Research - (2021) Volume 9, Issue 6
A Study of Post-Operative Wound Infections in Sree Balaji Medical College and Hospital
Arvind Gilbert J and P Sasikumar*
*Correspondence: P Sasikumar, Department of General Surgery, Sree Balaji Medical College and Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India, Email:
Abstract
Background: Postoperative wound infections become a challenge in certain patients and may cause excessive comorbidity, mortality and costs. The aim of this study was to determine the incidence of postoperative wound infections in emergency abdominal surgeries in patients admitted to Sree Balaji Medical College and Hospital, Chennai. Method: In this study 120 patients were included who underwent emergency abdominal surgeries. Data concerning type of wound, various surgical procedures, length of surgery, age distribution, sex incidence, preoperative preparation, antibiotic prophylaxis, co morbid conditions, common microorganisms, antibiotic sensitivity, and timing of presentation of SSI were obtained and interpreted, statistically. Results: This study showed that abdomen injury (80%), aging (20%) and duration of surgery (>3.5h), prolonged anesthesia provoked the chances of SSI. There was no correlation of gender with SSI development. Burst abdomen, abscess with suppuration, enterocutaneous fistula and incisional hernia were most common complications associated with post-operative patients. The study also inferred that the proper diabetic management would reduce SSI risk. Conclusion: The present study revealed that the need of strategic goal for effective post-operative wound management based important factors such as host, environmental, and microorganism characteristics before doing any surgery. The antibiotics usage warrants for their resistance and the hospitals should establish an antibiotic policy for surgery patients.
Keywords
Wound infections, Abdominal surgeries, Antibiotic prophylaxis, Abdomen injury, Anesthesia
Introduction
Wound infection is a common postoperative complication which causes significant postoperative morbidity and mortality and prolongs hospital stay. Infection was accepted as an inevitable sequalae of surgery a century ago. The infection rate which was about 75-80% has now dropped to less than 10%. Yet today infections accompanying surgical procedures contribute significantly to morbidity and mortality. Although the total elimination of wound infection is not possible, a reduction in the infection rate to a minimal level could have significant benefits in terms of both patient comfort and medical resources used. Clear understanding of pathogens and their pathogenicity, advances in the field of asepsis, the advent of antibiotics and reliable suture materials have furnished the surgical artillery in combating infection. Hence a constant awareness of the everpresent threat of infection must be a way of life for the entire surgical fraternity [1-29].
To determine incidence of postoperative wound infections in emergency abdominal surgeries and to identify the risk factors for appropriate wound management. To identify the common wound causing agents in post-operative abdominal surgery in SBMCH. To study the role of prophylactic antibiotics in reducing surgical site infection.
Materials and Methods
This prospective study was carried out in the Surgical Units-I and II of Sree Balaji Hospital, Chrompet, Chennai on 120 patients who underwent emergency abdominal surgeries between July 2014 to November 2015. Patients undergoing emergency abdominal surgeries received post-operative antibiotic therapy also parentally. In this study, pus / wound swab was sent for SSI confirmation and for SSI- patients, 5ml sample was taken in a sterile container for further process. The relevant information was processed in a specially designed proforma along with their biodata, clinical features, the possible risk factors, diagnosis, complications which included wound infections, the organisms which were isolated with their antibiograms, hospital stay and the outcome. The statistical analysis was carried using SPSS, version 10.0 on computer.
Inclusion criteria
✓ Age between 25-60 years.
✓ Patients of either sex.
✓ Patients undergoing contaminated and dirty surgery as emergency.
✓ Comorbidities: Anemia, type 2 diabetes mellitus, Smoking.
Exclusion criteria
✓ Age less than 25 years.
✓ HbsAg/HIV positive individuals.
✓ Patients operated on elective basis.
Results and Discussion
The prevalence of emergency abdominal wounds in post-operative patients were analysed in the present study. Of the 120 studies patients, 104 (86.6%) had healed wounds and only, 16 patients (13.4%) developed post-operative SSI. The study also showed that contaminated wound was the more prevalence in patients (69.16%) than the dirty wounds (30.83%) and the dirty wounds were more prone for further infections (Table 1 and Figure 1).
| Sl. No |
Type of wound | Total cases |
Infected cases |
Percentage(%) infected |
|---|---|---|---|---|
| 1 | Contaminated | 83 | 5 | 0.06 |
| 2 | Dirty | 37 | 11 | 29.72 |
Table 1: Type of wounds commonly found in post-operative abdominal patients.
