Case Report - (2022) Volume 10, Issue 7
A Rare Case of Goblet Cell Carcinoid
*Correspondence: Sushma Nayar, Department of Pathology, Madha Medical College and Hospital, Chennai, Tamil Nadu, India, Email:
Abstract
Objective: This case is presented for its rarity and importance of examining the tip of the appendix.
Case report: An 18 year’s old female presented with repeated haematuria, urinary tract infection and pain in the right lower abdomen. On MRI, an urachal cyst and acute appendicitis was diagnosed. The patient underwent surgery for the same. Incidentally, the patient was found to have a goblet cell carcinoid of the appendix on histopathological study. Goblet cell carcinoid can present with acute appendicitis as was seen in our patient.
Incidental finding of goblet cell carcinoid is seen in 3% cases. Goblet cell carcinoid can present with pain in right iliac fossa as in our case. Presentation with stage III/IV disease can be seen in 51% to 97% cases as was seen in our patient. Lymph node metastasis was seen in 17-38% cases with involvement of the mesenteric node. The patient did not have carcinoid syndrome. The tumour is generally seen at the tip of the appendix as an ill-defined mass with circumferential and longitudinal extension as was seen in our case. It may involve the whole of the appendix which was not seen in our case where the tumour was confined to the tip.
These tumours generally show strong positivity for CEA, CDX-2 CAM 5.2 and CK. They are inconsistently positive for neuroendocrine markers, though the tumour in our case showed diffuse Chromogranin positivity.
Conclusion: It is important to submit all appendixes for histopathological examination where especially the tip of the appendix should be examined.
Keywords
Carcinoid, Mucins, Chromogranin, AppendixIntroduction
Mucin secreting goblet cell carcinoid are small, detected incidentally, and carry a good prognosis. Their histological features are distinctive and differ from those of ordinary carcinoid tumours and adenocarcinoma [1-6].
Goblet cell carcinoid can present with acute appendicitis as was seen in our patient [1]. Urachal cyst arises from the incomplete obliteration of urachus, which is a primitive structure that connects the umbilical cord to the fetal bladder Urachal cysts are asymptomatic unless infected [2]. Here, we have a case of Goblet cell carcinoid presenting with haematuria and repeated urinary tract infection [7-12].
This case is presented for its rarity and incidental finding and importance of examining the tip of the appendix.
Case Presentation
A 18 years old female was admitted with the chief complaints of pain right lower abdomen, fever, intermittent haematuria, loss of weight, loss of appetite. She had a past history of recurrent haematuria for the past for 8 years, recurrent urinary tract infections in the past. There was no past history of pulmonary tuberculosis. She had a past history of consultation in another hospital at 12 years of age. She was suspected to have urachal cyst but the Imaging studies were inconclusive at that time. This was followed up by Cystoscopy where no abnormal communication was identified. She had a history of reduced food intake, irregular menstrual cycles.
The general examination showed a thinly built female, poorly nourished with a weight of 35 kg. She was pale, with no icterus/cyanosis/clubbing/cervical lymphadenopathy. The vitals were within normal limits.
The systemic examination showed a soft abdomen and no organomegaly. There was localised tenderness in the right iliac fossa. The other systems were normal. The clinical diagnosis was acute appendicitis.
The investigations revealed CBC: Hb–9.8%/TC-10,700/MCV–71/MCH–23 with a normal differential. The random blood sugar was 73 mg/dl. The renal function tests were within normal limits.
The chest X ray PA views was normal. The serology was non-reactive. The CT-Abdomen was normal. The MRI-Abdomen showed a 1 cm Urachal Cyst.
The final pre-op diagnosis was: Acute Appendicitis and Remnant Urachal Cyst Laparoscopic Urachal cyst excision and Appendectomy was done and sent for Histopathological examination. Preoperatively, the appendix appeared grossly unremarkable.
