Research - (2021) Volume 9, Issue 1
A Retrospective Analysis on Interdental Bone Changes After Orthodontic Treatment
Nor Syakirah binti Shahroom and Ravindra Kumar Jain*
*Correspondence: Ravindra Kumar Jain, Department of Orthodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, India, Email:
Abstract
Orthodontic treatment is known for its benefits of making teeth align properly along with improving occlusion and jaw relation. However, some risks and complications may be encountered by the patient including discoloration, decalcification, root resorption, periodontal complications, and allergies. A retrospective study was conducted in a private dental hospital to assess the changes in the interdental bone of the patients who underwent orthodontic fixed appliance treatment. A total number of 30 subjects who had undergone fixed appliance orthodontic treatment were divided into two groups in which 14 subjects were in Group A - non extraction group and 16 subjects were in Group B-extraction group. The interdental bone heights were measured from distal of lower canine to mesial of the second molar in the third and fourth quadrant and the mental foramen was selected as the reference point. Measurements were done on both pre-operative and post-operative panoramic radiographs for both groups and subjected to statistical analysis. A paired T test was done to find the significance of difference in the two groups. The results of the study showed that there was no significant decrease in interdental bone height in the group A (p>0.05). However, there was a significant decrease in interdental bone height in group B (p<0.05). On comparing the interdental bone height changes between the two groups, only the interdental area between 34-35 in group A and 33-35 in group B showed statistically significant differences (p<0.05), similarly in quadrant 4. In conclusion, vertical bone loss in the interproximal area after orthodontic treatment was more significant in the patients undergoing extractions for orthodontic treatment.
Keywords
Alveolar defect, Fixed appliance, Panoramic radiograph, Periodontal bone, Root resorption
Introduction
Over the past few decades, fixed appliances have become a choice of treatment for malocclusions. The appliances are fixed and fitted on the teeth by the dentist and cannot be removed by the patient [1]. The main advantage of fixed appliance is that it allows various tooth movements which are incredibly detailed and precise such as tipping, torquing, bodily movement, intrusion, extrusion and rotating [1,2].
Patients using fixed appliances face difficulties in maintaining proper oral hygiene due to brackets and archwire which leads to the accumulation of food debris and plaque [3,4]. They may develop problems like gingivitis, gingival recession, gingival bleeding, and increased pocket depth [5-8]. Therefore, it is important to practice proper brushing technique and the use of interdental brushes and flossing [9]. Besides, a fixed appliance may also cause root resorption and alveolar defects due to improper treatment procedures [2]. It has also been reported that the extraction site has a high tendency for inter bone loss [10]. Orthodontic bands placed subgingivally may lead to greater bone loss [11]. Assessment of inter bone loss in a patient before proceeding with orthodontic treatment is important. With the help of biomarkers which can be detected in the gingival crevicular fluid, it could help to assist in screening patients at risk of bone loss [12]. The biomarkers are inflammatory cytokines such as interleukin 1β (IL-1β), interleukin 6 (IL -6) and interleukin 8, (IL-8) and growth factors such as tumor growth factor (TGF) [13].
Interdental bone loss following orthodontic treatment is well documented in the literature and there are many factors which can lead to interdental bone loss. The most common reasons include the mechanics used, duration of the treatment, host factors, magnitude of force applied, oral hygiene of the patient. Orthodontic treatment involving extractions of premolars is implicated for interdental bone loss by some authors [10], hence this study was planned to analyze the amount of interdental bone loss in patients undergoing orthodontic treatment with extraction of teeth and to compare the same with patients undergoing non -extraction orthodontic treatment. There are very few studies that have reported about the above findings but there are no studies done in the south Indian population and hence this study was sought. Various imaging techniques can be used to assess the interdental bone change such as intraoral radiographic including periapical and bitewing [2]. Several studies used this technique to measure the interdental alveolar bone height in the orthodontic treated patient. Besides, panoramic radiograph and conebeam computed tomography (CBCT) which provide two dimensional and three-dimensional visualization of the image respectively can also be used to assess the interdental alveolar bone height [2,14]. Our extensive research expertise ranged from epidemiological studies to randomized clinical trials that have been published in reputed journals [15-24]. This knowledge was instrumental for us to study the alveolar bone changes in fixed appliance treated patients using a panoramic radiograph.
