Research - (2021) Volume 9, Issue 11
A Study to Assess the Effectiveness of Twin Technique with Nebulization on Respiratory Status among Patients with Chronic Obstructive Pulmonary Disease and Bronchiectasis
*Correspondence: AR Bharathi, Department of Nursing, Bharath Institute of Higher Education and Research, Selaiyur, Chennai-600073 Tamil Nadu, India, Email:
Abstract
Breathing is a mandatory involuntary activity of the body to sustain life. When normal breathing is disrupted it results in compromised homeostasis and health, in general. In patients suffering with respiratory diseases like chronic obstructive pulmonary disorder (COPD), upper respiratory tract infection, asthma and bronchiectasis, breathing difficulty is predominantly seen. Inhalation therapy has been recommended as the favoured route of administration COPD treatment. Nebulizers are used in reversal of airways obstruction with bronchodilators, mucus clearance, and reduction in microbial load. Hence the present study was designed to assess the effectiveness of twin technique with nebulization on respiratory status among patients with chronic obstructive pulmonary disease (COPD) and bronchiectasis.
Keywords
Nebulization, Twin technique, Respiratory diseases, Chronic obstructive pulmonary disease (COPD), Bronchiectasis, Breathing
Introduction
Breathing is a mandatory involuntary activity of the body to sustain life. Inhalation causes outside air to enter the lungs and the oxygen in the air mixes with the blood and is distributed throughout the body. Simultaneously, carbon dioxide is let out from the cells to the lungs and out of the body during exhalation. This mechanism is called gas exchange [1]. When normal breathing is disrupted it results in compromised homeostasis and health, in general [2]. Normally, a quick walk or intense exercise makes breathing difficult but in time it gets back to normal. But in patients suffering with respiratory diseases, the normal breathing does not return to normal. Some of the respiratory diseases are chronic obstructive pulmonary disorder (COPD), upper respiratory tract infection, asthma and bronchiectasis.
COPD is caused due to continuous exposure to lung irritants such as tobacco smoke, industrial materials and chemicals, polluted air, childhood respiratory infection, etc. Rarely COPD is caused due to a genetic condition which causes deficiency in Alpha-1 Antitrypsin (AAT), a protein which protects the lungs from inflammation damage [3]. Inhalation therapy has been recommended as the favoured route of administration COPD treatment [4]. The patients suffering from long term with moderate and severe symptoms and those most susceptible to COPD are mostly recommended to take Bronchodilators (β2- agonists and antimuscarinics) [5]. Both the patient and the doctors are most satisfied with using Nebulization for drug delivery as most of the drugs come in liquid formulations [5]. Pressurized metered dose inhalers (pMDIs), dry powder inhalers (DPIs), slow mist inhalers (SMIs), and nebulizers are the commonly used inhalers used in COPD patients [6,7]. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) strategy document states that using nebulizers are more productive in treating COPD than using DPIs or MDIs. Being the fourth leading cause of death globally COPD remains as one of the challenges to medical field.
Bronchiectasis is another important respiratory condition. In bronchiectasis, the airways to the lungs slowly lose their ability to clear out mucus. Mucus builds up overtime becoming a breeding ground for bacteria and lung infections [8]. Bronchiectasis can lead to serious health problems, such as respiratory failure, atelectasis (at-eh- LEK-tah-sis), and heart failure [8]. Almost all bronchiectasis patients have been found to have sputum intermittently or daily [9]. Few studies have been published on the use of nebulizers in bronchiectasis. Nebulizers are used in reversal of airways obstruction with bronchodilators, mucus clearance, and reduction in microbial load [9].
A nebulizer uses an air compressor to turn liquid medication into a fine mist that can be inhaled and delivered across the respiratory system, to the lungs. The nebulizer has three basic components: an air compressor, a medicine cup, and a mouthpiece or a mask [10]. Some nebulizers need to be plugged in but currently most of them run on batteries [11]. Nebulizers are mostly preferred due to their efficacy, convenience, low cost [4], dispersion of any amount and wide variety of medicine and suitability for using in infants [10].
Hence the present study was designed to assess the effectiveness of twin technique with nebulization on respiratory status among patients with chronic obstructive pulmonary disease (COPD) and bronchiectasis.