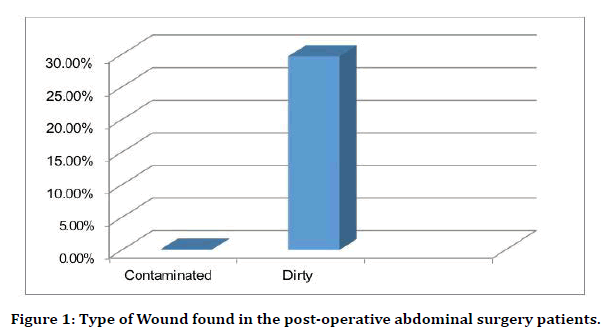
Figure 1. Type of Wound found in the post-operative abdominal surgery patients.
Type of surgery
The study also revealed that the type of surgery was the major factors that contributed for occurrence of wounds. In this study, severe risk for SSI was associated with penetrating trauma abdomen followed by bowel perforation and obstructed ventral hernia (Table 2 and Figure 2) and concordance with previous results [30].
| Sl. no : | Surgical procedure (for) |
Total cases | Infected case(s) | Percentage infected (%) |
|---|---|---|---|---|
| 1 | Appendicular pathology | 64 | 2 | 0.03 |
| 2 | Duodenal perforation |
12 | 1 | 0.08 |
| 3 | Penetrating injury abdomen |
5 | 4 | 80 |
| 4 | Blunt injury abdomen |
6 | 1 | 0.16 |
| 5 | Large bowel obstruction |
10 | 1 | 10 |
| 6 | Strangulated ventral hernia |
12 | 2 | 0.16 |
| 7 | Obstructed ventral hernia |
4 | 2 | 50 |
| 8 | Gastric perforation |
3 | 1 | 33.33 |
| 9 | Ileal perforation | 4 | 2 | 50 |
Table 2: Association of type of wounds and classes of surgery.
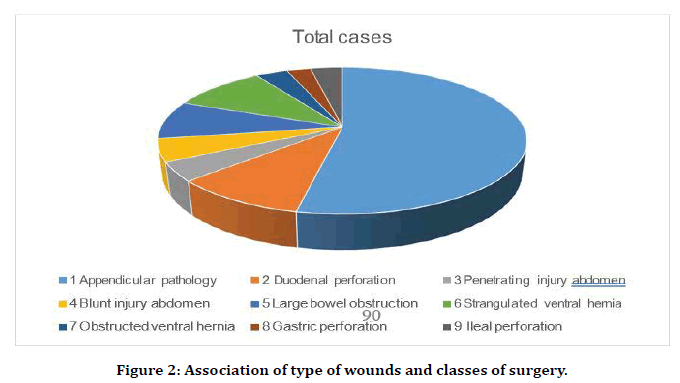
Figure 2. Association of type of wounds and classes of surgery.
Duration of surgery
The duration of surgery was also a significant factor for wound occurrence. The present study revealed that proportional relationship with the higher duration and risk for SSI wounds. Prologed surgeries (>3h) had definite risk for wounds (Table 3 and Figure 3) and the result was similar for the study of Simon et al. [31].
| Sl no | Duration | Total cases | Infected cases | Percentage (%) |
|---|---|---|---|---|
| 1 | 1 – 2 hours | 35 | 1 | 0.02 |
| 2 | 2 – 3 hours | 45 | 6 | 13.33 |
| 3 | > 3hours | 40 | 9 | 22.5 |
Table 3: Duration of surgery and risk for wounds.
