Research - (2021) Volume 9, Issue 4
A Study of Etiological Factors Involved in Acute Pancreatitis in Sree Balaji Medical College and Hospital
Namasivayam T and Baskaran PK*
*Correspondence: Baskaran PK, Department of General Surgery, Sree Balaji Medical College & Hospital, Bharath Institute of Higher Education and Research, India, Email:
Abstract
response to therapy. Nearly 0.0025% world’s population affected by pancreatitis and its prevalence is ever increasing. The present study aimed to evaluate the incidence, causative factors, etiological factors, investigations and complications in patients with Acute pancreatitis admitted in medical and surgical departments of Sree Balaji Medical College, Chromepet, Chennai between October 2013 and October 2015.
Methods: After the ethical permission, fifty patients that were fulfilled the inclusion criteria were enrolled in to the study. Detailed medical history and physical examination was performed and investigated.
Results: Male were severely affected than the females and a direct correlation between the alcoholic (46%) and pancreatitis followed by gallstone (34%). Other factors such as ERCP, Drug induced and trauma also a pivotal role in the disease progression. Of them, 38% of the patients are smokers and 62% are non-smokers. 88% of patients had elevated serum amylase level. Serum alanine transferase was elevated in 11 patients (22%). Hypercalcemia in 4 patients (8%). 56% of patients had no complications. Among the complications sterile necrosis was the commonest (30%)
Interpretation and Conclusion: The study showed that the severity of the disease could be minimized by reducing the alcohol consiumptiom and maintaining the balanced diet.
Keywords
Pancreatitis, Alcohol, Ultrasonography, Serum amylase, Complications, Necrosis, Pseudocyst
Introduction
Throughout the last decades, acute pancreatitis (AP) remains one of the most extensively investigated therapeutic problems with a hardly improvable course. The incidence of the first attack of AP has increased in past decades. In 80% of acute pancreatitis patients, pancreatic injury is mild or moderate and selflimiting, requiring only brief hospitalization to recover without complications. About 25% of the patients is associated with organ failure and local complications [1,2]. The influence of etiological factors on the course and outcomes of AP is not fully understood yet. The dominant (>80%) etiological factors of AP are gallstones and alcohol consumption [1,3] Prevalence of these two main etiologic factors in AP varies considerably among different countries, reflecting differences in culture, tradition and lifestyle [4]. The etiology of pancreatitis should be determined on admission or in the early course of the disease, as this allows the clinician to choose the most appropriate. Management strategies and therapy in acute phase to prevent the recurrence. A detailed personal history (including data such as previous acute pancreatitis or gallstone disease, alcohol abuse, drug intake, metabolic syndromes, trauma or recent invasive procedures, concomitant autoimmune diseases) and family history of pancreatic disorders can provide guidance for a first etiological approach. Physical examination, biochemical tests (liver enzymes, calcium, triglycerides) and the appropriate performance of imaging studies will help to make a differential diagnosis among biliary, alcoholic, and other causes of pancreatitis.
To identify the various etiological factors involved in acute pancreatitis in our hospital. To study the causative factors, clinical presentations, complications, and investigations in patients with acute pancreatitis. To study the age and sex distribution of patients presenting with acute pancreatitis.
Materials and Methods
The study was conducted over a period of two years (October 2013 to October 2015) with fifty patients admitted to medical and surgical departments of Sree Balaji Medical College and Hospital, Chromepet, Chennai.
Inclusion criteria
All patients attending medical and surgical wards of Sree Balaji medical college and hospital who have been diagnosed to have acute pancreatitis for the first time. This study includes all the age groups and both the sex.
Exclusion criteria
All abdominal conditions having similar clinical features other than pancreatitis. Patients who refused to take part in the study.
Patients with carcinoma of pancreas. Patients who were diagnosed to have chronic and acute on chronic pancreatitis. The details of the patients including clinical features, family history of pancreatitis, alcohol intake, dietary habits, stigmata of alcoholic liver diseases were collected. The medical investigations related to blood routine, serum amylase, serum LDH, serum calcium, liver function test and radiological investigations like plain X ray abdomen, abdominal ultrasonography and CT scan were done. the patients were grouped based on their severity of the disease using ultrasonography of abdomen as followed, Acute pancreatitis when the patient had hypoechogenic bulky pancreas. Chronic pancreatitis when they had ductal dilatations and calcifications.