The aim of this study was to analyze the interdental bone loss following orthodontic treatment and compare it between orthodontic treatment done without extraction and with extraction of teeth.
Materials and Methods
Study settings and designs
A retrospective study was conducted involving patients who reported for orthodontic treatment in a private dental hospital. Ethical approval was granted by the Institutional Ethics Committee of Saveetha Dental College and Hospitals.
Selection criteria
The 30 case records of subjects were divided into two groups - group A (non-extraction) and group B (extraction). The subjects were chosen based on the inclusion criteria. The inclusion criteria were patients in the age group 18-25 years undergoing fixed appliance therapy with 022 MBT appliance. Meanwhile, patients with existing periodontal ligament disease, missing teeth, congenital deformities, and systemic diseases were excluded. For the group A, 14 subjects that do not require extraction for fixed appliances were selected. Meanwhile for group B, 16 subjects who had undergone extraction of the premolars were selected. Both pre-operative and post-operative panoramic radiographs were assessed for each subject’s record.
Methodology
This study was done by measuring the interdental bone height from the alveolar crest to a point on the reference line drawn tangent to the upper border of the two mental foramina as shown in Figure 1. Measurements were made from the distal of lower canine to the mesial of second molar on both the sides. A vertical line was drawn from the alveolar crest to the reference line [2]. A total of eight measurements were acquired for group A and six for group B. The treatment group had undergone extraction of the first premolar in the third and fourth quadrant. Therefore, the measurement for pre-operative would be the interdental bone between the first molar and second premolar and for post-operative would be between second premolar and canine.
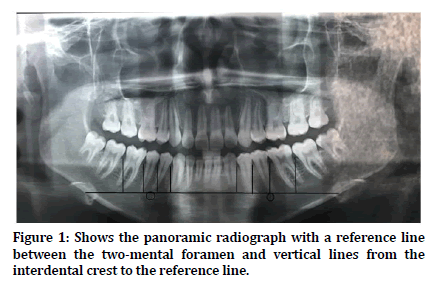
Figure 1. Shows the panoramic radiograph with a reference line between the two-mental foramen and vertical lines from the interdental crest to the reference line.
Statistical analysis
Data were entered in Excel and analyzed using the Statistical Package for Social Sciences SPSS Version 20. The descriptive analysis was computed including mean and standard deviation of each group. The comparison of the data and distribution was checked at 0.05 level of significance using a paired T test. The statistical effect of significance was determined. Independent T test was done to find the significant difference in between the two groups.
Results and Discussion
A total of 30 participants were included out of which 14 subjects were in group A and 16 subjects were in group B. The descriptive statistics for each group are shown in Table 1.
| Interdental bone height between teeth | Group A- Non extraction | Interdental bone height between teeth | Group B - extraction | Independent T test p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| T0 (mm) | T1 (mm) | T0-T1 (mm) | Paired T test p-value | T0 (mm) | T1 (mm) | T0-T1 (mm) | Paired T test p-value | |||
| 36-37 | 23.71 | 22.61 | 1.1 | 0.22 (p>0.05) | 36-37 | 26.97 | 24.81 | 2.2 | 0.003 (p<0.05) | 0.114 (p>0.05) |
| 35-36 | 21.29 | 19.79 | 1.5 | 0.085 (p>0.05) | 35-36 | 22.59 | 20.34 | 2.3 | 0.017 (p>0.05) | 0.649 (p>0.05) |
| 34-35 | 20.14 | 19.5 | 0.6 | 0.475 (p>0.05) | 33-35 | 20.56 | 19.38 | 1.2 | 0.294 (p>0.05) | 0.000 (p<0.05) |
| 33-34 | 18.64 | 17.5 | 1.1 | 0.154 (p>0.05) | - | - | - | - | - | - |
| 43-44 | 18.36 | 17.79 | 0.6 | 0.482 (p>0.05) | - | - | - | - | - | - |
| 44-45 | 20 | 19.43 | 0.6 | 0.414 (p>0.05) | 43-45 | 20.44 | 18.75 | 1.7 | 0.040 (p<0.05) | 0.000 (p<0.05) |
| 45-46 | 21.79 | 21.5 | 0.3 | 0.486 (p>0.05) | 45-46 | 23.84 | 21.41 | 2.4 | 0 (p<0.05) | 0.938 (p>0.05) |
| 46-47 | 24.86 | 24.57 | -0.3 | 0.575 (p>0.05) | 46-47 | 26.94 | 25.31 | -1.6 | 0.002 (p<0.05) | 0.572 (p>0.05) |
Table 1: Shows the comparison of interdental bone height between non extraction group and extraction group.
