Research - (2020) Advances in Dental Surgery
A Study of Vacuum Assisted Negative Pressure Therapy for Wound Healing
Prashant N Mukadam*, Jaykumar J Mandanka, Dip H Joshi, Parth C Shah and Zeel U Khandla
*Correspondence: Prashant N Mukadam, Department of General Surgery, AMCMET Medical College, Ahmedabad, India, Email:
Abstract
Background and objective: Wounds are a major source of morbidity, disability and are associated with increased mortality; therefore, a significant impact on public health and the expenditure of healthcare resources. Vacuum-assisted closure (VAC) uses negative pressure to assist wound healing. Negative pressure drains fluid from the wound, removing the substrate for growth of microorganisms, accelerate granulation tissue formation and promote angiogenesis. The mechanical stimulation of cells by tensile forces may also play a role by increasing cellular proliferation and protein synthesis. Methodology: A total of 50 cases clinically presenting as ulcer between June 2017 and July 2019 were taken for study. Each case was examined clinically in systematic manner as per the proforma. VAC dressing was done and outcome was measured on days 3, 7 and 10. Interpretation and conclusion: In our study VAC therapy enhanced granulation tissue formation leading to better wound healing, and faster recovery. VAC is thus a promising new technology in the field of wound healing with multiple applications in a variety of wounds and can be used in both acute and chronic wounds, salvage procedures or as an adjuvant therapy to improve the results of various surgical procedures.
Keywords
VAC, NPWT, Angiogenesis, Granulation tissue
Introduction
Vacuum-assisted closure (VAC) (also called vacuum therapy, vacuum sealing or topical negative pressure therapy) is a new technique in the challenging field of management of contaminated, acute and chronic wounds. Negative pressure wound therapy (NPWT) also called vacuum-assisted wound closure and refers to wound dressing systems that continuously or intermittently apply sub- atmospheric pressure to the surface of a wound. The application of controlled levels of negative pressure has been shown to accelerate debridement and promote healing in many different types of wounds. The optimum level of negative pressure appears to be around 125 mmHg below ambient and it is believed that negative pressure assists with removal of interstitial fluid, decreasing localised edema and increasing blood flow. This in turn decreases tissue bacterial levels. Despite the significant costs involved, the technique is said to compare favourably in financial terms with conventional treatments in the management of difficult wounds [1].
Mechanisms of action of VAC
Wounds generally heal by primary, where edges are brought into close apposition for example by suturing, or secondary intention, where the wound edges are not opposed and a matrix of small blood vessels and connective tissue must be formed in between in order for keratinocytes to migrate across the surface and reepithelialise the defect. It is a complex, intricate process. The aims of the process can be considered as minimization of blood loss, replacing any deficits with new tissue (granulation) and restoring an intact epithelial barrier as quickly as possible. In order to achieve healing debris must also be removed; any infection controlled, and inflammation eventually cleared. The wound then heals with granulation, remodeling of the connective tissue matrix and finally maturation. The rate of healing may be limited by vascular supply and the capacity of the wound to form new capillaries/matrix. Any disruption in the various processes involved in proliferation, angiogenesis, chemotaxis, migration, gene expression, protein production can lead to a chronic wound.
Local blood flow
Morykwas et al. used needle probe laser Doppler flowometry to show that sub-atmospheric pressures of 125 mm Hg resulted in a fourfold increase in blood flow using an excisional wound model in pigs [2]. This increase in blood flow has also been shown in human burns. These direct effects on dermal vasculature are thought to be mediated by influencing vasomotor mediators. Vacuum Assisted Closure (VAC) is widely used in wound therapies and has been shown to positively affect angiogenesis [3,4].
Mechanical stress
Increasing mechanical stress in vitro causes an increase in cellular activity, the nature of which varies with the cell type and methodology. Accelerated cell cycling and DNA synthesis have been seen. Experimental evidence from model systems also suggests that mechanical forces can result in increased fibrogenesis in cutaneous wound models [5].
Granulation tissue formation
TNP treated wounds showed increased granulation tissue formation compared with the controls by 63% and 103.4% (continuous and intermittent suction respectively), although it is not known what effect contraction played to change the size of these wounds [6].
Bacterial colonization
Studies using swine wounds inoculated with a human isolate of Staphylococcus aureus and a swine isolate of Staphylococcus epidermidis that were treated with TNP or controlled moist saline dressing showed a more rapid decline in bacterial levels in the TNP treated wounds [7].
