Review - (2022) Volume 10, Issue 8
A Review Article: CRP as a Prognosis Factor from Day 1 to Day 6 in COVID-19 Patient
Shivangee* and Sonali Choudhary
*Correspondence: Shivangee, Department of Community Medicine, Jawaharlal Nehru Medical College, Datta Megohm Institute of Medical Science (Deemed to be University), India, Email:
Abstract
Introduction: Coronavirus SARS COV-2 has emerged as a global health issue with high fatality rates. Since there is no particular identifiable cure to this yet, precaution prevention and analyzing risk factors could only help to determine the mortality risk in individuals and curtail the effect of disease. How to reduce the spread and control disease mortality is major concern. One of the reliable biomarker till date is C reactive protein C reactive protein is an inflammatory marker formed by liver during any inflammation due to bacteria, virus, and fungus. Usually the levels in normal body are low around. Background: This process of inflammation is succeeded by process of healing which as a response produces acute phase reactant “one of which is CRP. It is easily available, inexpensive, easy to obtain marker for study. It can be classified based on their concentration in serum as - positive or negative. This suggest that during inflammatory process positive APR up regulates while negative APR down regulates Summary: The value increased on day1 in moderate severe cases but declined after day6 in survivors of covid-19 patients as per data released by different journals. The test is recommended in patients of covid-19 infection who has moderate to severe symptoms not relieved after 5 day. It helps in early detection of cytokine storm which is said to occur in second week of illness tracking the rate of change of the marker from Day 1 to Day 3 to Day 6 is very powerful and very clinically predictive test. The values were considerably increased in severe to morbid patients (200mg/l) compared to mild patients (20mg/l) with a sensitivity of 67%. So to combat these complication researchers came together to a conclusion that Statistical significance in CRP median exists between different subgroups clinical types and ages. In this article we aim at predicting the severity and outcome of patients infected by coronavirus by prognostic marker CRP
Keywords
Covid-19, Creative protein, Biomarker, Prognosis, Article
Introduction
Since December 2019, a new virus called SARS-COV-2 originated from Wuhan, china and quickly got spread in various continents across the globe and classified as PANDEMIC by WHO . SARS-C0V-2 is one of the seven types of coronavirus which may lead to mild to sudden acute respiratory syndrome. It has two strains : L and S . S is the older variant while L is common in outbreak. It is said to affect lungs, throat, sinuses , nose. The infection is spread through contact, droplets, and aerosols [1]. It has also been detected in non-respiratory specimen like blood, stool but are not very significant source of infection. It has been seen that the major cause of spreading of pandemic is its long distance transmission of virus. These are group of RNA virus mainly infecting mammals and birds, birds, ranging from mild illness like common cold to hepatitis, diarrhoea, and encephalomyelitis. Belonging to subfamily Orthocoronavirinae, family Coronaviridae, order Nidovirales, morphologically they are large spherical particles with unique projections coronavirus virion consists of structural proteins, namely spike , envelope , membrane , nucleocapsid and, for some beta coronaviruses, haemagglutinin-esterase. These are similar to those seen in other influenza viruses.
Its variant like alpha and delta are spreading faster and delta virus is said to be more potent and hazardous. Currently the mutated virus has taken countries like India, Brazil down on their knees which has known to cause severe lung pneumonia, embolic episodes and hypercoagulability. Normal to low white cell counts and increased interleukin-6 (IL-6) levels are consistent blood indicators in afflict-ed people. the fact that it is mostly a respiratory sickness, new evidence reveals that multi-organ harm is widespread, especially in moderate to severe infections.
Owing to rapid hike in COVID-19 infections, hospitals all over the world are facing challenges to emit huge incoming of patients, to combat this only severely ill patients were admitted in Intensive units while the rest were managed at home or isolation centre. Therefore the problem lies in early diagnosis and identifying these patients so actively monitoring is possible.
Since the cure is still not found, predicting the disease severity and to generate favorable outcome different lab investigation are been done like D DIMER, IL6, CRP.