In group A, there was a slight decrease in the interdental bone height in all teeth after the fixed appliance treatment as shown in Figure 2. However, there was no statistically significant difference between pre-operative and postoperative changes in the interdental bone height (p>0.05) in any of the interdental regions checked.
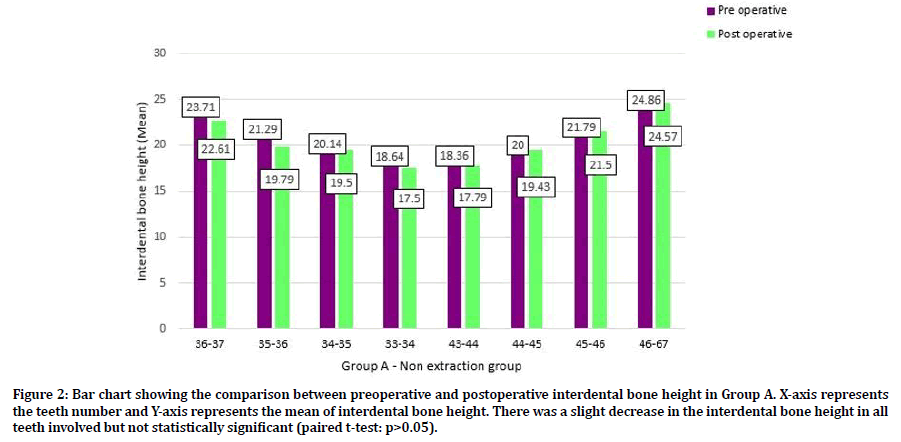
Figure 2. Bar chart showing the comparison between preoperative and postoperative interdental bone height in Group A. X-axis represents the teeth number and Y-axis represents the mean of interdental bone height. There was a slight decrease in the interdental bone height in all teeth involved but not statistically significant (paired t-test: p>0.05).
Meanwhile, in group B there was a decrease in the interdental bone height in all teeth after fixed appliance treatment as shown in Figure 3. There was a statistically significant difference between pre-operative and post-operative changes in the interdental bone height between 36-37, 35-36, 43-45, 45-46 and 46-47 (p<0.05). However, no statistically significant difference was seen in the 33-35 region (p>0.05).
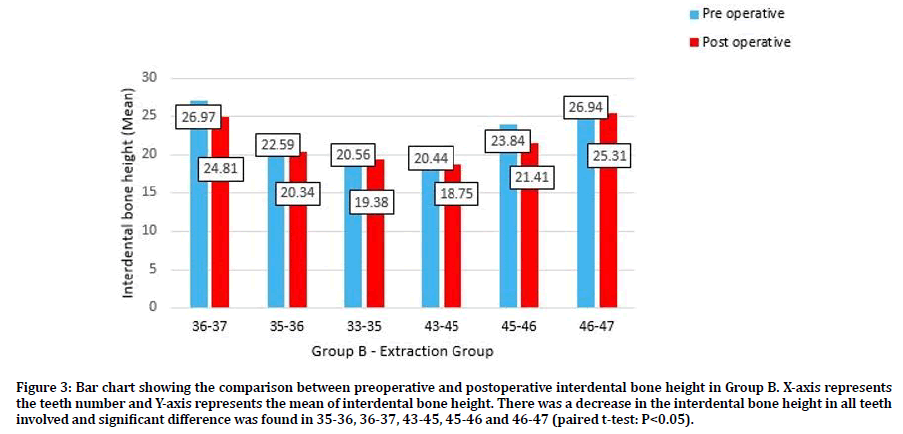
Figure 3. Bar chart showing the comparison between preoperative and postoperative interdental bone height in Group B. X-axis represents the teeth number and Y-axis represents the mean of interdental bone height. There was a decrease in the interdental bone height in all teeth involved and significant difference was found in 35-36, 36-37, 43-45, 45-46 and 46-47 (paired t-test: P<0.05).