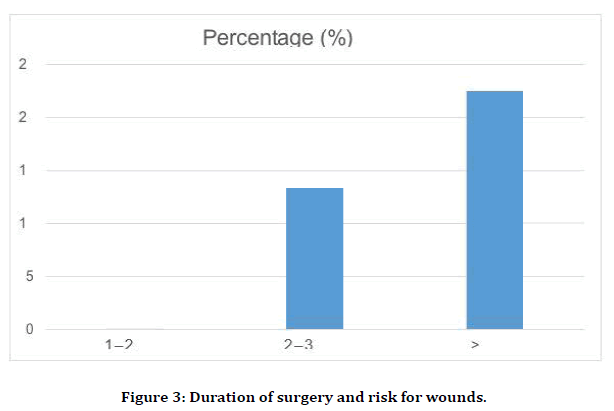
Figure 3. Duration of surgery and risk for wounds.
Age distribution and wound occurrence
The patient’s age was also one of the major risk factors for the occurrence of the wounds. The study revealed that the elder patients were more prone to wound occurrence than the younger ones (Table 4 and Figure 4) and these results were concordance with Yunzhou, et al. [32].
| Sl no | Age group (in years) | Total cases | Infected cases | Percentage (%) |
|---|---|---|---|---|
| 1 | 25 - 35 | 25 | 1 | 0.04 |
| 2 | 36-50 | 40 | 4 | 10 |
| 3 | 51 - 60 | 55 | 11 | 20 |
Table 4: Age distribution and wounds occurrence.
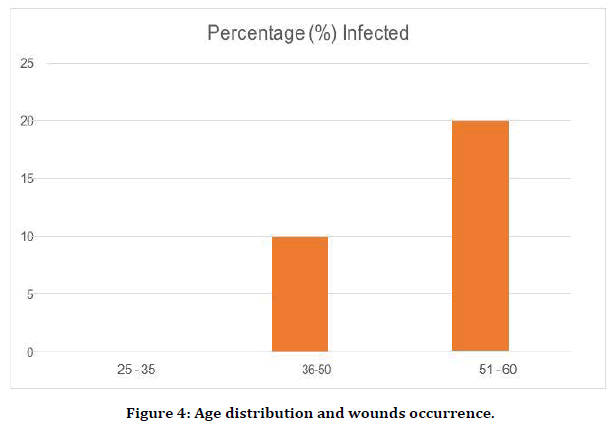
Figure 4. Age distribution and wounds occurrence.
Gender
In this study, we found that the sex is not the major factor for risk contribution on surgery wounds. Our study revealed that there is same risk ration for both the male and female and all of the studied patients had more or less same incidence of SSI (Table 5 and Figure 5). Similarly, Alkaaki et al. [33] also reported.
| Sl no | Gender | Total cases | Infected cases | Percentage (%) |
|---|---|---|---|---|
| 1 | Male | 74 | 9 | 12.16 |
| 2 | Female | 46 | 7 | 15.21 |
Table 5: Incidence of wounds on abdominal surgery and gender of the patients.
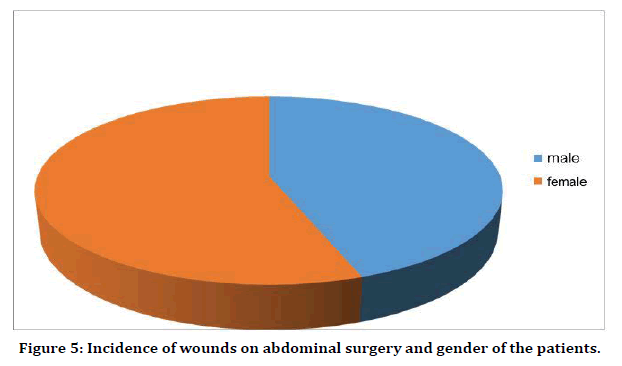
Figure 5. Incidence of wounds on abdominal surgery and gender of the patients.
Pre-operative preparation (hair removal)
The study revealed that the hair removal prior to the surgery (before a hour) had reduced the wounding risk. There was a least correlation of SSI wounds and preoperative hair removal (Table 6 and Figure 6).
| Sl no | Timing of hair removal |
Total cases | Infected cases | Percentage infected (%) |
|---|---|---|---|---|
| 1 | 1 hour before surgery |
55 | 2 | 0.03 |
| 2 | 1- 3 hours before surgery |
39 | 4 | 10.25 |
| 3 | 3 – 6 hours before surgery |
26 | 10 | 38.46 |
Table 6: Preoperative hair removal and wound occurrence.