Bacterial products are sensed by macrophages through TLR receptors, downstream signaling leads to activation of nuclear, transcriptional products which in turn activates liver to produce acute phase reactant. This process of inflammation is succeeded by process of healing which as a response produces acute phase reactant "one of which is CRP. It is easily available, inexpensive, easy to obtain marker for study. It can be classified based on their concentration in serum as - positive or negative. This suggests that during inflammatory process positive APR up regulates while negative APR down regulates. Talking about CRP it is not disease specific marker, it can be seen elevated in cancers, coronary artery disease, high cholesterol, infections, allergies, crohns disease so on and so forth. It is synthesized in hepatocytes (liver) and released in the blood streams from where the test sample is collected by venous puncture. The levels of CRP is regulated by other cytokines like IL-1 $ IL-6. The have increase affinity for bacteria as compared to other pathogens. The cytokine complication cascade include interleukin (IL) 6, IL-1β, and CC chemokine ligand 3 (CCL3), released by airway macrophages which are maladaptive form of immune responses. There is also synthesis occurring outside the liver called s extra hepatic synthesis like in atherosclerotic plaques, lymphocytes , monocytes. On the other hand it is seen that viral infection without bacterial involvement is very less likely if CRP is > 40 mg/l. CRP levels also depends on genetic constitution of an individual, studies were performed using gene and protein analysis. haplotype 4 is associated with increased risk of higher values of CRP. Variations were also seen with time of the day, according to a study it was found that highest mean concentration was found in morning time and lowest concentration in the noon. Other things which affects CRP level includes sedentary lifestyle, smoking, obesity, diabetes. While it has been seen that nitric oxide can decrease CRP production. CRP's primary function is to eliminate dying cells. Water plugs the alveoli during the sickness, leaving the lung cells without enough oxygen to repair. CRP destroys cells that are actually healthy, resulting in a hazardous overreaction. In other words, it is the inflammation, not the corona virus that causes lung damage.
Due to an excessive immune response to the virus the body triggers inflammatory cell infiltration in the lungs, activation of T-helper 1 reactions, and abundant release of proinflammatory cytokines into the blood circulation, known as the cytokine storm syndrome is the most feared and serious complication of COVID-19 patients.
According to Receiver operating characteristic curve (ROC) it can be used as an independent factor [2]. The area under the curve for CRP is used to describe severity of COVID-19 was predicted to be around 0.844 (95 percent CI, 0.761–0.926; P.001).
There are no particular signs and symptoms due to increase CRP, if any present it is due to under-lying inflammation. It is a type of latex agglutination test in which patient’s serum is mixed with human anti-cop and after 2 minutes agglutination is observed and result is quantified using photo-metric measurement [3].
Inclusion criteria
The subject for the studies was patients tested positive on RT-PCR. There are some studies that have recently reported that C-reactive protein (CRP) levels can be used in the detection of early diagnosis of pneumonia and to interpret the severity of the disease by checking upon increased values of CRP.
CT SCAN lung showed typical ground glass appearances, lung exudates, crazy pavement appearances and result was given through a CT score ranging from 0-25 (mild –severe).
Several retrograde studies are done to detect CRP value in severe and non- severe patient for comparison of prognosis of the disease. Patient’s medical record is viewed by clinicians. Data collection of symptoms, demographic detail, sex, past medical history and lengths of hospital stay was also done. Variables were expressed as counts with proportions and those which were significantly associated (P < .05) with disease progression were included in the analysis. The patient was classified into mild moderate and severe groups. The data within the course of 30 days were analysed while, maximum CRP during 7 days were noted. According to published studies the CRP at admission, maximum CRP, mean CRP values in various stages were collected to show a relationship between lesion, CRP, clinical types, outcome.
Exclusion criteria
Patients with onset of symptoms more than6 days, patients with bacterial infection, negative RT-PCR patients, patients with incomplete data.
The data collected are expressed as mean ± standard deviation. Numeric data was analysed using chi-square test.
Results
Positive correlation is defined as when two variables moves in same direction like if one decreases then other variable also decreases and if one increases the other dependent variable also increases.
The difference was statistically significant. CRP levels were positively correlated (positive correlation) with the diameter of lung lesion and severe presentation of the disease (correlation coefficient=0.873, 0.734, P˂0.001) [2]. The normal values of CRP is in the range of 0.3-1 mg/ dl while that noted in mild patients is 10-20 mg/dl and above 35mg/dl in severely ill patients which in hand I a depiction of increased circulating cytokines level in body [4]. The median value is ICU admitted patients were around 111mg/l while those in succumbed patients were 230mg/l. The rate of change in value due course of hospital stay is more useful than a highest value during any single day. Highest peak is observed after 48 hours disease onset.
