be the earliest warning of a significant renal pathology [10,11].
Mass urinary screening helps to determine the prevalence of renal diseases [12] and to improve the outcome in the population [13].
This study was carried out with the objective to find out renal abnormalities in asymptomatic school going children using urinalysis, microscopy and renal ultrasound examination.
Materials and Methods
This cross sectional study was conducted at Military Hospital, Roorkee, Uttarakhand, India and included all asymptomatic school going children of 5-19 years of age (n=3100) studying at Kendriya Vidyalaya, Roorkee Cantonment, Roorkee. Children with diagnosed renal or any other systemic disorders, who were taking steroid or any other drug therapy, and whose parents denied to provide consent for participation were excluded from the study.
Age appropriate assent was obtained from children, while informed written consent was obtained from parents. Administrative consent was obtained from the school administration. All the procedures were in accordance with the ethical guidelines provided by the institutional ethics committee and the Declaration of Helsinki (2013 revision) [14]. The study commenced with establishment of a small lab in the school itself for the duration of study. Participants were instructed to void the first morning mid-stream urine sample into a 100 ml container, which was then examined by a trained lab technician. As the first screening test, a dipstick test (Multistix, by Nicholas Piramal) was performed on the unspun urine specimen with a reagent strip designed to react progressively producing color changes at given intervals.
The results were decided by visual colorimetry by comparision with a color chart provided by the manufacturer on the label of dipstick bottle. Urinalysis was considered abnormal if the following findings were detected by dipstick: 1. More than 5-10 RBC/μl; hematuria (Green dots on yellow test: intact erythrocytes; Uniform green coloration of test: free hemoglobin or hemolysed erythrocytes); 2. Trace or greater proteinuria (trace, 1+, 2+, 3+, 4+ correspond to 10 mg/dl, 30 mg/dl, 100 mg/dl, 300 mg/dl, and 1000 mg/dl respectively); 3. 1 + or greater glycosuria (1+, 2+, 3+ corresponds to 100 mg/dl, 300 mg/dl, and 1000 mg/dl respectively); 4. More than 25 WBC/μl; leukocyturia. Details of screening protocol are given in Figure 1. Statistical analysis was performed with the help of MS Excel and SPSS version 20. A p value lesser than 0.05 was taken to be statistically significant.
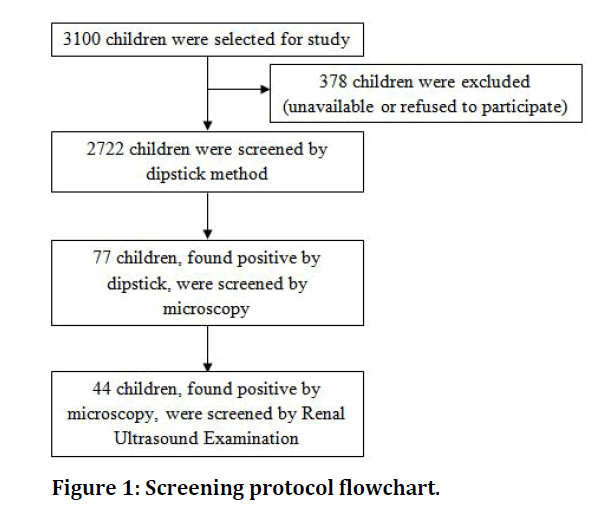
Figure 1: Screening protocol flowchart.
Results
Out of 3100 children in the school, 378 children could not be tested, being absent from school on the day of testing (because they were ill or had moved, etc.) or unable to urinate when requested.
Thus, data for 2722 children (1638 boys and 1084 girls) were included in the statistical analysis.
Out of 77 children, the most common abnormality found by dipstick method was isolated pyuria (WBC in urine) (n=28, 36%) followed by isolated Haematuria (n=21, 27%) (Table 1).
| Age group (in years) | Male | Female | Only WBC in Urine | Only RBC in Urine | RBC & WBC in Urine | Only Protein in Urine | Only Sugar in Urine | Protein & Sugar in Urine | Sugar & RBC in Urine |
|---|---|---|---|---|---|---|---|---|---|
| 5-8 | 8 | 5 | 8 | 3 | 1 | 1 | - | - | - |
| 9-10 | 3 | 10 | 5 | 5 | 1 | 2 | - | - | - |
| 11-12 | 1 | 15 | 8 | 4 | 3 | 1 | - | - | - |
| 13 - 14 | 14 | 12 | 6 | 6 | 7 | 6 | - | 1 | - |
| 15 - 17 | 6 | 3 | 1 | 3 | 3 | 1 | - | - | 1 |
| Total | 32 | 45 | 28 | 21 | 15 | 11 | Nil | 1 | 1 |
Table 1: Urine abnormalities by dipstick method (n=77).
