Research - (2021) Volume 9, Issue 8
A Study of Ocular Manifestations in Leprosy
*Correspondence: PM Palanimuthukumaran, Department of Anatomy, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, India, Email:
Abstract
Majority had brow and eyelash madarosis constituting 33%, Lagophthalmos 10.6%, Exposure Keratitis 9.3% and chronic dacroyocystitis 1.3%. Among this the total numbers of male patients were 28 and total number of female patients was 5, reflecting the male preponderance. The higher incidence of leprosy in male population can be attributed to higher rate of exposure and hence increased risk of infection. Maximum incidence was seen in paucibacillary group and the incidence of paucibacillary in the group with time lag of 19 to 24 months is low (4.1%) compared to that of time lag of <6 months (45.2%). Of the total study group, nearly 47% of population had no manifestations, indicating the efficacy of early detection of disease.
Keywords
Paucibacillary, Keratitis, DacroyocytitisIntroduction
Leprosy manifests itself in two polar forms, namely tuberculoid leprosy and Lepromatous leprosy with border line and indeterminate forms lying in between the two ends of a long spectrum of the disease. This study is designed to measure the prevalence, range and severity of ocular involvement in leprosy patients, to relate this to disease type, duration and early institution of multi-drug regime [1-2].
Materials and Methods
This study was carried out in Sree Balaji Medical College and Hospital, Chromepet. Total number of patients studied was 75 out of which 53 were males and 22 were females. A detailed ophthalmological examination was performed out by torch and slit lamp to ascertain the anterior segment involvement. Fundus examination was performed after dilating the patient with Tropicamide 0.5% and phenylephrine 0.5%. Visual acuity for distant vision was tested with Snellen's chart and for near vision with Jaegger’s chart [3]. Smears were taken from skin lesions and ear lobules and grading with bacteriological index was done. Routine laboratory investigations like complete haemogram, ESR, Urine routine, Stool examination and VDRL were carried out to rule out other possible associated causes of ocular lesions.
Results
Maximum patients examined were of age group of more than 61 years, which constituted to 44% of the study group. Among this the total number of male patients was 28 and total number of female patients was 5. The higher incidence of leprosy in male population can be attributed to higher rate of exposure and hence increased risk of infection (Table 1). This confirms to previous by Campos ER et al. [1-2].
| Age | Sex | No | Total (N) | Total % |
|---|---|---|---|---|
| 20-30 | M | 1 | 2 | 2.7 |
| F | 1 | |||
| 31-40 | M | 4 | 5 | 6.7 |
| F | 1 | |||
| 41-50 | M | 10 | 14 | 18.7 |
| F | 4 | |||
| 51-60 | M | 10 | 21 | 28 |
| F | 11 | |||
| >61 | M | 28 | 33 | 44 |
| F | 5 | |||
| Total | M | 53 | 75 | |
| F | 22 |
Table 1: Age sex distribution.
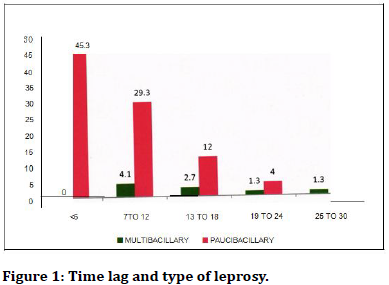
Dividing the patients to multibacillary and paucibacillary groups, maximum incidence was seen in paucibacillary group and the incidence of paucibacillary in the group with time lag of 19 to 24 months is low (4.1%) compared to that of time lag of <6 months (45.2%)(Figure 1).
Figure 1. Time lag and type of leprosy.
Discussion
Summarising the ocular manifestations in the 75 cases of our study group, we found that majority had brow and eyelash madarosis constituting 33%, Lagophthalmos 10.6%, Exposure Keratitis 9.3% and chronic dacroyocystitis 1.3%. Dividing the patients to multibacillary and paucibacillary groups, maximum incidence was seen in paucibacillary group and the incidence of paucibacillary in the group with time lag of 19 to 24 months is low (4.1%) compared to that of time lag of <6 months (45.2%), indicating the effectiveness of early detection and effective control of disease by Multi Drug Regime Therapy [4-10].
The incidence of severe ocular manifestations increases with the duration of the disease, time lag between onset of the disease and treatment. This is also in confirmation with previous reports. With proper medical and surgical management we can conserve sight and restore useful vision to patients previously considered beyond help.
References
- CamposWR, Orefice F. Bilateral Uveitis caused by M. Laprae diagnosed through paracentesis. Ind J Lepr 1998; 70:27-31.
- Campus WR, Monteiro LG. Study of ocular changes in Leprosy patients Ind. J. Lepr 1998; 70:197-202.
- Boratto IM, Orefice F. Dacryocystographic exam does not identify early seventh nerve failure in leprosy patients. Ind J Lepr 1998; 70:287-289.
- Desikan KV. Report of study of eye lesions in 3 autopsy cases of Leprosy. Ind J Lepr 1970; 42:1-4.
- Guimaraes FC. Eyelid changes in long standing leprosy. Oph Plastic Rec Surg 1998; 14:239-243.
- Hieselaar LC, Hogcweg M. Corneal sensitivity in leprosy and controls. BJO 1995; 79:993-995.
- Hogeweg M. Leprosy in the eye Comm Eye Health 1989; 22-30.
- Job CK, Ebenezer GJ. Pathology of eye in leprosy. Ind J Lepr 1998; 70:79-91.
- Job CK, Thompson K. Histopathologcal features of Lepromatous Iridocyclitis Int J Lepr 1998; 66:29-33.
- Karacorlu M. Corneal sensitivity in anterior segment pathology m Ocular leprosy. BJO 1992; 75:117.
Author Info
Department of Anatomy, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: PM Palanimuthukumaran, A Study of Ocular Manifestations in Leprosy, J Res Med Dent Sci, 2021, 9(8): 60-61
Received: 14-Jul-2021 Accepted: 02-Aug-2021