Thus it can be said that for increase in 1unit of CRP risk of having serious effects increases by 5% [5]. A maximum CRP during the first 7 days of illness more than 250 mg/L provided 67% sensitivity, 57% specificity, 34% PPV, and 84% NPV for mortality prediction. It was noted that there is increased risk in males compared to female though there was insignificant difference with p=0.122 [6]. P value signifies the difference between severe and non- severe patients, <0.5% indicates significant statistics [2]. The connection of plasma CRP levels and the severity of COVID-19 pneumonia on chest CT performance was also investigate and analysed .The diameter was taken of the largest lung lesion were higher in the moderate group than in the mild group (Mann-Whitney test=2.647, 2.171, P 0.05), and CRP levels and the diameter of the largest lung lesion were higher in the severe group than in the moderate group (Mann-Whitney test=0.693, P=0.01) (Figures 1 and 2).
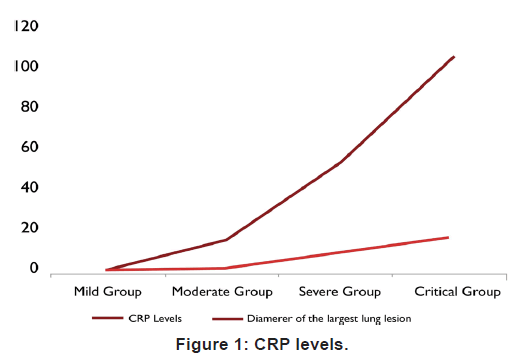
Figure 1. CRP levels.
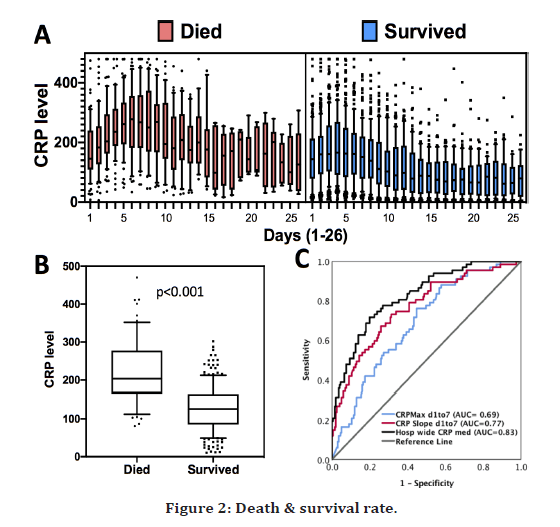
Figure 2. Death & survival rate.
Discussion
The number of cases is increasing exponentially so is the asymptomatic cases, though the survival is better but these asymptomatic cases tend to spread the disease more. Early monitoring of key markers is thus the basis of treatment strategies to reduce fatality rate. The main pathological damage is caused to immune system and lungs, lowered immunity welcomes other infections like bacterial pneumonia, black fungus, and white fungus commonly encountered these days. Physical distancing, use of mask, hygiene are said to prevent disease. Vaccine has shown to be efficient in reducing disease severity. Home isolation is advised in mild cases with proper monitoring. We enrolled hospitalized patient mostly of age group >30 years by cohort study, Sahu et al. examined the CRP levels of 849 died and 1896 recovered COVID-19 patients in a meta-analysis. They discovered significant levels of CRP in the bodies of deceased patients, suggesting that CRP might accurately predict COVID-19 illness prognosis.
Thus CRP lowering agents may be useful to control disease progression like statin, aspirin, vitamin c in covid infected patients. Diet low in cholesterol and rich in fruits and vegetables would be helpful. Continuous monitoring of CRP is helpful both In home isolation and ICU patients to reduce chest complications. Add on laboratory investigations like D-dimer, IL-6 are also done in ICU patients or patients with comorbid conditions to reduce risk of thromboembolism. 50% Reduction in CRP was also noted on administration of corticosteroid though steroids have their own disadvantages. CRP levels in patient with underlying cardiovascular disease and infected with covid infections has also elevated troponin I compared to other patients [7,8].
Also in patients with type 2 diabetes mellitus and infected with covid infection has higher CRP value and neutrophil counts in sepsis associated with covid infection inflammatory mediators are most important pro inflammatory markers, CRP has ability. The test is also recommended in patients with fluctuating levels of oxygen saturation and under home isolation to know the extent of inflammation ongoing in body. It is also in recommended in patients under home isolation with no improvements to treatment. Though CRP levels are not very much linked with viral infections but it has been seen that adaptive immunity clears the disease process by macrophage activation syndrome which may indirectly in-crease CRP levels.