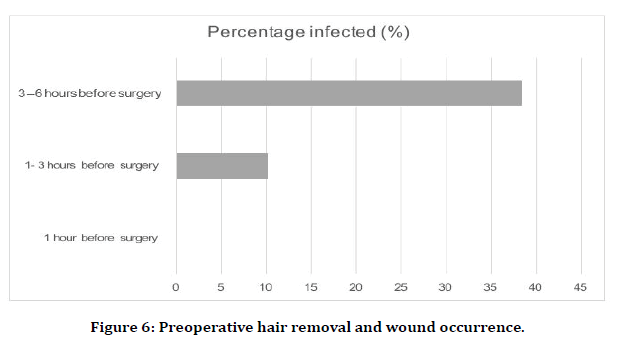
Figure 6. Preoperative hair removal and wound occurrence.
Antibiotic prophylaxis
Prophylactic antibiotic therapy was given for all cases taken into this study. However, there was no significant influence of timing of administering the drug in the incidence of wound infection (Table 7 and Figure 7) [34].
| Sl no | Antibiotic prophylaxis | Total cases | Infected cases | Percentage (%) |
|---|---|---|---|---|
| 1 | 1 hour before surgery | 43 | 6 | 13.95 |
| 2 | 1 – 2 hours before surgery | 51 | 6 | 11.76 |
| 3 | 2 to 4 hours before surgery | 26 | 4 | 15.38 |
Table 7: Antibiotic prophylaxis and wound occurrence in abdominal surgery patients.
Figure 7. Antibiotic Prophylaxis and wound occurrence in abdominal surgery patients.
Comorbid conditions
Usually, comorbidities increase the risk of wounds for abdominal surgery patients (Table. 8 and Figure. 8). There was increased incidence of post-operative wound infection in patients with anemia, and diabetes mellitus and this result was concordance with the view of previous study by Derek et al. [35]. This study also showed that patients with comorbid conditions like Smoking, DM and anemia had higher incidence than those without. Several studies have shown a higher incidence of wound infection amongst smokers than in non-smokers. It was proposed that smoking has a detrimental effect on the tissue oxygenation, there by impairing the reparative processes of wound healing and the neutrophil defense against surgical pathogens. Anaemia itself is not an established factor for postoperative wound infection. However, a higher incidence of postoperative wound infection was noted with initial low haemoglobin levels. Others postulated this in 1993.Diabetes mellitus is also a proven risk factor as it hampers the vasculature leading to reduced blood flow and oxygenation to the tissues. Study conducted by Masood Ahmed in Karachi proves the finding in this study (Table 8 and Figure 8).
| Sl no | Comorbidity | Total cases | Infected cases | % infected |
|---|---|---|---|---|
| 1 | Anemia (Hb<8 gm%) | 49 | 7 | 14.28 |
| 2 | Diabetes mellitus | 36 | 6 | 16.66 |
| 3 | Smoking | 35 | 3 | 0.08 |
Table 8: Comorbidities and risk of wounds in abdominal surgery patients.
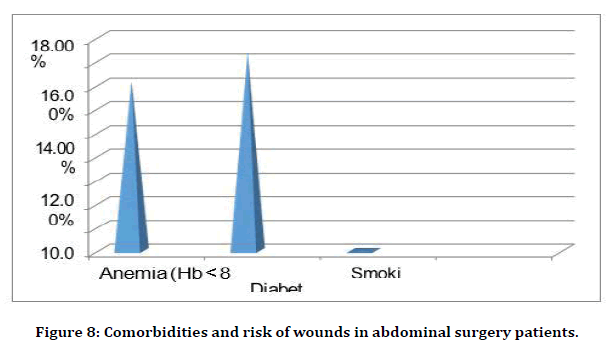
Figure 8. Comorbidities and risk of wounds in abdominal surgery patients.