On comparing the interdental bone height changes between the two groups, only the interdental area between 34-35 in group A and 33-35 in group B showed statistically significant differences (p<0.05) as shown in Figure 4. Also, the same was noted in the 4th quadrant. In this study, a panoramic radiograph was selected as the method to determine the presence of any changes in the height of bone in the posterior mandibular region. In other reported studies, periapical and bitewing radiographs were used to measure the height from the cementoenamel junction to the alveolar crest ridge which may lead to several false results [25]. This is because, in a post-orthodontic treatment, there are potential changes in the axial slope of teeth [2]. Meanwhile, in the present study, anatomical landmarks such as mental foramen in right and the left side were used as the reference point to construct a reference line. Mental foramen can be easily identified in a radiograph as a round translucency between two premolars which does not change its location depending on age and gender [2].
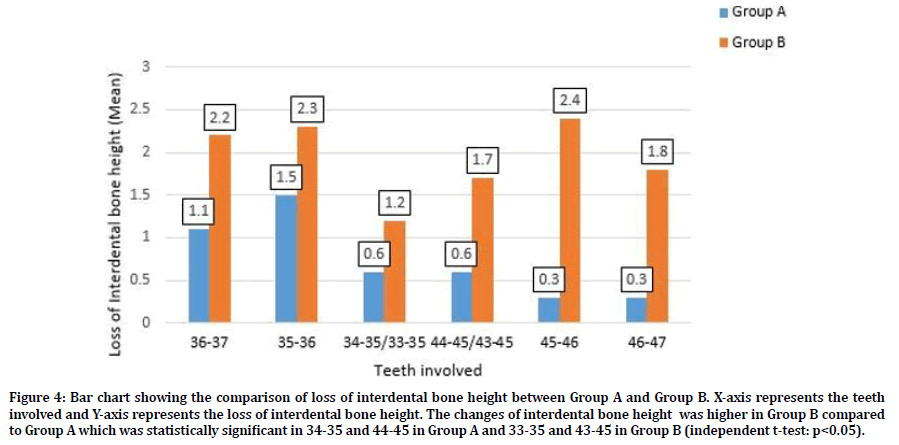
Figure 4. Bar chart showing the comparison of loss of interdental bone height between Group A and Group B. X-axis represents the teeth involved and Y-axis represents the loss of interdental bone height. The changes of interdental bone height was higher in Group B compared to Group A which was statistically significant in 34-35 and 44-45 in Group A and 33-35 and 43-45 in Group B (independent t-test: p<0.05).
According to the present study, there was a change in the height of the interdental bone in both extraction and non-extraction methods of fixed orthodontic treatment. However, in the cases of fixed orthodontic treatment with extraction of teeth, the loss of interdental bone is slightly higher than in non-extraction cases and this is mainly in the extraction site. Several studies suggest that the probability of alveolar bone loss after extraction is high in which the bone resorption activity is quite high after extraction [26]. Besides, it was also reported that the alveolar bone loss and gingival recession among fixed appliance patients may be due to the presence of inflammation during the tooth movement [27]. In a study done by Zacharisson et al. it was reported that the height of alveolar bone decreased with orthodontic treatment [10]. Besides, a study done by Bondemark et al. Ogaard et al. and Janson et al. reported that alveolar bone loss can be seen in orthodontically treated patients when compared with controls in which the mean alveolar bone loss is greater in comparison with the untreated orthodontic patient [28-30].
In a study done by Ahuja et al. the authors reported about the interproximal bone height after orthodontic treatment using Begg Appliance and Preadjusted Edgewise Appliance [31]. It was reported that there was a significant decrease in interproximal alveolar bone regardless of the technique. However, the mean bone loss in Begg Appliance is greater compared to Preadjusted Edgewise Appliance with the maximum value in Begg Appliance was 0.347mm and 0.291mm in Preadjusted Edgewise Appliance. Based on the result, this study suggested that Preadjusted Edgewise Appliance leads to more physiological tooth movement compared to Begg Appliance.
However, in a study done by Celebi et al. it was observed that there was an increase in bone height in patients treated with non-extraction fixed orthodontic treatment [2]. The group revealed a statistically significant increase in three interdental alveolar spaces. According to several studies, the reason for the increase in bone height was due to the extrusive forces that were exerted by fixed orthodontic mechanics [32].