Methodology
Quantitative approach has been adopted for this study (Table 1. Research design used in this study is Quasi Experimental One group pre-test post- test design.
| Pre-assessment | Intervention | Post-assessment |
|---|---|---|
| Assessment of level of existing respiratory status based on respiratory rate, oxygen saturation, expiratory flow rate, indirectly indicate chest expansion, lung volume, by using, Modified Borg dyspnoea scale, pulse oxymetry, Peak Flow Meter, Respiratory Rating scale | Administered twin technique with nebulization 3 times per day for 6 days. | On the 6th day assessment of respiratory status based on respiratory rate, oxygen saturation, expiratory flow rate, indirectly indicate lung volume expansion, by using, Modified Borg dyspnoea scale, pulse oxymetry, Peak Flow Meter, Respiratory Rating scale |
Table 1: According to polit and beck the schematic representation of one group pre-test post- test shown.
The selection of the hospital for the present study was on the basis of availability of subjects, feasibility of conducting study and economy of time. The study conducted in Male & Female Medical wards General Hospital, Chennai. 30 patients were randomly selected for this study. Firstly, the Patient profile (Name, IP no, Diagnosis, Demographic variable includes Age, Sex, Residential Area, Religion, Education, Occupation, Monthly income, Area of work duration of respiratory diseases, family history of respiratory diseases, and allergic reactions use of alternative medicine , regular morning exercise, Breathing difficulty) was assessed. Secondly, the respiratory status with the help of Respiratory Rate, modified Borg dyspnea scale, peak flow meter and pulse oximeter was measured. The criteria for respiratory assessment are adequate and inadequate (Table 2).
| Parameter | Criteria | ||
|---|---|---|---|
| I | Respiratory Rate | Adequate | |
| b) | 12-22 breaths/minute- normal | ||
| II | Modified Borg dyspnea scale | ||
| a) | Grade I- slight breathlessness | ||
| III | Peak flow meter | ||
| a) | 81-100%- free of symptoms | ||
| IV | Pulseoxymeter | ||
| a) | 91-100% oxygen saturation normal | ||
| I | Respiratory Rate | Inadequate | |
| a) | <12 breaths/minute-bradypnea | ||
| c) | >22 breaths/minute- tachypnea | ||
| II | Modified Borg dyspnea scale | ||
| b) | Grade II- moderate breathlessness | ||
| c) | Grade III- severe breathlessness | ||
| d) | Grade IV-maximum breathlessness | ||
| III | Peak flow meter | ||
| b) | 51-80%- caution | ||
| c) | <50%- danger | ||
| IV | Pulseoxymeter | ||
| b) | 81-90% oxygen saturation-Desaturated | ||
| c) | 70-80% oxygen saturation-hypoxic | ||
Table 2: Representation of criteria of respiratory assessment from respiratory rate modified borg dyspnea scale, peak flow meter and pulseoxymeter.
Twin technique with nebulization was done on COPD and bronchiectasis patients (Table 3).
| Number of patients per day | Pre-test | Post-test | ||
|---|---|---|---|---|
| Date | Time | Date | Time | |
| 3 | 1/10/2019 | 5:00am | 6/10/2019 | 5:00am |
| 3 | 3/10/2019 | 5:00am | 8/10/2019 | 5:00am |
| 2 | 5/10/2019 | 5:00am | 10/10/2019 | 5:00am |
| 2 | 7/10/2019 | 5:00am | 12/10/2019 | 5:00am |
| 3 | 9/10/2019 | 5:00am | 14/10/19 | 5:00am |
| 2 | 11/10/2019 | 5:00am | 16/10/19 | 5:00am |
| 2 | 13/10/19 | 5:00am | 18/10/19 | 5:00am |
| 2 | 15/10/19 | 5:00am | 20/10/19 | 5:00am |
| 3 | 17/10/19 | 5:00am | 22/10/19 | 5:00am |
| 2 | 19/10/19 | 5:00am | 24/10/19 | 5:00am |
| 3 | 21/10/19 | 5:00am | 26/10/19 | 5:00am |
| 2 | 23/10/19 | 5:00am | 28/10/19 | 5:00am |
| 2 | 5/10/2019 | 5:00am | 30/10/19 | 5:00am |
Table 3: Data collection schedule.
The proposed study was conducted after the approval of the institutional ethical committee. Permissions were obtained from the concerned hospital. Informed consent was obtained from the patients.