Bacteriological surveillance
Microbial occurrence is one of the major risk factors for SSI occurrence in any type of surgery. Our results also revealed that the bacterial infections increased the risk of wound occurrence like previous study ````36]. Our studyalso revealed that the gram-positive bacteria increase the wound risk than the gramnegative ones (Table 9 and Figure 9).
| SL NO | Name of organism | Infected case |
% of cases infected |
|---|---|---|---|
| 1 | Staphylococcus aureus | 6 | 37.5 |
| 2 | Staphylococcus epidermidis | 2 | 12.5 |
| 3 | Beta haemolytic streptococci | 3 | 18.75 |
| 4 | Escherichia coli | 2 | 12.50 |
| 5 | Proteus mirabilis | 1 | 6.25 |
| 6 | Pseudomonas aeruginosa | 1 | 6.25 |
| 7 | Klebsiella | 1 | 6.25 |
Table 9: Bacteriological surveillance.
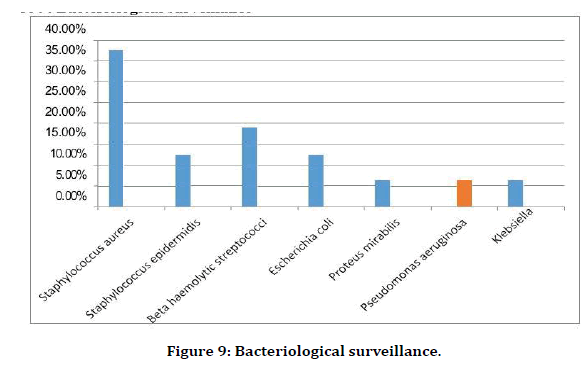
Figure 9. Bacteriological surveillance.
Antibiotic sensitivity
The patient’ antibiotic sensitivity was the major risk factor for wound occurrence on abdominal surgery (Table 10). In this study most of the organisms were sensitive to Ciprofloxacin, Amikacin, and gentamycin in descending order of frequency.
| Name of organism | Ciprofloxacin | Amoxycillin+ clavulanate | Amikacin | Gentamycin | cephalexin | cefotaxime | norfloxacin | cefixime | ampicillin |
|---|---|---|---|---|---|---|---|---|---|
| Staphylococcus aureus | +++ | ++ | + | + | |||||
| Beta haemolytic streptococci | ++ | ++ | +++ | + | + | ||||
| Staphylococcus epidermidis | ++ | + | ++ | ++ | |||||
| Proteus | + | +++ | + | + | |||||
| Escherichia coli | + | ++ | + | + | |||||
| Klebsiella | + | ++ | + | ||||||
| Pseudomonas | + | ++ | + | + | + | + |
Table 10: Antibiotic Sensitivity and wound occurrence in abdominal surgery patients.
Time of presentation of surgical site infection
In this study nearly 50% of the patients who developed SSI manifested with fever (>99.6-degree Fahrenheit) or pain in the wound at the time of presentation of SSI (Table 11).
| Time of Presentation of SSI | Number | Percentage |
|---|---|---|
| Before first dressing with fever>99.6oF or pain in the wound | 7 | 43.75 |
| Abscess, cellulitis or discharge noted at 1st week postoperatively | 4 | 25 |
| Abscess, cellulitis or discharge noted at 2nd week postoperatively | 3 | 18.75 |
| Abscess, cellulitis or discharge noted at 3rd week postoperatively | 2 | 12.5 |
| Abscess, cellulitis or discharge noted at 4th week postoperatively | _ | _ |
Table 11: Time of presentation of SSI in abdominal surgery patients.
Complications
Of the 16 patients who developed SSI, 12 developed complications namely Abscess with suppuration, Burst Abdomen enterocutaneous fistula and incisional hernia (Table 12 and Figure 10) and the remaining 25 % of the patients, the wound healed by secondary intention.
| Sl no | Complication | No. of cases | % |
|---|---|---|---|
| 1 | Burst Abdomen | 4 | 33.33 |
| 2 | Abscess with suppuration | 3 | 25 |
| 3 | Enterocutaneous fistula | 2 | 16.67 |
| 4 | Incisional hernia | 3 | 25 |
Table 12: Complications and occurrence of wounds.