By microscopy, out of 44 children, urine abnormalities were found in 70.5% females and 29.5% males. 47.7% were found to have isolated WBC in urine, 34% had isolated RBC in urine, 13.6% were having both RBC and WBC in urine and 4.5% were having only protein in urine (Table 2).
| Age group (in years) | Male | Female | Only WBC in Urine | Only RBC in Urine | RBC & WBC in Urine | Only Protein in Urine | Only Sugar in Urine | Protein & Sugar in Urine | Sugar & RBC in Urine |
|---|---|---|---|---|---|---|---|---|---|
| 5-8 | 1 | 3 | 3 | 1 | - | - | - | - | - |
| 9-10 | - | 6 | 3 | 3 | - | - | - | - | - |
| 11-12 | 1 | 11 | 7 | 3 | 1 | 1 | - | - | - |
| 13-14 | 6 | 8 | 6 | 5 | 3 | - | - | - | - |
| 15-17 | 5 | 3 | 2 | 3 | 2 | 1 | - | - | - |
| Total | 13 | 31 | 21 | 15 | 6 | 2 | Nil | Nil | Nil |
Table 2: Urine abnormalities by microscopy (n=44).
Renal ultrasound detected those 2 children (1 male, 1 female) had hydro ureter with hydronephrosis, 1 female child had small concretion in kidney, while 1 male child had generalised enhancement in echo texture in kidney (Table 3).
| Age group (in years) | Male | Female | Hydroureter with Hydronephrosis | Small Concretion | Generalised Enhancement in Echotexture |
|---|---|---|---|---|---|
| 5-10 | - | - | - | ||
| 11-17 | 2 | 2 | 2 | 1 | 1 |
| Total | 2 | 2 | 2 | 1 | 1 |
Table 3: Kidney abnormalities detected by renal USG (n=4).
Discussion
A significant number of disorders of kidney and urinary tract can remain asymptomatic for a long duration of time. Therefore, it is recommended to routinely conduct urinalysis screening programs for early diagnosis and management of renal damage. This strategy has been particularly important in reducing the gradually increasing burden of CKD in both developed and developing countries.
Findings of our study i.e. hematuria, proteinuria and pyuria in school going children were compared to other studies globally. Our finding of urinary abnormalities was nearly 2.9% of the studied group which was similar to the 2.5% and the 2.3% reported in Northern Iran and Malaysia respectively [15,16] higher than the 0.6% and the 0.72% reported in Tokyo and Egypt respectively [17,18] and lower than the 7.2% and the 9.6% reported in Bolivian and Nigerian studies respectively [19,20].
Pyuria was the most common urinary abnormality in our study. Whereas, other studies reported proteinuria as the commonest abnormality [18,20]. Hematuria prevalence was reported to be 0.21%, 0.36% and 0.46% in Malaysia, Egypt and Shanghai respectively [16,18,21] which is similar to our results of 0.22%. A higher prevalence 1.5% and 1.21% was reported from Nigerian and Xiamen cities respectively [20,22]. Bergstein et al reported hypercalciuria as the most common urinary abnormality (in 16%) [23], which was flowed by MPGN (membranoproliferative glomerulonephritis) and PSGN (poststreptococcal glomerulonephritis) [24]. Vehaskari et al reported IgA nephropathy in two and Alport syndrome in one children by studying the renal biopsy of 22 children who had microscopic haematuria [25].
A study from Japan reported 7 cases of minor glomerular abnormalities, and 6 cases of IgA nephropathy among 220 children having microscopic haematuria [26]. These studies showed that microscopic asymptomatic hematuria might be benign but it can also be an important sign of underlying disease.
Proteinuria could be a temporary finding in normal children or an important manifestation of an underlying renal disease. It is an independent and important risk factor for ESRD (end stage renal disease). Therefore, asymptomatic proteinuria warrants further work up to detect and even prevent ESRD [27]. A study conducted in China reported that 2.87% children with urine abnormalities were detected by Ultrasound alone while 0.79% by both Ultrasound and urine alysis as compared to 0.15% and 0.07% respectively in our study [28].
A limitation of our study was that did not follow up the participants. Long-term follow up is important because children showing urinary abnormalities may develop full-blown kidney disease. The urinary dipstick method is mainly sensitive for albumin while quantitative analysis methods can detect all renal proteins.
Conclusion
Our study assessed the prevalence of urinary abnormalities in school-aged children of India and isolated pyuria was found to be the most common urinary abnormality, followed by isolated haematuria. Such a three step screening protocol if routinely employed for early detection and treatment of renal abnormalities can decrease the incidence CKD and ESRD.
References
- Shalaby MA, Abd El Hameed AE, Affifi WE, et al. Screening for urine abnormalities among school children in Qalubyia. Geget 2019; 14:75-81.
- https://emedicine.medscape.com/article/984358.
- Parakh P, Bhatta NK, Mishra OP, et al. Urinary screening for detection of renal abnormalities in asymptomatic school children. Nephrol Mon 2012; 4:551-555.
- Nour MO, Mansour AE, Ghandour AA, et al. Prevalence of asymptomatic urinary abnormalities among primary school children in damietta governorate. Umm Al-Qura Univ Med J 2013; 4:1-8.