Subjects were given the right to withdraw from the study any time they want and assurance of their privacy and anonymity was assured.
Descriptive statistics was used to assess the demographic variables including frequency and percentage.
Descriptive and inferential statistics like Independent and paired‘t’ test and Chi Square test was used to compare the data between the two groups. The analyzed data was presented in the form of tables, diagrams and graphs.
Results
The analysis and interpretation of data of this study were based on data collected through pre-assessment questionnaire and observation. The results were computed by using descriptive and inferential statistics.
Table 4 depicted the distribution of demographic variable of patients with lower respiratory tract infection chronic obstructive pulmonary disease, and bronchiectasis.
| Sl.no | Demographic variables | N | % |
|---|---|---|---|
| 1 | Age in years | ||
| <20 | 0 | 0% | |
| 21-40 | 4 | 12% | |
| 41-60 | 2 | 6% | |
| 61 and above | 24 | 72% | |
| 2 | Sex | ||
| Male | 15 | 45% | |
| Female | 15 | 45% | |
| 3 | Residential area | ||
| Rural | 18 | 54% | |
| Semi urban | 10 | 30% | |
| Urban | 2 | 7% | |
| 4 | Religion | ||
| a. Hindu | 22 | 66% | |
| b. Christian | 3 | 9% | |
| c. Muslim | 5 | 15% | |
| d. Others | 0 | 0 | |
| 5 | Educational status | ||
| a. Illiterate | 10 | 30% | |
| b. Primary | 13 | 39% | |
| c. Secondary | 6 | 18% | |
| d. Higher secondary | 1 | 5% | |
| e. Graduate | 0 | 0 | |
| 6 | Type of employment | ||
| a. Self employed | 6 | 18% | |
| b. Agriculture | 16 | 48% | |
| c. Coolie | 8 | 32% | |
| d. Technical | 0 | 0 | |
| e. Professional | 0 | 0 | |
| 7 | Area of work | ||
| a. Industries | 0 | 0 | |
| b. Field | 25 | 100% | |
| c. Road workers | 1 | 4 | |
| d. Mining | 0 | 0 | |
| e. Florist | 2 | 4% | |
| f. Building construction | 2 | 4% | |
| 8 | g. Others | 0 | 0 |
| Family income per month in rupees | |||
| a. <2000 | 17 | 54% | |
| b. 2001-4000 | 13 | 39% | |
| c. 4001-6000 | 0 | 0 | |
| 9 | d. 6001 and above | 0 | 0 |
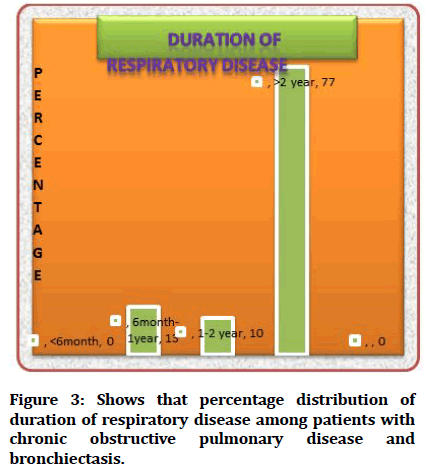
| Duration of respiratory disease of COPD & Bronchiectasis | |||
| a. <6 month | 0 | 0 | |
| b. 6month-1 year | 4 | 12% | |
| c. 1-2 year | 3 | 10% | |
| d. >2 year | 23 | 66% | |
| 10 | General appearance of the patient | ||
| a. Thin body built | 26 | 78% | |
| b. Moderately body built | 4 | 13% | |
| c. Obese | 0 | 0 | |
| 11 | Do you have any unhealthy habit. If yes tick any one of the following | ||
| a. Tobacco chewing | 1 | 4% | |
| b. Alcoholism | 2 | 4% | |
| c. Smoking | 23 | 69% | |
| d. Drug abuse | 0 | 0 | |
| e. Mixed option | 4 | 12% | |
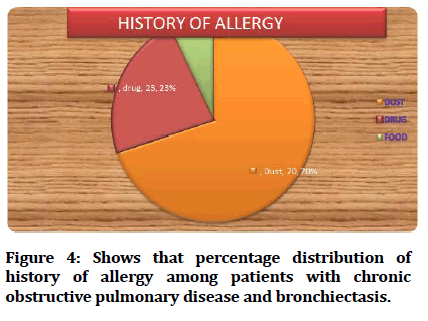
| 12 | History of any allergy? If yes tick any one of the following | ||
| a. Dust | 21 | 63% | |
| b. Drug | 7 | 21% | |
| c. Food | 2 | 8% | |
| 13 | Are you taking any alternative medicine | ||
| a. Yes | 16 | 48% | |
| b. No | 14 | 42% | |