Edema reduction and exudate management
Clinically VAC removes large amounts of fluid from wounds especially acute burns. The resulting reduction in oedema is thought to aid in the enhancement of blood and nutrient flow into the wound. Removal of fluid prevents a buildup of inflammatory mediators and encourages diffusion of further nutrients into the wound. This is all beneficial to the healing process especially in the case of chronic wounds where it has been hypothesized that an imbalance of metalloproteinases can inhibit healing.
Objectives of the Study
To study the effect of vacuum therapy on wound healing.
To evaluate changes in clinical parameters of wound after vacuum therapy.
To assess effect on duration of hospital stay due to vacuum therapy.
Methodology
Source of data
50 Patients for study of vacuum assisted negative pressure therapy were selected from the wards of LG Hospital, Maninagar, according to inclusion and exclusion criteria between June 2017 and October 2019. A predesigned proforma was used to collect the information for individual case.
Sample size: 50 Cases.
Inclusion criteria
All large ulcers over body which are not connected with body cavity–either healthy or unhealthy.
Ulcers >2 inch (5cm) in size in diameter.
Age >16 years.
Exclusion criteria
Fistula to organ or body cavity.
Malignancy in the wound.
Osteomyelitis–localized.
Necrotic tissue in wound.
Small healthy ulcer.
Post burn ulcer.
Major cardiorespiratory disease.
Sequence of procedure
Wound preparation
Any dressings from the wound was removed and discarded. A culture swab for microbiology was taken before wound irrigation with normal saline. Surgical debridement was done, and adequate hemostasis achieved.
Placement of foam
Sterile, open-cell foam dressing was gently placed into the wound cavity.
Sealing with drapes
The site was then sealed with an adhesive drape ensuring that the drapes covered the foam and tubing and at least three to five centimeters of surrounding healthy tissue.
Application of negative pressure
Controlled pressure was uniformly applied to all tissues on the inner surface of the wound using centralized vacuum pump, which could deliver either continuous or intermittent pressures, ranging from 50 to 125 mm Hg. The foam dressing compressed in response to the negative pressure. The pressure was applied continuously for the first 48 hours and changed as required thereafter. The outcome was measured using area of wound covered with granulation tissue, and its color and consistency (Figure 1).
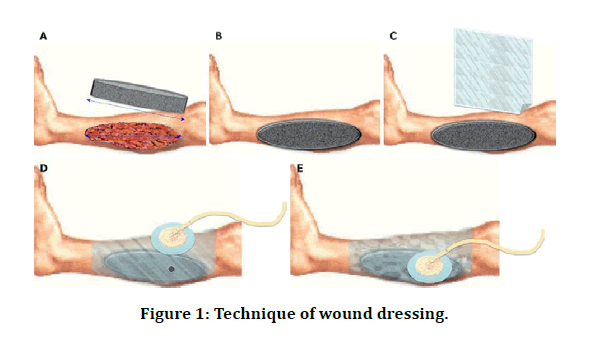
Figure 1: Technique of wound dressing.
Observation
Most of the patients presenting with wounds were in the 6th decade of life 13(26%), followed by the 5th decade 10(20%).
Wounds were more common in males 30 cases (60%) than in females.
Wounds were most located in the foot 30(60%) followed by the leg 18(36%), Back 3(6%), forearm 2(4%) and abdomen 1(2%) (Figure 2).
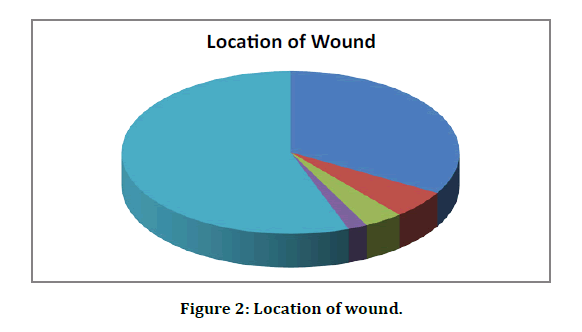
Figure 2: Location of wound.
Based on etiology of wounds, which were determined by history and clinical examination, wounds were divided into Traumatic, Diabetic and post-diabetic. A major portion 24(48%) of cases fell into Diabetic group and 10(20%) into post-debridement and 8(16%) into trauma group.