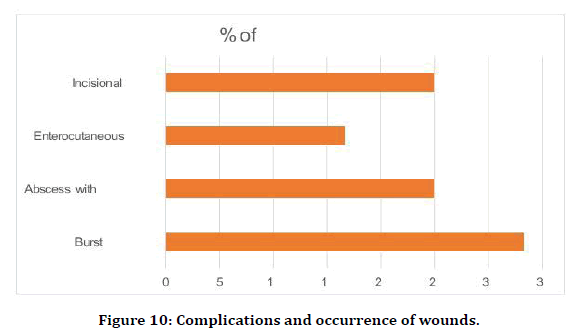
Figure 10. Complications and occurrence of wounds.
Conclusion
In summary, the present study showed that the early diagnosis and strategic therapy would reduce the post-operative wounds. The study showed that the age of the patients, surgery duration, comorbidities such as diabetes and optimal anti biotic regime were important players. If anaerobes are isolated in necrotizing fasciitis an early and aggressive second look is necessary. At the same time, however, the basis of timely therapy is a high level of suspicion with no diagnostic tool being superior to clinical judgment.
References
- Mangram AJ, Horan TC, Pearson ML, et al: Guideline for prevention of surgical site infection, 1999. Hospital Infection ControlPractices Advisory Committee. Infect Control Hosp Epidemiol 20:250, 1999.
- Martone WJ, Nichols RL: Recognition, prevention, surveillance, and management of surgical site infections. Clin Infect Dis 33:S67,200
- Kobayashi M, Mohri Y, Inoue Y, et al: Continuous follow-up of surgical site infections for 30 days after colorectal surgery. World J Surg 32:1142, 2008.
- Blumetti J, Luu M, Sarosi G, et al: Surgical site infections after colorectal surgery: Do risk factors vary depending on the type of infection considered? Surgery 142:704, 2007.
- Konishi T, Watanabe T, Kishimoto J, et al: Elective colon and rectal surgery differ in r isk factors for wound infection: Results of prospective surveillance. Ann Surg 244:758, 2006Perencevich EN, Sands KE, Cosgrove SE, et al: Health and economic impact of surgical site infections diagnosed after hospital discharge. Emerg Infect Dis 9:196, 2003.
- Page CP, Bohnen JM, Fletcher JR, et al: Antimicrobial prophylaxis for surgical wounds: Guidelines for clinical care. Arch Surg128:79, 1993.
- Cohn SM, Giannotti G, Ong AW, et al: Prospective randomized trial of two wound management strategies for dirty abdominal wounds. Ann Surg 233:409, 2001
- Margenthaler JA, Longo WE, Virgo KS, et al: Risk factors for adverse outcomes after the surgical treatment of appendicitis in adults. Ann Surg 238:59, 2003.
- McManus LM, Bloodworth RC, Prihoda TJ, et al: Agonist-dependent failure of neutrophil function in diabetes correlates with extent of hyperglycemia. J Leukoc Biol 70:395, 2001.
- Trick WE, Scheckler WE, Tokars JI, et al: Modifiable risk factors associated with deep sternal site infection after coronary artery bypass grafting. J Thorac Cardiovasc Surg 119:108, 2000
- Russo PL, Spellman DW: A new surgical-site infection risk index using risk factors identified by multivariate analysis for patients undergoing coronary artery bypass graft surgery. Infect Control Hosp Epidemiol 23:372, 2002.
- Greif R, Akca O, Horn EP, et al: Supplemental perioperative oxygen to reduce the incidence of wound infection. N Engl J Med 342:161, 2000.
- Pryor KO, Fahey TJ 3rd, Lien CA, et al: Surgical site infection and the routine use of perioperative hyperoxia in a general surgical population: A randomized controlled trial. JAMA 291:79, 2004.
- Melling AC, Ali B, Scott EM, et al: Effects of preoperative warming on the incidence of wound infection after clean surgery: A randomized controlled trial. Lancet 358:876, 2001.
- Gregor S, Maegele M, Sauerland S, et al: Negative pressure wound therapy: A vacuum of evidence? Arch Surg 143:189, 2008
- Grubbs BC, Statz CL, Johnson EM, et al: Salvage therapy of open, infected surgical wounds: A retrospective review using Techni-Care. Surg Infect 1:109, 2000.