| 14 | Do you use any inhalation devices? | ||
| a. Meter dose inhaler | 21 | 63% | |
| b. Home use steam inhaler | 9 | 36% | |
| 15 | Do you have any habit of early morning exercise like walking? | ||
| a. Yes | 12 | 48% | |
| b. No | 18 | 56% | |
| 16 | Are you taking any medication such as bronchodilator, and corticosteroid? | ||
| a. Yes | 21 | 63% | |
| b. No | 9 | 30% | |
| 17 | Do you have breathing difficulty periodically | ||
| a. Yes | 22 | 68% | |
| b. No | 8 | 32% | |
Table 4: Frequency and percentage distribution of demographic variable of patients with lower respiratory tract infection chronic obstructive pulmonary disease, and bronchiectasis.
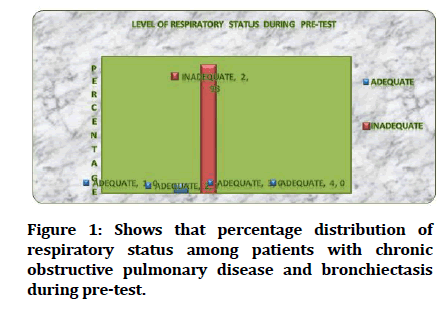
Table 5 shows the distribution of respiratory status among patients with chronic obstructive pulmonary disease and bronchiectasis during pre-test. Most of the patients i.e. 28 (93%) are having inadequate respiratory status and only 2 (7%) of them had adequate respiratory status.
| Respiratory status | Frequency (N) | Percentage (%) |
|---|---|---|
| Adequate | 2 | 8% |
| Inadequate | 28 | 96% |
Table 5: Frequency and percentage distribution of respiratory status among patients with chronic obstructive pulmonary disease and bronchiectasis during pre-test.
Table 6 showed the frequency and percentage distribution of respiratory pattern assessed Borg Dyspnoea scale, among patients with chronic obstructive pulmonary disease and bronchiectasis during pre-test. Data shows that majority of the subjects 12(40%) of them were in Grade III category - severe breathlessness, and 11(37%) of them were Grade IV-maximum breathlessness. Only 7(23%) subject were found Grade II-moderate breathlessness, and none of them were in Grade I- slight breathlessness.
| Respiratory pattern (Dyspnoea) | Frequency (N) | Percentage (%) |
|---|---|---|
| Grade I | ||
| Slight breathlessness | 0 | 0 |
| Grade II | ||
| Moderate breathlessness | 7 | 21% |
| Grade III | ||
| Severe Breathlessness | 12 | 36% |
| Grade IV | ||
| Maximum | 11 | 33% |
Table 6: Frequency and percentage distribution of respiratory pattern assessed with Borg dyspnoea scale among patients with chronic obstructive pulmonary disease and bronchiectasis during pre-test.
Table 7 showed the frequency and percentage distribution of oxygen saturation assessed with pulse oximeter among patients with chronic obstructive pulmonary disease and bronchiectasis during pre-test.
| Oxygen saturation | Frequency (N) | Percentage (%) |
|---|---|---|
| 91-100%-Normal | 0 | 0 |
| 81-90%-Desaturated | 15 | 45% |
| <80%-Hypoxic | 15 | 45% |
Table 7: Frequency and percentage distribution of oxygen saturation assessed with pulse oximeter among patients with chronic obstructive pulmonary disease and bronchiectasis during pre-test.
Among 30 subjects half of the subjects Desaturated i.e. 15(50%) that is with oxygen saturation level between 81-90% and 15(50%) of them were hypoxic that is oxygen desaturation <80%.