Due to the limitation in radiographic technique, several studies had used cone-beam computed tomography (CBCT) to assess the bone changes in the oral cavity. This method is better in terms of accuracy and precision as it can be evaluated in multiplanar view and the data available with a voxel size below 0.25mm in comparison to other radiographic methods [14]. However, there were some limitations to be considered in CBCT while evaluating the height of the bone such as superimposition and bias in the results [14,33]. In a study done by Kalbassi et al. it was found that CBCT is able to represent the alveolus clearly and also detecting the three-dimensional volume of intrabony defects [34]. Meanwhile, by using a traditional radiograph, it is impossible to assess the dehiscence and fenestration of the alveolar bone due to superimposition. However, it was concluded in a study that the traditional radiography images would provide more bone details, but more pronounced morphologic structure of alveolus and periodontal defects can be seen in CBCT [35]. Thus, each radiographic technique would have different advantages and indications. By identifying all the characteristics of bone such as bone volume, bone thickness, dehiscence, fenestrations and other intrabony defects, it will help in orthodontic diagnosis and well-described treatment plans [34,36].
The limitations in this study include a small sample size, retrospective design. Further studies can be done with a bigger sample to determine whether extraction of teeth for orthodontic treatment is associated with more alveolar bone loss and also other side effects like root resorption, dehiscence and fenestrations can be studied.
Conclusion
In conclusion, this study revealed that there was vertical bone loss in the interproximal area after orthodontic treatment done both with and without extraction of the teeth. Patients treated with extraction mechanotherapy had more vertical bone loss which was statistically significant. This can be attributed mainly to oral hygiene maintenance, the mechanics used and the duration of treatment. Minimizing the incidence of vertical bone loss is important as further progression of bone loss may lead to periodontitis.
Acknowledgment
We thank Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University for granting the research proposal and research support.
Conflict of Interest
No conflict of interest declared by the authors.
References
- Alam MK. A to Z Orthodontics. Malaysia: PPSP Publication 2012.
- Celebi F, Arici N, Canli E. The effects of non-extraction fixed orthodontic treatment on the vertical mandibular bone level. Indian J Orthodont Dentofac Res 2017; 3:48-52.
- Türkkahraman H, Sayın M, Bozkurt FY, et al. Archwire ligation techniques, microbial colonization, and periodontal status in orthodontically treated patients. Angle Orthodont 2005; 75:231-236.
- Papageorgiou SN, Papadelli AA, Eliades T. Effect of orthodontic treatment on periodontal clinical attachment: A systematic review and meta-analysis. Eur J Orthodont 2018; 40:176-194.
- Wennström JL. Mucogingival considerations in orthodontic treatment’, Seminars in orthodontics. Elsevier 1996; 2:46–54.
- Yamaguchi M, Yoshii M, Kasai K. Relationship between substance P and interleukin-1β in gingival crevicular fluid during orthodontic tooth movement in adults. Eur J Orthodont 2006; 28:241–246.
- Sheibaninia A, Saghiri MA, Showkatbakhsh A, et al. Determining the relationship between the application of fixed appliances and periodontal conditions. African J Biotech 2011; 10:16347-16350.
- van Gastel J, Quirynen M, Teughels W, et al. Longitudinal changes in microbiology and clinical periodontal parameters after removal of fixed orthodontic appliances. Eur J Orthodont 2011; 33:15-21.
- Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol 1967; 38:610-616.
- Zachrisson BU, Alnæs L. Periodontal condition in orthodontically treated and untreated individuals II. Alveolar bone loss: Radiographic findings. Angle Orthodont 1974; 44:48-55.
- Boyd RL, Baumrind S. Periodontal considerations in the use of bonds or bands on molars in adolescents and adults. Angle Orthodont 1992; 62:117-126.
- Alves AC. The impact of orthodontic treatment on periodontal support loss. Dent Press J Orthodont 2012; 17:18-20.
- Teles R, Sakellari D, Teles F, et al. Relationships among gingival crevicular fluid biomarkers, clinical parameters of periodontal disease, and the subgingival microbiota. J Periodont 2010; 81:89-98.
- Jäger F, Mah JK, Bumann A. Peridental bone changes after orthodontic tooth movement with fixed appliances: A cone-beam computed tomographic study. Angle Orthodont 2017; 87:672–680.
- Felicita AS. Orthodontic management of a dilacerated central incisor and partially impacted canine with unilateral extraction-A case report. Saudi Dent J 2017a; 9:185–193.
- Felicita AS. Quantification of intrusive/retraction force and moment generated during en-masse retraction of maxillary anterior teeth using mini-implants: A conceptual approach. Dent Press J Orthodont 2017b; 22:47–55.
