Case Reports - (2021) Volume 9, Issue 11
A Rare Case of Leptospirosis with Diffuse Alveolar Haemorrhage
Devang J. Barad*, R. Vedamanickam and Saranya Devi K
*Correspondence: Devang J. Barad, Department of General Medicine, Sree Balaji Medical College and Hospital, Chennai, India, Email:
Abstract
Weil’s disease is the severe form of leptospirosis and is characterized by renal and hepatic involvement and may be accompanied by development of multi-organ dysfunction along with hemorrhagic manifestation. One such serious type of pulmonary involvement is called severe pulmonary hemorrhagic syndrome which is characterized by profuse lung hemorrhages. We wish to present a case of leptospirosis with Diffuse Alveolar Hemorrhage. It is important to remember that a high index of suspicion of leptospirosis along with its timely diagnosis and management with oxygen therapy, antibiotics and intensive care therapy can prevent morbidity and mortality.
Keywords
Leptospirosis, Weil's disease, Hemorrhagic manifestationsIntroduction
Leptospirosis is a zoonotic disease caused by spirochetes. It is usually seen in tropical countries. Weil's disease is a severe form of leptospirosis causing hepatic and renal dysfunction with hemorrhagic manifestations.
It is usually found in tropical countries which rainfall, rice fields and rats, popularly known as 3Rs. It is mostly associated with occupations which are directly in contact with water contaminated by urine of infected animal or by drinking contaminated water.
The organism enters the body through contact with skin or mucous membrane. Hence, the usual suspects are the farmers, field laborers and sanitation workers [1].
On most occasions, leptospirosis presents as an acute febrile illness which is usually undistinguishable from other viral illness. But, occasionally, it may progress to multi-systemic involvement, which is termed as Weil’ss disease. Late diagnosis and delayed treatment are associated with an increase in severity of the disease. Hence, early diagnosis and prompt treatment forms the backbone of management of leptospirosis [2].
A 30 years old male patient, a farmer by occupation, chronic smoker, with no known comorbidities, presented with complaints of high grade continuous fever with chills and rigors with associated myalgia, dyspnea and hemoptysis since 7 days. Initially, he was treated with some oral medications by local doctor on outpatient basis [3]. There was no H/O loss of taste or loss of smell, no H/O chest pain, palpitation, orthopnea, paroxysmal nocturnal dyspnea (PND), no H/O diarrhea, vomiting, reduced urine output, no H/O headache, blurring of vision, altered sensorium, neck rigidity. Physical examination was normal except for the presence of mild icterus. Systemic examination showed bilateral basal crepitations on examination of the respiratory system. Other systemic examination was grossly normal. Upon investigation, CBC showed raised total count of 18100/cu.mm., with 90% neutrophils and thrombocytopenia of 60000/cu.mm.. Serum electrolytes were normal (Figure 1).
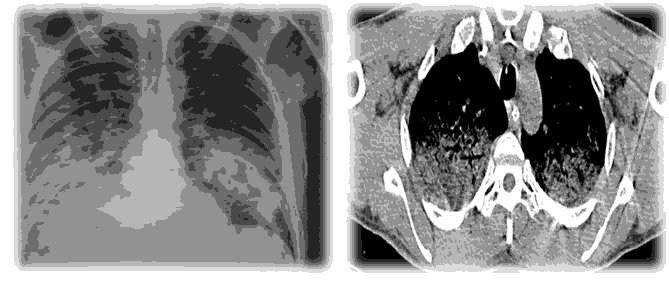
Figure 1: RFT was altered with S.creatinine of 5.2mg/ dl with urea of 120mg/dl.
LFT is altered with S. bilirubin (total) of 6.2 mg/dl which direct bilirubin of 3.9 mg/dl. AST was 170IU and ALT was 158IU. S. total protein and albumin were normal. Urine routine examination showed 2-3 pus cells/hpf and 3-4 RBCs/hpf. COVID-19 RT-PCR was negative.
CXR done showed B/L lower zone non-homogenous opacities. Tests for malaria, typhoid, dengue, and chikunguniya were negative. Viral markers for HIV, HAV, HBV, HCV and HEV were negative [4]. Blood and Urine cultures were sent.