Table 8 depicts the frequency and percentage distribution of lung volume expansion assessed with peak flow meter among patients with chronic obstructive pulmonary disease and bronchiectasis during pre-test .Half of them i.e,16(53%) are in danger with a level <50% and 14(47%) of them were in caution with a level between 50-80%. None of them were found in free of symptoms.
| Peak expiratory flow rate | Frequency (N) | Percentage (%) |
|---|---|---|
| Free of symptoms 81-100% | 0 | 0 |
| Caution 50-80% | 14 | 42% |
| Danger <50% | 16 | 48% |
Table 8: Frequency and percentage distribution of lung volume expansion assessed with peak flow meter among patients with chronic obstructive pulmonary disease and bronchiectasis during pre-test.
Table 9 shows the distribution of respiratory rate among patients with chronic obstructive pulmonary disease and bronchiectasis pre-test. Most of the subjects 25(83%) having Bradypnoea with less than <12 breaths /minute. Rest of the samples i.e.5 (17%) having Tachypnoea with less than >22 breaths/minute.
| Respiratory rate | Frequency (N) | Percentage (%) |
|---|---|---|
| Normal 12-22 breaths/minute | 0 | 0 |
| Bradypnoea <12 breaths /minute | 25 | 75 |
| Tachypnoea >22 breaths /minute | 5 | 15 |
Table 9: Frequency and percentage distribution of respiratory rate among patients with chronic obstructive pulmonary disease and bronchiectasis during pre-test.
Table 10 shows the frequency and percentage distribution of respiratory status among patients with chronic obstructive pulmonary disease and bronchiectasis. Among 30 subjects all (100%) of them had adequate respiratory status during post-test.
| Respiratory status | Frequency (N) | Percentage (%) |
|---|---|---|
| Adequate | 30 | 100% |
| Inadequate | 0 | 0 |
Table 10: Frequency and percentage of respiratory status among patients with chronic obstructive pulmonary disease and bronchiectasis during post-test.
Table 11 Showed the frequency and percentage distribution of respiratory pattern (dyspnoea) assessed with Borg Dyspnoea scale among patients with chronic obstructive pulmonary disease and bronchiectasis during post-test. Data shows that majority of the subjects 20(67%) were in Grade 1-slight breathlessness, and 10(33%) of them in grade II moderate breathlessness during post-test.
| Respiratory pattern(Dyspnoea) | Frequency (N) | Percentage (%) |
|---|---|---|
| Grade I | ||
| Slight breathlessness | 20 | 60 |
| Grade II | ||
| Moderate breathlessness | 10 | 30% |
| Grade III | ||
| Severe Breathlessness | 0 | 0 |
| Grade IV | ||
| Maximum | 0 | 0 |
Table 11: Frequency and percentage distribution of respiratory pattern assessed with Borg dyspnoea scale among patients with chronic obstructive pulmonary disease and bronchiectasis during post-test.
Table 12 showed the frequency and percentage distribution of oxygen saturation assessed with pulse oximeter among patients with chronic obstructive pulmonary disease and bronchiectasis. Among 30 subjects majority of the them 24(80%) had normal oxygen saturation that is 91-100%, only 6(20%) of them are Desaturated that is saturation level between 81-90% during post-test.
| Oxygen saturation | Frequency (N) | Percentage (%) |
|---|---|---|
| Normal-91-100% | 24 | 80% |
| Desaturated-81-90% | 6 | 20% |
| Hypoxic-<80% | 0 | 0 |
Table 12: Frequency and percentage distribution of oxygen saturation assessed with pulse oxymetry among patients with chronic obstructive pulmonary disease and bronchiectasis during post-test.
Table 13 showed the frequency and percentage distribution of lung volume expansion assessed with peak flow meter among patients with chronic obstructive pulmonary disease and bronchiectasis during post-test.
| Lung volume expansion | Frequency (N) | Percentage (%) |
|---|---|---|
| Free of symptoms 81-100% | 23 | 69% |
| Caution 50-80% | 7 | 21% |
| Danger <50% | 0 | 0 |
Table 13: Frequency and percentage distribution of lung volume expansion assessed with peak flow meter among patients with chronic obstructive pulmonary disease and bronchiectasis during post-test.
Among 30 subjects most of them 23(77%) are in category with free of symptoms that is 81-100% and 7(23%) of them were in caution that is 50-80%. None of them were found in danger during post-test.