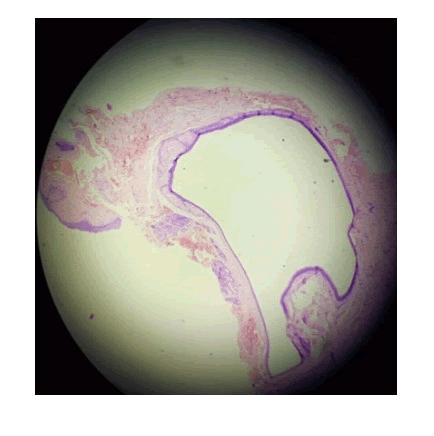
Histopathology Study showed: Urachal cyst excised specimen showed a cyst lined by transitional epithelium (Figure 1).
Figure 1: Haematoxylin and eosin stained section (10Xx4X) showing urachal cyst lined by transitional epithelium.
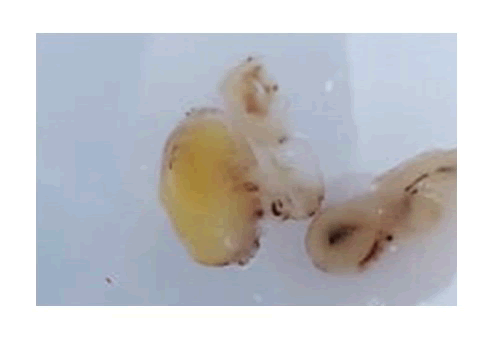
Appendicectomy specimen showed a Goblet Cell Carcinoid. Grossly, the appendix appeared shrivelled up with a yellowish tip measuring 1X1 cm (Figure 2).
Figure 2: Gross appearance of the appendix with a yellow tip.
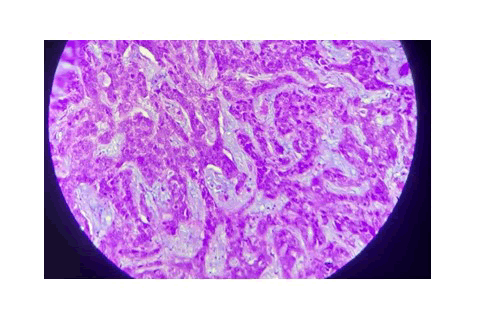
Three sections were taken one each from the tip; mid and base of the appendix. Tumour was seen at the tip with circumferential involvement. The tumour was composed of nests, trabaculae and cords of atypical cells separated by extra-cellular pools of mucin. The atypical cells showed mild atypia, a vesicular nucleus and “salt and pepper” chromatin and eosinophilic vacuolar cytoplasm. The tumour was seen invading the muscularis layer and extending up to the serosa and was not seen infiltrating the periappendiceal fat. The tumour showed characteristic nesting pattern at the periphery of the tumour. The tumour showed both intra and extra cellular pools of mucin (Figure 3).
Figure 3: Haemaoxylin and eosin stained section (10XX40X) showing intra and extracellular pools of mucin.
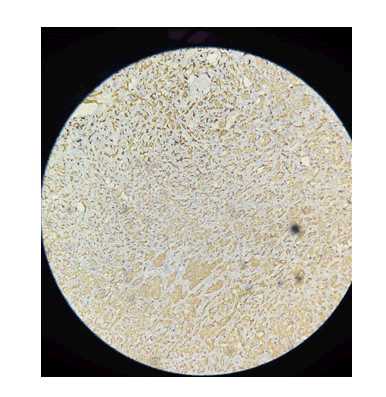
At the periphery of the lesion some desmoplastic was seen. Mitotic Figures 3-4/10 hpf was seen. Paneth cell metaplasia was seen. The immunohistochemistry showed cells to be Chromogranin diffusely positive (Figure 4) and Ki 67 index was 3-4%.
Figure 4: Immunohistochemistry with Chromogranin (10XX10X) showing diffuse Chromogranin positivity.