Most common organism cultured from the wounds was Staphylococcus aureus 22(44%) (Table 1).
| Organisms cultured from wound | No. of Cases |
|---|---|
| No Growth | 12 (24%) |
| Staphylococcus | 22 (44%) |
| Pseudomonas | 4 (8%) |
| Escheria Coli | 6 (12%) |
| Proteus | 6 (12%) |
| Total | 50 |
Table 1: Organisms cultured from wound
Following V.A.C. Dressing for 3-7 days, most of the wound show’s improvement in terms of decreased wound surface area (Figure 3), layer of granulation tissue covering wound and quantity of exudate (Table 2).
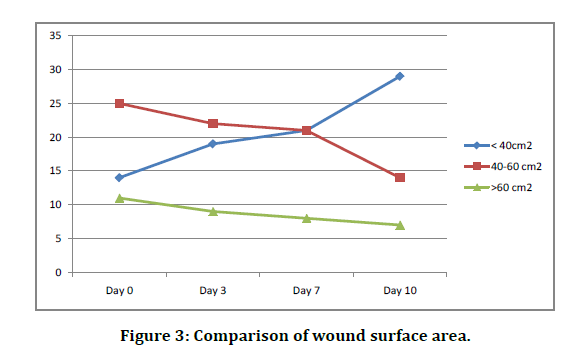
Figure 3: Comparison of wound surface area.
| Days after V.A.C. Application | Number of cases | ||
|---|---|---|---|
| <40 cm2 | 40-60 cm2 | >60 cm2 | |
| Before VAC application | 14 | 25 | 11 |
| Day 3 | 19 | 22 | 9 |
| Day 7 | 21 | 21 | 8 |
| Day 10 | 29 | 14 | 7 |
Table 2: Comparison of wound surface area.
Comparison of colour of granulation tissue
Initially 40 patients (80%) were having wounds with pale granulation tissue and minimal slough. After application of vac dressing for 3 to 10 days, 94% (47) patients are having bright red granulation tissue in the floor with no slough (Figure 4 and Table 3). Comparison of duration of hospital stay before definitive surgical management is shown Table 4.
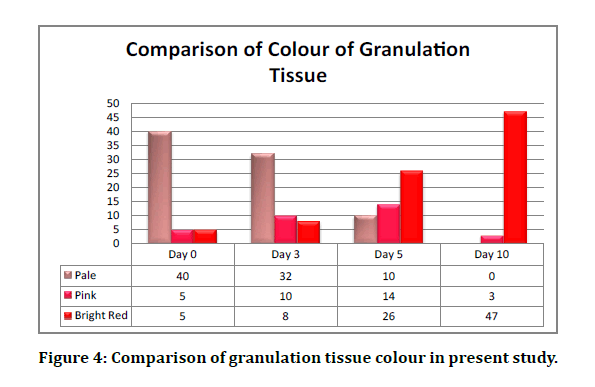
Figure 4: Comparison of granulation tissue colour in present study.
| Days of V.A.C. | Number of Cases | ||
|---|---|---|---|
| Application | Pale with slough | Pink | Bright Red |
| Before VAC application | 40 | 5 | 5 |
| Day 3 | 32 | 10 | 8 |
| Day 5 | 10 | 14 | 26 |
| Day 10 | 0 | 3 | 47 |
Table 3: Comparison of colour of granulation tissue.
| Dressing Method | Duration of Hospital Stay before definitive surgical management |
|---|---|
| Conventional Techniques | 29 Days |
| V.A.C. Application | 12 Days |
Table 4: Duration of hospital stay.
Complications after vac dressing
There was only one case of developing gangrene over great toe requiring amputation. However, this complication might have resulted from pre- VAC therapy ischemic changes. This complication may not be causally related to VAC dressing.
Discussion
Delayed wound healing is a significant health problem and a challenge in the community setting particularly in older adults, often requires daily or more frequent hospital visits. With conventional wound-healing methods, it may take several months to heal the wound. Vacuum-assisted closure (VAC) therapy has been developed as an alternative to the standard forms of wound management, which incorporates the use of negative pressure to optimize conditions for wound healing and requires fewer painful dressing changes [8].
Negative pressure therapy is an expensive treatment modality, and, because the costs are high, a recent consensus report suggests that use as a first-line therapy is inappropriate.