- Felicita AS. Orthodontic extrusion of ellis class VIII fracture of maxillary lateral incisor-The sling shot method. Saudi Dent J 2018; 30:265–269.
- Felicita AS, Thirumurthi AS, Jain RK. Patient’s psychological response to twin-block therapy. World J Dent 2017; 8:327–330.
- Korath AV, Padmanabhan R, Parameswaran A. The cortical boundary line as a guide for incisor re-positioning with anterior segmental osteotomies. J Maxillofac Oral Surg 2017; 16:248–252.
- Krishnan S, Pandian S, Rajagopal R. Six-month bracket failure rate with a flowable composite: A split-mouth randomized controlled trial. Dent Press J Orthodont 2017; 22:69–76.
- Charles A, Ramani P, Sherlin HJ, et al. Evaluation of dermatoglyphic patterns using digital scanner technique in skeletal malocclusion: A descriptive study. Indian J Dent Res 2018; 29:711-715.
- Pandian KS, Krishnan S, Kumar SA. Angular photogrammetric analysis of the soft-tissue facial profile of Indian adults. Indian J Dent Res 2018; 29:137–143.
- Reddy AK. Comparative evaluation of antimicrobial efficacy of silver, titanium dioxide and zinc oxide nanoparticles against streptococcus mutans. Pesquisa Brasileira Odont Clin Integrada 2018; 18:e4150.
- Chinnasamy A, Ramalingam K, Chopra P, et al. Chronic nail biting, orthodontic treatment and Enterobacteriaceae in the oral cavity. J Clin Exp Dent 2019; 11:e1157-e1162.
- Baxter DH. The effect of orthodontic treatment on alveolar bone adjacent to the cetnento-enamel junction. Angle Orthodont 1967; 37:35–47.
- Hansson S, Halldin A. Alveolar ridge resorption after tooth extraction: A consequence of a fundamental principle of bone physiology. J Dent Biomec 2012; 3.
- McComb JL. Orthodontic treatment and isolated gingival recession: A review. Br J Orthodont 1994; 21:151–159.
- Ogaard B. Marginal bone support and tooth lengths in 19-year-olds following orthodontic treatment. Eur J Orthodont 1988; 10:180–186.
- Bondemark L. Interdental bone changes after orthodontic treatment: A 5-year longitudinal study. Am J Orthodont Dentofac Orthop Elsevier, 1998; 114:25–31.
- Janson G, Bombonatti R, Brandão AG, et al. Comparative radiographic evaluation of the alveolar bone crest after orthodontic treatment. Am J Orthodont Dent Orthop 2003; 124:157-164.
- Ahuja J, Jeyaraj JM, Nayak USK. Evaluation of proximal alveolar bone level changes during orthodontic treatment-A comparative clinical study. J Indian Orthodont Society 2009; 43:48–57.
- Salama H, Salama M. The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: A systematic approach to the management of extraction site defects. Int J Periodont Restorative Dent 1993; 13.
- Adriaens PA, de Boeverw J, Van de Velde F. Comparison of intra-oral long-cone paralleling radiographic surveys and orthopantomographs with special reference to the bone height. J Oral Rehab 1982; 9:355–365.
- Kalbassi S, Chiong FW, Cheau HY, et al. Quantitative three-dimensional assessment of buccal alveolar bone thickness with dental cone-beam computed tomography. Biomed Res 2017; 28.
- Vandenberghe B, Jacobs R, Yang J. Diagnostic validity (or acuity) of 2D CCD versus 3D CBCT-images for assessing periodontal breakdown. Oral Surg Oral Med Oral Pathol Oral Radiol Endodont 2007; 104:395–401.
- Bjerklin K, Ericson S. How a computerized tomography examination changed the treatment plans of 80 children with retained and ectopically positioned maxillary canines. Angle Orthodont 2006; 76:43–51.
Author Info
Nor Syakirah binti Shahroom and Ravindra Kumar Jain*
Department of Orthodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, Chennai, IndiaCitation: Nor Syakirah Binti Shahroom, Ravindra Kumar Jain, A Retrospective Analysis on Interdental Bone Changes After Orthodontic Treatment, J Res Med Dent Sci, 2021, 9 (1): 287-292.
Received: 23-Sep-2020 Accepted: 04-Jan-2021