In view of hemoptysis, sputum for AFB was done which was negative. ESR, CRP and S. Procalcitonin were also elevated. Meanwhile, his fever continued and dyspnea increased. He also developed hypotension and his urine output decreased. ABG done showed pH: 7.47, pCO2: 29mmHg, HCO3: 20.1mmol/L, pO2: 65mmHg, SaO2: 94%.
Supportive treatment was started with oxygen inhalation, low-dose vasopressors, judicious IV fluids, IV Azithromycin, anti-fibrinolytics and antipyretics. On further evaluation, USG abdomen was done which was grossly normal.
ECG and 2D echocardiography were grossly normal. Bilateral lower Limb venous Doppler was normal. HRCT Thorax done showed opacities bilateral lower zone with areas of dilatation of bronchi which was suggestive of alveolar hemorrhage.
Intravenous corticosteroid was started (inj. methylprednisolone 500 milligram IV OD for 3 days). 4 units of platelets were also transfused. In the absence of Definitive diagnosis, Biofire panel was sent which came negative. Reviewing the history and the demographic profile of the patient, the differential of leptospirosis raised.
Hence, serum IgM for leptospira was done and the result turned out to be positive [5]. Intravenous Piperacillin-Tazobactam along with oral Doxycycline was started. Gradually, patient responded and became afebrile after 4 days of treatment.
Oxygen support was tapered off and hemoptysis also resolved. LFTs and RFTs also started to improve. After 10 days, the patient was discharge in hemodynamically stable condition. On subsequent follow-up, the patient remained asymptomatic with no residual complaints
Discussion
Leptospirosis is a zoonotic disease caused by spirochete leptospira. Weil’s disease is the severe form of leptospirosis, usually caused by leptospira interrogens serotype interohaemorrhagic. Leptospirosis can present with spectrum of clinical manifestations, ranging from mild cases to even life threatening forms. The usual incubation period is 7 to 10 days. Leptospiral infection in body presents in two distinct phases. First septicemic and second immune phase. Septicemic phase is characterized by the development of constitutional symptoms whereas the immune phase is characterized by organ dysfunction. Weil’s disease is the severe form of leptospirosis and is characterized by renal and hepatic involvement and may be accompanied by development of multi-organ dysfunction along with hemorrhagic manifestation [2]. One such serious type of pulmonary involvement is called severe pulmonary hemorrhagic syndrome which is characterized by profuse lung hemorrhages. Severe pulmonary haemorrhagic syndrome can be one of the causes of death in patients with leptospirosis, unless promptly diagnose and rapidly treated.
Conclusion
Careful History taking with early recognition of organ dysfunction in addition to prompt diagnosis and rapid initiation of appropriate antimicrobial treatment in cases of weil’s disease can drastically improve the patient outcome and can lead to a reduction in mortality.
Conflict of Interest Statement
We declare that we have no conflict of interest.
References
- Luks AM, Lakshminarayanan S, Hirschmann JV. Leptospirosis presenting as diffuse alveolar hemorrhage: Case report and literature review. Chest. 2003; 123:639-643.
- Von Ranke FM, Zanetti G, Hochhegger B, et al. Infectious diseases causing diffuse alveolar hemorrhage in immunocompetent patients: A state-of-the-art review. Lung. 2013; 191:9-18.
- Agrawal VK, Bansal A, Pujani M. A rare case of leptospirosis with isolated lung involvement. Indian J Crit Care Med: Peer-reviewed, official publication of Indian Society of Critical Care Medicine. 2015; 19:174.
- Tatopoulos A, Herbain D, Kazmierczak C, et al. Parenteral use of recombinant activated factor VII during diffuse alveolar hemorrhage secondary to leptospirosis. Inten Care Med. 2010; 36:555.
- Von Ranke FM, Zanetti G, Escuissato DL, et al. Pulmonary leptospirosis with diffuse alveolar hemorrhage: high-resolution computed tomographic findings in 16 patients. J Comput Assist Tomogr. 2016; 40:91-95.
Author Info
Devang J. Barad*, R. Vedamanickam and Saranya Devi K
Department of General Medicine, Sree Balaji Medical College and Hospital, Chennai, IndiaCitation: A Rare Case of Leptospirosis with Diffuse Alveolar Haemorrhage, J Res Med Dent Sci, 2021, 9(11): 382-383
Received: 04-Oct-2021 Accepted: 18-Oct-2021 Published: 25-Oct-2021