The data were analyzed using a designed proforma and subjected to relevant statistical analysis.
Results
Incidence
Overall, 28,765 cases of abdominal pain were screened for pancreatitis during the study period (two years) in medical and surgical departments, out of which fifty cases have been diagnosed to have acute pancreatitis. Hence the incidence of pancreatitis in this study was found to be 1.73 cases/1000/ year.
Age and sex distribution
Acute pancreatitis is more common in 31–40- year age group in males and 41-50 age group in females (Table 1 and Figure 1). If both sexes were included 29 cases (58%) were between 31-50 years age group (Table 2 and Figure 2). Out of 50 patient’s majority of cases 41/50 (82%) were male patients and 9/50 (18%) are females. The study revealed that the patients felt severe on epigastric region (90%) and radiation of pain was towards the back (66%). Table 3 and Figure 3 had showed site of pain and its distribution. The Etiological factors significantly contributed to the severity of the disease. In the present study, 23 patients (46%) out of 50 patients were alcoholic. In 17 patients (34%) the underlying etiology was found to be Gallstones. Hypertriglyceridemia was seen in 2 patients (4%). Other causes like ERCP, Drug induced, and trauma accounted for 8 patients (16%) (Table 4 and Figure 4).
| Age group | Number of cases | Total | Percentage | |
|---|---|---|---|---|
| Males | Females | |||
| 1-10 | - | - | - | |
| 11-20 | - | 1 | 1 | 2% |
| 21-30 | 7 | 2 | 9 | 18% |
| 31-40 | 15 | 2 | 17 | 34% |
| 41-50 | 9 | 3 | 12 | 24% |
| 51-60 | 7 | 1 | 8 | 16% |
| 61 & above | 3 | - | 3 | 6% |
Table 1: Age distribution and incidence of pancreatitis.
| Gender | Number of cases | Percentage (n=50) |
|---|---|---|
| Male | 41 | 82 |
| Female | 9 | 18 |
| Total | 50 | 100 |
Table 2: Gender Distribution and incidence of pancreatitis.
| Site | Number of cases | Percentage (n=50) |
|---|---|---|
| Epigastrium | 45 | 90 |
| Left | 2 | 4 |
| Right | 3 | 6 |
Table 3: Distribution of site of pain in pancreatitis cases.
| Etiology | No of patients | Percentage |
|---|---|---|
| Alcoholic pancreatitis | 23 | 46% |
| Gall stones | 17 | 34% |
| Dyslipidemia | 2 | 4% |
| Others (ERCP, drug induced & trauma) | 8 | 16% |
Table 4: Distribution of etiology among study subjects.
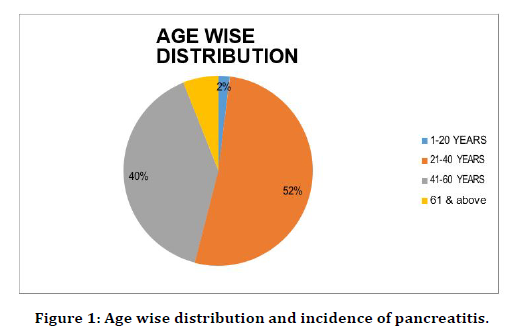
Figure 1. Age wise distribution and incidence of pancreatitis.
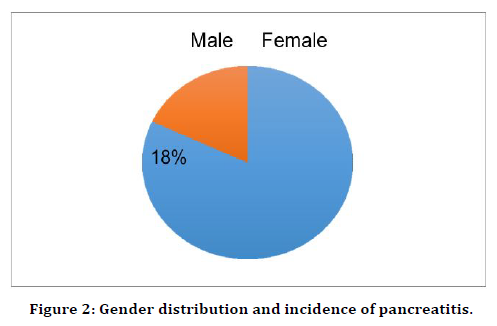
Figure 2. Gender distribution and incidence of pancreatitis.