Table 14 showed the frequency and percentage distribution of respiratory rate among patients with chronic obstructive pulmonary disease and bronchiectasis. All of them had normal respiratory rate that is 100% during post-test.
| Respiratory rate | Frequency (N) | Percentage (%) |
|---|---|---|
| Normal- 12-22breaths/minute | 30 | 100% |
| Bradypnoea <12breaths/minute | 0 | 0 |
| Tachypnoea >22breaths/minute | 0 | 0 |
Table 14: Frequency and percentage distribution of respiratory rate among patients with chronic obstructive pulmonary disease and bronchiectasis during post-test.
Table 15 showed that distribution of mean respiratory status of patients with chronic obstructive pulmonary disease and bronchiectasis during pretest and post .The mean difference was 0.93. Pre- test score was (1.93) and post-test respiratory rate score was (1), it was low of pretest score. The standard deviation of pretest respiratory rate score was 0.254 and post-test respiratory rate score was 0.The obtained paired ‘t’ value was 20.149and P value was 0.000*. It was significant at p<0.001% level. Hence the stated null hypothesis was rejected. It was inferred that the twin technique with nebulization was effective on improving the respiratory status of patients with chronic obstructive pulmonary disease and bronchiectasis.
| Sl.no | Variables | Mean | Standard deviation | Mean difference | Paired ‘t’ Value | P Value |
|---|---|---|---|---|---|---|
| 1 | Pre-test | 1.93 | 0.254 | 20.149 | 0.000*** | |
| 2 | Post-test | 1 | 0 | 0.93 | ||
| ***Highly significant at p<0.001 | ||||||
Table 15: Distribution of mean respiratory status of patients with chronic obstructive pulmonary disease and bronchiectasis during pretest and post –test.
Table 16 revealed that Distribution of mean respiratory pattern (dyspnoea) of patients with chronic obstructive pulmonary disease and bronchiectasis during pretest and post-test assessed with Borg Dyspnoea Scale .The mean difference was 1.8 between pre-test mean score was (3.13) and post-test mean score was (1.33). The standard deviation of pre-test score was 0.776 and post test score was 0.476. The obtained paired‘t’ value was 12.245 and p value 0.000***. It was highly significant at p<0.001 level. Hence the stated null hypothesis was rejected. It was inferred that the twin technique with nebulization is effective on improving the respiratory status of patients with chronic obstructive pulmonary disease and bronchiectasis.
| Sl.no | Variable | Mean | Standard deviation | Mean Difference | Paired ‘t’ value | P value |
|---|---|---|---|---|---|---|
| 1 | Borg Pre-Test | 3.13 | 0.776 | 1.8 | 12.245 | 0.000*** |
| 2 | Borg Post-Test | 1.33 | 0.476 | |||
| ***Highly significant at P<0.001 | ||||||
Table 16: Distribution of mean respiratory pattern of patients with chronic obstructive pulmonary disease and bronchiectasis during pretest and post-test assessed with Borg dyspnoea scale.
Table 17 revealed that, distribution of mean oxygen saturation of patients with chronic obstructive pulmonary disease and bronchiectasis during pretest and post-test assessed with pulse oximeter. The mean difference was 1.3 between the pre-test mean score was (2.50) and post test score was (1.20). The obtained paired‘t’ value was 15.77 and p value was 0.000***. It was highly significant at p<0.001% level. Hence the stated null hypothesis was rejected. It was inferred that the twin technique with nebulization on improving the respiratory status of patients with chronic obstructive pulmonary disease and bronchiectasis.
| Sl.no | Variable Pulse oxymetry | Mean | Standard Deviation | Mean difference | Paired ‘t’ value | P value |
|---|---|---|---|---|---|---|
| 1 | Pre-test | 2.5 | 0.509 | 1.3 | 15.777 | 0.000*** |
| 2 | Post- test | 1.2 | 0.407 | |||
| ***Highly significant at p<0.001 | ||||||
Table 17: Distribution of mean oxygen saturation of patients with chronic obstructive pulmonary disease and bronchiectasis during pretest and post-test assessed with pulse oximeter.