Conclusion
Several other research linking CRP levels to disease severity backed up our findings. CRP has been proposed as a predictive marker in dengue infection, with greater levels of CRP suggesting a greater risk of illness development. Dengue virus and SARS-CoV-2 are both RNA viruses, and their infection processes are quite similar.
Our study showed that there exists a positive correlation between crp value and disease outcome in covid patients and provided early threshold during hospitalization and higher treatment modalities. Sex of the patients mattered insignificantly. Rate of change of crp from Day1 to Day6 is much more useful than one time value. We looked at the CRP levels over time for the full sample and found that they rose in a linear and uniform pattern throughout the initial first week of hospitalization, peaked on day5, and then gradually dropped. Levels increased with increase in lung lesions in pneumonia. Different from th survivors with changes gradually decreased to a normal level, CRP rapidly elevated within 10 days and increased persistently but slowly decreased. Clinical characteristic of severe patients include hypertension, diabetes, cerebrovascular disease, cardiovascular disease as co-morbidities. As a quick and simple technique of screening for lung infection, CT scan examination may not only establish the existence of lung infection, but it can also serve as a reference for establishing the kind of pathogen, providing unique diagnostic benefits. The sensitivity of COVID-19 diagnosis using CT scan alone was 76.4 percent, according to latest research of Zhong Nanshan’s, and the application of CT scan in COVID-19 diagnostic was 76.4 percent.
During the study of case, a small proportion of non- severe patients developed into severe cases in the first 2 weeks after onset of symptoms. Therefore, health care institutions should pay close attention to the mild patient as well.
It is a highly sensitive marker for tissue damage, infections occurring anywhere in body or any ongoing inflammatory process; it helps in removing source of infection by activating process of phagocytosis and complement activation. This result indicated that CRP levels were highly raised in severe patients, in expired patients, patients in ventilator than compared to non-severe patients. Complications during disease progression were also associated with increased levels.
From day 1 to day 3 levels started increasing while it peaked on day for which correspond to specificity of pneumonia , whereas ESR levels peaked after day 5. So it is used in some countries in Nordic to differentiate pneumonia from other respiratory tract infections. Continuous Decline in levels started at day 10. A hypersensitive test of CRP can detect minor elevations and give a uniform pattern. The goals of lowering CRP is to reduce risk of CVD, so exercise, good diet, cessation of smoking, statins are used in therapy. Since medical facility especially in Asian countries is not upto mark and doctor to patient ratio, bed to patient ratio is less, theses early markers will help to decrease severity and mortality of disease. The case study and reports were made in retrospective study in admitted, hospitalized patients using medical record, test reports, data analysis.
References
- Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J Med Virol 2020; 92:401.
- Wang G, Wu C, Zhang Q, et al. C-reactive protein level may predict the risk of COVID-19 aggravation. In Open forum infectious diseases US: Oxford University Press 2020; 7.
- Ali N. Elevated level of C‐reactive protein may be an early marker to predict risk for severity of COVID‐19. J Med Virol 2020.
- https://www.news-medical.net/news/20201106/Rapid-rise-in-CRP-levels-predicts-COVID-19-outcomes.aspx
- Qu G, Huang G, Zhang M, et al. Features of C-reactive protein in COVID-19 patients with different ages, clinical types and outcomes: A cohort study. Med Rxiv 2020.
- Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 1999; 340:448-454.
- Chen W, Zheng KI, Liu S, et al. Plasma CRP level is positively associated with the severity of COVID-19. Ann Clin Microbiol Antimicrob 2020; 19:1-7.
- Yacoub S, Wills B. Predicting outcome from dengue. BMC Med 2014; 12:147.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Shivangee* and Sonali Choudhary
Department of Community Medicine, Jawaharlal Nehru Medical College, Datta Megohm Institute of Medical Science (Deemed to be University), Sawangi (Meghe), IndiaReceived: 18-Jul-2022, Manuscript No. jrmds-22-69422; , Pre QC No. jrmds-22-69422(PQ); Editor assigned: 20-Jul-2022, Pre QC No. jrmds-22-69422(PQ); Reviewed: 04-Aug-2022, QC No. jrmds-22-69422(Q); Revised: 09-Aug-2022, Manuscript No. jrmds-22-69422(R); Published: 16-Aug-2022