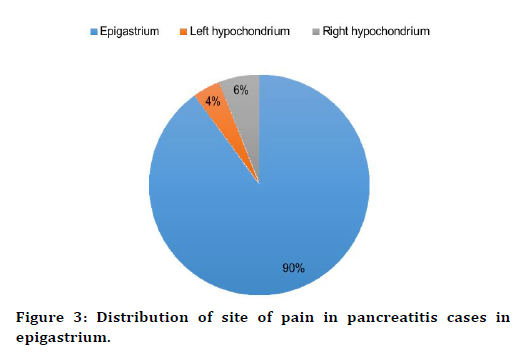
Figure 3. Distribution of site of pain in pancreatitis cases in epigastrium.
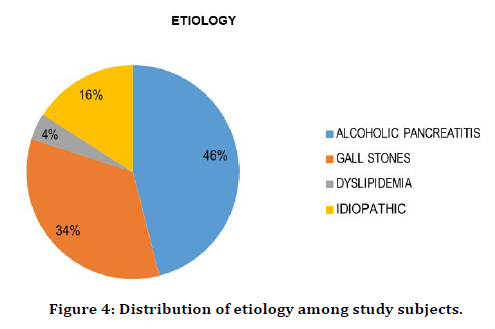
Figure 4. Distribution of etiology among study subjects.
Association between smoking and acute pancreatitis
In the 50 patients with acute pancreatitis, 19 patients (38%) were found to be smokers. Out of which 15 patients (30%) are current smokers and 4 patients (8%) were former smokers. Rest of the 31 patients (62%) are non-smokers (Table 5 and Figure 5).
| Number of patients | Current smokers | Former smokers | Non-Smokers |
|---|---|---|---|
| 50 | 15 | 4 | 31 |
| Percentage (%) | 30% | 8% | 62% |
Table 5: Association between smoking and acute pancreatitis.
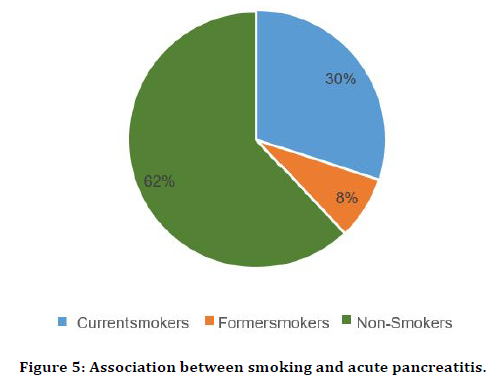
Figure 5. Association between smoking and acute pancreatitis.
Serum amylase was elevated 5 times of the normal level in 44 patients (88%) of acute pancreatitis. The serum alanine transferase was elevated in 11 patients (22%) indicating that they had gallstone diseases. Serum albumin was less than normal in 6 patients (12%), whereas hypercalcemia was found in 4 patients (8%). Diabetes with blood sugars greater than 180mg/ dl was found in 9 patients (18%). And Total WBC count was raised in 9 patients (18%). The medical investigations were summarized in Table 6.
| List of investigations | No of patients | Percentage |
|---|---|---|
| Serum amylase >800U/L | 44 | 88% |
| Serum alanine transferase >90 U/L | 11 | 22% |
| Serum albumin <3.2g/l | 6 | 12% |
| Serum calcium >10mg/dl | 4 | 8% |
| Blood sugar (>180mg/dl) | 9 | 18% |
| Total WBC count >15000 | 9 | 18% |
Table 6: Results of investigations.
Complications
Acute pancreatitis also caused many complications in the studied subjects (Table 7 and Figure 6). 28 patients (56%) had no complications, 15 patients (30%) had sterile necrosis, 3 patients (6%) had infected necrosis and 4 patients (8%) had pseudocyst.
| Complications | Total (%) |
|---|---|
| Sterile necrosis | 15 (30) |
| Infected necrosis | 3 (6) |
| Pseudocyst | 4 (8) |
| Total (%) | 50 (100) |
Table 7: Distribution of complications.