Table 18 revealed that distribution of mean lung volume expansion of patients with chronic obstructive pulmonary disease and bronchiectasis during pretest and post-test. The mean difference was 1.3 the mean pre-test score was 2.53 and post test score was 1.23 it was lower than the pre-test score. The standard deviation of pretest score was .507 and post test score was 0.430. The obtained paired ‘t’ value was 15.777 and p value was 0.000. It was significant at p<0.001% level. Hence the stated null hypothesis was rejected. It was inferred that the twin technique with nebulization is effective on improving the respiratory status of patients with chronic obstructive pulmonary disease and bronchiectasis.
| Sl.no | Variable Peak flow meter | Mean | Standard Deviation | Mean difference | Paired ‘t’ value | P value |
|---|---|---|---|---|---|---|
| 1 | Pre-Test | 2.53 | 0.507 | 1.3 | 15.777 | 0.000*** |
| 2 | Post-Test | 1.23 | 0.43 | |||
| ***Highly significant at P<0.001 | ||||||
Table 18: Distribution of mean lung volume expansion of patients with chronic obstructive pulmonary disease and bronchiectasis during pretest and post-test.
The table 19 revealed that, Distribution of mean respiratory rate of patients with chronic obstructive pulmonary disease and bronchiectasis during pretest and post-test. The mean pre-test score 2.17 and post test score 1.00 it was lower than the pre-test score. The standard deviation of pre-test score was 0.379 and post test score was 0.000. The obtained paired‘t’ value was 16.858 and p value was 0.000.It was significant at p<0.001% level. Hence the stated null hypothesis was rejected It was inferred that the twin technique with nebulization is effective on improving the respiratory status of patients with chronic obstructive pulmonary disease and bronchiectasis.
| Sl.no | Variable Respiratory Rate | Mean | Standard Deviation | Mean difference | Paired ‘t’ value | P value |
|---|---|---|---|---|---|---|
| 1 | Pre-Test | 2.17 | 0.379 | 16.858 | 0.000*** | |
| 2 | Post- Test | 1 | 0.000 | 1.17 | ||
| ***Highly significant at p<0.001 | ||||||
Table 19: Distribution of mean respiratory rate of patients with chronic obstructive pulmonary disease and bronchiectasis during pretest and post-test.
With regards to age no one of them in age group of <20 years, 4(13%) of them in age group of 21-40 years had adequate respiratory status, only 2(7%) of them in age group 41-60 years had inadequate respiratory status. Most of them 24(80%) had adequate respiratory status in age group of 60 and above. The obtained χ² value was 30.000 and P value=0.000* which is significant at p<0.001 level (Table. 20).
| Sl.no | Demographic Variables | Adequate respiratory Status | Inadequate respiratory status | χ² value (df) | P value | ||
|---|---|---|---|---|---|---|---|
| N | % | N | % | ||||
| Age in years | |||||||
| 1 | <20 years | _ | _ | _ | _ | 30.000 (2) | 0.000*** |
| 2 | 21-40 years | 4 | 13 | 0 | 0 | ||
| 3 | 41-60 years | 0 | 0 | 2 | 7% | ||
| 4 | 60 and above | 24 | 80% | 0 | 0 | ||
| *** Highly Significant at p< 0.001 | |||||||
Table 20: Association of effectiveness of twin technique with nebulization on respiratory status of patients with chronic obstructive pulmonary disease and bronchiectasis with their age.
Hence there is significant association between effectiveness of twin technique with nebulization of respiratory status of patients with chronic obstructive pulmonary disease and bronchiectasis with their age. This concludes that there is a relationship between the patient’s age and the effectiveness of twin technique with nebulization Mere the age poor the respiratory status that may be due to physiological changes during aging.
Table 20 showed that association of effectiveness of twin technique with nebulization on respiratory status of patients with chronic obstructive pulmonary disease and bronchiectasis with their age. The study findings had been summarized in Figures 1-7.
Figure 1: Shows that percentage distribution of respiratory status among patients with chronic obstructive pulmonary disease and bronchiectasis during pre-test.
Figure 2: Shows that percentage distribution of area of work among patients with chronic obstructive pulmonary disease and bronchiectasis.
Figure 3: Shows that percentage distribution of duration of respiratory disease among patients with chronic obstructive pulmonary disease and bronchiectasis.
Figure 4: Shows that percentage distribution of history of allergy among patients with chronic obstructive pulmonary disease and bronchiectasis.