However, others suggest that negative pressure therapy has the potential for saving money if it is used on the “right patient, the right wound, at the right time.” The use of negative pressure therapy has been proposed as a novel method of manipulating the chronic wound environment to assist and accelerate wound healing. Although most studies were probably too small to detect significant differences between wounds managed by conservative dressings and by VAC, some did show VAC to result in better healing than standard methods, with few serious complications. VAC appears to be a promising alternative for management of wounds. VAC was also more effective at treating various chronic and complex wounds, with a significantly greater reduction in wound volume, depth, and treatment duration for VAC. It has the potential to reduce health care costs, for both hospital and patient, and enhance patient satisfaction and quality of life [9].
In our study, following VAC therapy, wound scoring was done with scores from 1-7given for area of granulation tissue, color and consistency of granulation tissue. The wounds following VAC therapy can be considered for skin graft. In the present study, >70% cases showed considerable improvement following a week of VAC therapy. The use of sub-atmospheric pressure dressings, available commercially as the VAC device, has been shown to be an effective way to accelerate healing of various wounds. The optimal subatmospheric pressure for wound healing appears to be approximately 125 mm Hg. VAC has significantly increased the skin graft success rate when used as a bolster over the freshly skin-grafted wound. VAC is generally well tolerated and, with few contraindications or complications, is fast becoming a mainstay of current wound care.
Conclusion
This study includes 50 patients with acute or chronic wounds fulfilling inclusion and exclusion criteria. VAC or NPWT therapy is an excellent alternative modality of treatment of acute or chronic large non-healing wounds. VAC dressing increases the process of wound healing by favouring local environment by increasing blood flow and reducing slough and exudates from wound continuously, increases the formation of granulation tissue formation rate leads to contraction of wound and reduces the surface area of wound, rapidly reduces depth of wound by increasing formation of new granulation tissue. In this way the VAC therapy causes rapid wound healing, reduces the number of changes of dressing and reduces the time of hospital stay before definitive surgery for covering wound can be planned. VAC dressing is associated with minimal complications like mild and dragging pain and minor bleeding or oozing from the newly formed granulation tissue. Based on the data from the present study and other studies available, VAC appear to result in better and rapid healing, with few serious complications, and thus VAC is a better option of wound management technique.
References
- Eginton MT, Brown KR, Seabrook GR, et al. A prospective randomized evaluation of negative pressure wound dressings for diabetic foot wounds. Ann Vasc Surg 2003; 17:645-649.
- Morykwas MJ, Argenta LC, Shelton-Brown EI, et al. Vacuum-assisted closure: a new method for wound control and treatment: Animal studies and basic foundation. Ann Plast Surg 1997; 38:553–562.
- Barbul A, Efron DT. Wound healing. Brunicardi FC. Schwartz principles of surgery. 9th Edn New York. McGraw Hill 2010; 209-233.
- Galiano RD, Mustoe TA. Wound healing. Mulholland, Michael W, Lillemoe, et al. In greenfield's surgery: Scientific principles and practice. 4th Edn Philadelpihia Lippincott Williams and Wilkins 2006.
- Lazarus GS, Cooper DM, Knighton DR, et al. Definitions and guidelines for assessment of wounds and evaluation of healing arch dermatol. Wound Repair Regeneration 1994; 130:489-493.
- Lionelli GT, Lawrence WT. Wound dressings. Surg Clin N Am 2003; 83:192-195.
- Bowler PG. Wound pathophysiology, infection and therapeutic options. Annals Med 2002; 34:419-427.
- Lee HJ, Kim JW, Oh CW, et al. Negative pressure wound therapy for soft tissue injuries around the foot andankle. J Orthop Surg Res 2009; 4:14.
- Lazarus GS, Cooper DM, Knighton DR, et al. Definitions and guidelines for assessment of wounds and evaluation of healing. Arch Dermatol 1994; 130:489-493.
Author Info
Prashant N Mukadam*, Jaykumar J Mandanka, Dip H Joshi, Parth C Shah and Zeel U Khandla
Department of General Surgery, AMCMET Medical College, Ahmedabad, IndiaCitation: Prashant N Mukadam, Jaykumar J Mandanka, Dip H Joshi, Parth C Shah, Zeel U Khandla, A Study of Vacuum Assisted Negative Pressure Therapy for Wound Healing, J Res Med Dent Sci, 2020, 8 (7): 350-354.
Received: 21-Oct-2020 Accepted: 06-Nov-2020 Published: 13-Nov-2020