- Alharthi AA, Taha AA, Edrees AE, et al. Screening for urine abnormalities among preschool children in western Saudi Arabia. Saudi Med J 2014; 35:1477.
- Marquette GP, Dillard T, Bietla S, et al. The validity of the leukocyte esterase reagent test strip in detecting significant leukocyturia. Am J Obstet Gynecol 1985; 153:888-889.
- Arm JP, Peile EB, Rainford DJ, et al. Significance of dipstick hematuria: Correlation with microscopy of the urine. Br J Urol 1986; 58:211-217.
- Ahmed Z, Lee J. Asymptomatic urinary abnormalities. Hematuria and proteinuria. Med Clin North Am 1997; 81:641–52.
- Longo DL, Kasper DL, Jameson JL, et al. Harrison’s principles of internal medicine. 18th Edn. New Delhi: McGraw Hill Medical Publishing Division, 2011.
- Abitbol C, Zilleruelo G, Freundlich M. Quantitation of proteinuria with urine protein/creatinine ratios and random testing with dipsticks in children. J Pediatr 1990; 116: 243-7.
- Bard RH: The significance of asymptomatic hematuria in women and its economic implications: A ten-year study. Arch Intern Med 1988; 148:2629-32.
- Kitagawa T. Lessons learned from the Japanese nephritis screening study. Pediatr Nephrol. 1988; 2:256-263.
- Park YH, Choi JY, Chung HS, et al. Hematuria and proteinuria in a mass school urine screening test. Pediatr Nephrol 2005; 20:1126-1130.
- World medical association declaration of helsinki. Ethical principles for medical research involving human subjects. JAMA 2013; 310:2191-2194.
- Badeli H, Heidarzadeh A, Ahmadian M. Prevalence of hematuria and proteinuria in healthy 4 to 6 year old children in daycare centers of Rasht (Northern Iran). Iran J Pediatr 2009; 19:169–172.
- Zainal D, Baba A, Mustaffa BE. Screening proteinuria and hematuria in Malaysian children. Southeast Asian J Trop Med Public Health 1995; 26:785–788.
- Murakami M, Yamamoto H, Ueda Y, et al Urinary screening of elementary and junior high-school children over a 13 year period in Tokyo. Pediatr Nephrol 1991; 5:50–53.
- Bakr A, Sarhan A, Hammad A, et al. Asymptomatic urinary abnormalities among primary school children in Egypt. World J Pediatr 2007; 3:214–217.
- Plata R, Silva C, Yahuita J, et al. The first clinical and epidemiological programme on renal disease in Bolivia: A model for prevention and early diagnosis of renal diseases in the developing countries. Nephrol Dial Transplant 1998; 13:3034–3036.
- Akor F, Okolo S, Agaba E, et al. Urine examination findings in apparently healthy new school entrants in Jos, Nigeria. SA J Child Health 2009; 3:60–63.
- Rao J, Zhou L, Shen Q, et al. School urinalysis screening in Shanghai. World J Pediatr 2006; 3:195–198.
- Tong S, Gui-lan P, Hui-fen Z, et al. Urine routine screening of 34455 school children in Xiamen city. J Child Health Care 2009; 1.
- Bergstein J, Leiser J, Andreoli S. The clinical significance of asymptomatic gross and microscopic hematuria in children. Arch Pediatr Adolesc Med 2005; 159:353–355.
- Stapleton F. Asymptomatic microscopic hematuria. Arch Pediatr Adolesc Med 2005; 159:398–399.
- Vehaskari VM, Rapola J, Koskimies O, et al. Microscopic hematuria in schoolchildren: epidemiology and clinicopathologic evaluation. J Pediatr 1979; 95:676–684.
- Murakami M, Hayakawa M, Yanagihara T, et al. Proteinuria screening for children. Kidney Int 2005; 68:S23–27.
- Hanif R, Ally S, Jalal-ud-din, et al. Effectiveness of routine urinalysis of patients attending rural health care centers in abbottabad. J Ayub Med Coll Abbottabad 2006; 18:63-64.
- Yang H, Wang Q, Luo J et al. Ultrasound of urinary screening in 14256 aymptomatic children in China. Nephrology 2010; 15:362-367.
Author Info
Ashish Kumar Goyal1, Pratik Akhani2 and Vijay Nayak3*
1Military Hospital, Roorkee-247667, Uttarakhand, India2Department of Physiology, Government Medical College, Khandwa, Madhya Pradesh, India
3Department of Anatomy, Government Medical College, Khandwa, Madhya Pradesh, India
Citation: Ashish Kumar Goyal, Pratik Akhani, Vijay Nayak,A Three Step Screening Protocol for Early Detection of Renal Abnormalities in Asymptomatic Indian School Children , J Res Med Dent Sci, 2021, 9(8): 339-342
Received: 07-Aug-2021 Accepted: 23-Aug-2021