Figure 5: Shows that percentage distribution of general appearance among patients with chronic obstructive pulmonary disease and bronchiectasis.
Figure 6: Shows that percentage distribution of respiratory status among patients with chronic obstructive pulmonary disease and bronchiectasis during post-test.
Figure 7: Shows effectiveness of twin technique with nebulization on respiratory status of patients with chronic obstructive pulmonary disease and bronchiectasis with their age.
Figure 8: Shows the effectiveness of twin technique with nebulization on respiratory status of patients with chronic obstructive pulmonary disease and bronchiectasis with their unhealthy habits.
Discussion
Being the fourth leading cause of death globally COPD remains as one of the challenges to medical field. Another equally traumatizing respiratory disease is Bronchiectasis which can lead to serious health problems, such as respiratory failure, atelectasis and heart failure. To combat these diseases the medicine needs to reach the lungs without delay. Hence the use of nebulizers has been recommended for easy and efficient travel of the drugs to the places of interest. Hence in the present study nebulizers were used to treat COPD and bronchiectasis patients.
The efficacy of nebulization twin technique was not altered by age, educational status, religion, habitat, exercise activity, use of alternative medicine, use of inhalation device, history of allergy, unhealthy habits, stature of body, employment status, place of work or family income. Irrespective of the differences of the patients in these categories, the nebulization twin technique worked well–as shown in the results. Most of the patients showed adequate respiratory status, improved slight to moderate breathlessness, better O2 saturation, better lung volume expansion and normal breathing pattern post the twin technique nebulization. These results are in agreement with many studies [4,11-14].
Conclusion
In conclusion, the present study shows the efficacy of twin technique nebulization on the respiratory status of the patients with COPD and bronchiectasis. Hence we recommend the use of twin technique nebulization to improve the quality of life of patients suffering with COPD and bronchiectasis.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgements
The encouragement and support from Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India is gratefully acknowledged for providing the laboratory facilities to carry out the research work.
References
- https://www.nhlbi.nih.gov/health-topics/how-lungs-work
- Courtney R. The functions of breathing and its dysfunctions and their relationship to breathing therapy. Int J Osteopathic Med 2009; 12:78-85.
- https://www.uofmhealth.org/
- Bollu V, Guérin A, Gauthier G, et al. Readmission risk in chronic obstructive pulmonary disease patients: Comparative study of nebulized β 2-agonists. Drugs-Real World Outcomes 2017; 4:33-41.
- Tashkin DP. A review of nebulized drug delivery in COPD. Int J Chron Obstruct Pulmon Dis 2016; 11:2585-2596.
- Dolovich MB, Ahrens RC, Hess DR, et al. Device selection and outcomes of aerosol therapy: Evidence-based guidelines: American college of chest physicians/American college of asthma, allergy, and immunology. Chest 2005; 127:335-371.
- Turner MO, Patel A, Ginsburg S, et al. Bronchodilator delivery in acute airflow obstruction. A meta-analysis. Arch Intern Med 1997; 157:1736–1744.
- https://www.nhlbi.nih.gov/health-topics/bronchiectasis
- Currie DC. Nebulisers for bronchiectasis. Thorax 1997; 52:S72–S74.
- https://www.momjunction.com/articles/nebulizers-for-babies_00480275/
- https://www.healthline.com/health/breathing-treatment#for-asthma
- Flick MR, Moody LE. Effect of nebulization of patients with chronic airway obstruction. BMJ 2011; 69:453-458.
- Greene AB, Jackson CL. Terbutaline metered-dose inhalation vs metaproterenol by hand-held nebulization: a comparison in black inner-city COPD patients. J National Med Assoc 1988; 80:393.
- Flick MR, Moody LE, Block AJ. Effect of ultrasonic nebulization on arterial oxygen saturation in chronic obstructive pulmonary disease. Chest 1977; 71:366-370.
Author Info
Department of Nursing, Bharath Institute of Higher Education and Research, Selaiyur, Chennai-600073 Tamil Nadu, IndiaCitation: AR Bharathi, A Study to Assess the Effectiveness of Twin Technique with Nebulization on Respiratory Status among Patients with Chronic Obstructive Pulmonary Disease and Bronchiectasis, J Res Med Dent Sci, 2021, 9(11): 201-212
Received: 19-Jul-2021 Accepted: 08-Nov-2021