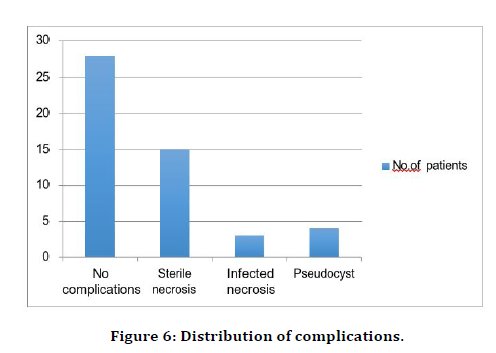
Figure 6. Distribution of complications.
Discussion
Acute pancreatitis is an inflammation of the pancreas and its etiology and pathogenesis have been extensively investigated worldwide. The clinical profile, complications and response to therapy are significantly vary in different parts of the world and warrant for detailed evaluation to reduce its related morbidity and mortality. Although advances in pancreatic function testing and imaging procedures have broadened our knowledge of pancreatitis, the early diagnosis of acute pancreatitis and its complication is still difficult. Therefore, this study was undertaken at Sree Balaji Medical College and Hospital, Chromepet, to study the clinical and etiological profile of acute pancreatitis. Out of 28,765 patients screened for pancreatitis during the study period, only, fifty were diagnosed with acute pancreatitis. Hence the overall incidence of acute pancreatitis was found to be 1.73 cases/ 1000/ year. A study conducted by Spanier et al. [5] in Czech Republic showed an incidence of 7. 9 cases per 100,000 persons. In this study the age of patients ranges from 12 to 70 years and most of the patients were above 30 years of age. The present study has shown that 82 % of the patients were males and only 18% were females. Categorization of patients based on the type of pancreatitis was made based on their ultrasonography. Although pain abdomen was found to be the most common symptom for pancreatitis, and this was correlated with a study conducted by Lee et al. [6] in which 30 (86%) patients out of 35 cases had abdominal pain.
The site of abdominal pain may also vary in patients with acute pancreatitis. In our study 45 (90 %) patients had pain predominantly in the epigastrium, 2 (4%), patients had pain in the left hypochondrium, 3 (6%) in the right hypochondrium. However, this does not correlate with a study conducted by Lankisch et al. [7] where 68% of patients had pain predominantly in the epigastric region, 32 % in the right hypochondrium, and 10 % in the left hypochondrium. Bile duct stones and alcohol abuse together account for about 80% of acute pancreatitis. In most of the countries, alcohol is the major etiologic factor in the development of acute pancreatitis. In the present study alcohol consumption was present in 23 (46 %). This was correlating with the study conducted by Shaheen et al. [8] in 760 patients of acute pancreatitis, the percentage of alcoholics was 53% which shows alcohol was the prime etiological factor.
Alcohol is a well-known precipitant of acute pancreatitis, although the incidence of acute pancreatitis in heavy alcohol consumers is not more than 2% to 3% per year, suggesting that there are as yet undetermined environmental or genetic factors that influence the development of acute pancreatitis in this population. The incidence rate may be similar in heavy drinkers of both sexes. Acute pancreatitis incidence rates peak between ages 35 and 44 years. Furthermore, alcoholic acute pancreatitis has the highest associated risk of overall mortality, with the odds of death increased 90% as compared with biliary pancreatitis, possibly due to poor baseline nutrition [6]. Excessive alcohol use as a cause of pancreatitis is more common among men than women; the association between alcohol consumption and acute pancreatitis is complex but appears to be dose-dependent. In 17 (34%) patients the underlying etiology was found to be Gallstone. The high incidence of common bile duct stones supports the hypothesis that the causative mechanism in gall stone pancreatitis is the passage of a calculus through the common channel formed by pancreatic and common bile ducts, with consequent reflux of bile or duodenal juice into the pancreatic duct [8].