- Gregor S, Maegele M, Sauerland S, et al: Negative pressure wound therapy: A vacuum of evidence? Arch Surg 143:189, 2008.
- Winter GD: Formation of the scab and the rate of epithelialisation of superficial wounds in the skin of the young domestic pig. Nature 193:293, 1962.
- Gulliver G (ed): The Works of John Hunter. London: Longman, 1837.
- Feiken E, Romer J, Eriksen J, et al: Neutrophils express tumor necrosis factor-alpha during mouse skin wound healing. J Invest Dermatol 105:120, 1995.
- Dovi JV, He L-K, DiPietro LA: Accelerated wound closure in neutrophil-depleted mice. J Leukoc Biol 73:448, 2003.
- Leibovich SJ, Ross R: The role of the macrophage in wound repair. A study with hydrocortisone and antimacrophage serum. Am J Pathol 78:71, 1975.
- DiPietro LA: Wound healing: The role of the macrophage and other immune cells. Shock 4:233, 1995
- Zabel DD, Feng JJ, Scheuenstuhl H, et al: Lactate stimulation of macrophage-derived angiogenic activity is associated with inhibition of Poly(ADP-ribose) synthesis. Lab Invest 74:644, 1996
- Schäffer MR, Barbul A: Lymphocyte function in wound healing and following injury. Br J Surg 85:444, 1998.
- Efron JE, Frankel HL, Lazarou SA, et al: Wound healing and T-lymphocytes. J Surg Res 48:460, 1990.
- Barbul A, Breslin RJ, Woodyard JP, et al: The effect of in vivo T helper and T suppressor lymphocyte depletion on wound healing. Ann Surg 209:479, 1989.
- Rezzonico R, Burger D, Dayer JM: Direct contact between T lymphocytes and human dermal fibroblasts or synoviocytes down-regulates types I and III collagen production via cell-associated cytokines. J Biol Chem 273:18720, 1998.
- Grotendorst GR: Chemoattractants and growth factors, in Cohen K, Diegelmann RF, Lindblad WJ (eds): Wound Healing, Biochemical and Clinical Aspects. Philadelphia: WB Saunders, 1992, p 237.
- Hemmati, H., Kazemnezhad-Leili, E., Mohtasham-Amiri, Z., Darzi, A. A., Davoudi-Kiakalayeh, A., Dehnadi-Moghaddam, A., & Kouchakinejad-Eramsadati, L. (2013). Evaluation of chest and abdominal injuries in trauma patients hospitalized in the surgery ward of poursina teaching hospital, guilan, iran. Archives of trauma research, 1(4), 161.
- Li, Simon, et al. "Incidence, risk factors, and outcomes of acute kidney injury after pediatric cardiac surgery–a prospective multicenter study." Critical care medicine 39.6 (2011): 1493.
- Fan, Yunzhou, et al. "The incidence and distribution of surgical site infection in mainland China: a meta-analysis of 84 prospective observational studies." Scientific reports 4.1 (2014): 1-8.
- Alkaaki, Aroub, et al. "Surgical site infection following abdominal surgery: a prospective cohort study." Canadian Journal of Surgery 62.2 (2019): 111.
- JAMA Surg. 2013;148(7):649-657. doi:10.1001/jamasurg.2013.134
- Masden, Derek, et al. "Negative pressure wound therapy for at-risk surgical closures in patients with multiple comorbidities: a prospective randomized controlled study." Annals of surgery 255.6 (2012): 1043-1047
- Aga, Emil, et al. "Surgical site infections after abdominal surgery: incidence and risk factors. A prospective cohort study." Infectious Diseases 47.11 (2015): 761-767.
Author Info
Arvind Gilbert J and P Sasikumar*
Department of General Surgery, Sree Balaji Medical College and Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Arvind Gilbert J, P Sasikumar, A Study of Post-Operative Wound Infections in Sree Balaji Medical College and Hospital, J Res Med Dent Sci, 2021, 9 (6):464-472.
Received: 02-Apr-2021 Accepted: 27-Apr-2021