Hypertriglyceridemia was seen in 2 patients (4%). Other causes like ERCP, Drug induced, and trauma accounted for 8 patients (16%). Smoking is a risk factor for AP. In our study out of 50 patiens with AP, 19 patients (38%) were found to be smokers. Out of which 15 patients (30%) are current smokers and 4 patients (8%) are former smokers. 31 patients (62%) are non-smokers. In a study conducted by Tolstrup et al. [9] it is reported that smoking increases by approximately two-fold the risk of AP. The exact pathogenesis is unknown, but nicotine has been shown to modulate the oxidative stress and lipid peroxidation and these processes might be involved in the pathophysiology of acute and chronic pancreatitis. Interestingly in our study, there were no patients with family history of pancreatitis. Serum amylase and lipase activities are elevated only during acute attacks of pancreatitis and not during asymptomatic intervals. In this study, 44 (88%) patients had elevated serum amylase 5 times of the normal level. The single best laboratory predictor of biliary pancreatitis; a level of alanine aminotransferase more than three times the upper limit of normal (10-40 IU/L) has a positive predictive value of 95 percent for gallstone pancreatitis. However, the presence of normal alanine aminotransferase levels does not reliably rule out the diagnosis. In our study, the serum alanine transferase was elevated in 11 patients (22%) indicating gallstone diseases. Serum albumin was less than normal in 6 patients (12%), whereas hypercalcemia was found in 4 patients (8%). Diabetes with blood sugars greater than 180mg/dl was found in 9 patients (18%). And Total WBC count was raised in 9 patients (18%). In this study 28 (56%) patients had no complications, 15 (30%) patients had sterile necrosis and 3 (6%) patients had infected necrosis. 4 (8%) patients developed patients developed pseudocyst [10].
Limitations of the Study
One of the limitations of our study was the small sample size, because of which the results of the study may not be applicable to the community. Incidence in this study may show subtle variation as the conduct of the study was restricted to only Medicine and Surgery departments. The number of cases screened and the total number of patients attending the outpatient department may vary due to constrain of single investigator and lack of computerized data storage.
Conclusion
In this study we concluded that most of the clinical observations was in accordance with other studies conducted earlier. A total of 50 patients with acute pancreatitis were studied and males were more prone to the disease. Among the study group, all the patients presented with abdominal pain and most of them had it in the epigastric region. Alcohol and gallstones were the main factors associated with pancreatitis followed by Hypertriglyceridemia. As the medical investigations were significantly varied with the severity of the disease the present study implied the need of holistic approach for providing the best treatment regime.
Funding
No funding sources.
Ethical Approval
The study was approved by the institutional ethics committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgments
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Frossard JL, Steer ML, Pastor CM. Acute pancreatitis. Lancet 2008; 371:143–152.
- Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology 2013; 144:1252–1261.
- Lowenfels AB, Maisonneuve P, Sullivan T. The changing character of acute pancreatitis: Epidemiology, etiology, and prognosis. Curr Gastroenterol Rep 2009; 11:97–103.
- Whitcomb DC. Clinical practice. Acute pancreatitis. N Engl J Med 2006; 354:2142–2150.
- Spanier BW, Dijkgraaf MG, Bruno MJ. Epidemiology, aetiology and outcome of acute and chronic pancreatitis: an update. Best Pract Res Clin Gastroenterol 2008; 22:45-63.
- Lee MG, Chun A, Miles A, et al. Chronic pancreatitis in Jamaica. West Indian Med J 1992; 4:61-63.
- Lankisch PG, Schirren CA, Kunze E. Undetected fatal acute pancreatitis. why is the disease so frequently overlooked? Am J Gastroenterol 1991; 86:322 -326.
- Shaheen MA, Akhtar JA. Organ failure associated with acute pancreatitis in African-American and Hispanic patients. J National Med Assoc 2007; 99:1403.
- Tolstrup JS, Kristiansen L, Becker U, et al. Smoking and risk of acute and chronic pancreatitis among women and men: A population-based cohort study. Archives Internal Med 2009; 169:603-609.
- Acosta JM, Pellegrini CA, Skinner DB. Etiology and pathogenesis of acute biliary pancreatitis. Surgery 1980; 88:118-125.
Author Info
Namasivayam T and Baskaran PK*
Department of General Surgery, Sree Balaji Medical College & Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: T Namasivayam, PK Baskaran, A Study of Etiological Factors Involved in Acute Pancreatitis in Sree Balaji Medical College and Hospital, J Res Med Dent Sci, 2021, 9 (4): 381-386.
Received: 20-Mar-2021 Accepted: 21-Apr-2021