Thus, the tumour was classified as “Goblet cell carcinoid” Grade II pT3 since there was no breach of the serosa. Any perineural or vascular invasion or periappendiceal involvement of the appendix by the tumour was not seen as is commonly seen in these tumours [2].
Discussion
The age at presentation of Goblet cell carcinoid is unusual in our case (18 years) [3,4]. It has been reported to occur in an older age group with equal predilection of the sexes. Half the female patients presented with metastasis to the ovary [5]. Our patient’s ovary was free of disease.
Goblet cell carcinoid can present with pain in right iliac fossa as in our case [6-8]. Incidental finding of goblet cell carcinoid is seen in 3% cases [5]. Presentation with stage III/IV disease can be seen in 51% to 97% [8,9], cases as was seen in our patient. Lymph node metastasis was seen in 17-38% cases with involvement of the mesenteric node [5,8]. The patient did not have carcinoid syndrome [9,10].
These tumour is generally seen at the tip of the appendix as an ill-defined mass with circumferential and longitudinal extension as was seen in our case [5]. It may involve the whole of the appendix which was not seen in our case where the tumour was confined to the tip. The mucosa was spared as was seen in our case.
Microscopically, goblet cell carcinoid has been divided into Grade I, II and III. Grade I being cells with minimal atypia, mitotic figures <2/hpf and Ki 67 index<2%. Grade II having cells with moderate atypia, mitotic figures between 2-20/hpf, Ki 67 index 3-20% and Grade III being cells showing marked atypia with mitotic figures >20/hpf and Ki67 index>20% [10]. Our patient had Grade II tumour.
This tumour’s generally show strong positivity for CEA, CDX-2 CAM 5.2 and CK. They are inconsistently positive for neuroendocrine markers [6,12], though the tumour in our case showed diffuse Chromogranin positivity [5].
A urachal cyst is a collection of tissue and fluid between the bladder and the umbilicus. The cyst forms in the remnants of the urachus, a structure normally present in a fetus that usually closes before birth. In some infants, the closure doesn't occur.
The urachal cyst remains largely asymptomatic unless infected. Infected urachal cysts present with acute symptoms such as suprapubic pain, dysuria, fever, nausea, vomiting, haematuria, pelvic pain, and purulent umbilical discharge like it did in our patient who had haematuria and repeated urinary tract infection [2].
On post-operative follow-up the patient had gained 3 kg weight and did not have any abdominal mass/pain [12], as the tumour was confined to the appendix.
Conclusion
It is important to submit all appendixes for histopathological examination where especially the tip of the appendix should be examined.
References
- Roy RP, Runjan C. Goblet cell carcinoid tumours of the appendix: an overview.
- Kwok CM. Infected urachal cyst in an adult: A Laparoscopic Approach. Case Rep Gastroenterol 2016; 10:269â??274.
- Rindi G, Luinetti O, Cornaggia M, et al. Three subtypes of gastric argyrophil carcinoid and the neuroendocrine carcinoma: a clinicopathologic study. Gastroenterology 1993; 104:994-1006.
- Burke AP, Sobin LH, Federspiel BH, et al. Goblet cell carcinoids and related tumors of the vermiform appendix. Am J Clin Pathol 1990; 94:27-35.
- Tang LH, Shia J, Soslow RA, et al. Pathologic classification and clinical behaviour of the spectrum of goblet cell carcinoid tumors of the appendix. Am J Surg Pathol. 2008; 1429â??1443.
- Warkel RL, Cooper PH, Helwig EB. Adenocarcinoid, a mucin-producing carcinoid tumour of the appendix: a study of 39 cases. Cancer 1978; 2781â??2793.
- Donnell ME, Carson J, Garstin WI. Surgical treatment of malignant carcinoid tumours of the appendix. Int J Clin Pract 2007;431â??437.
- Pham TH, Wolff B, Abraham SC, et al. Surgical and chemotherapy treatment outcomes of goblet cell carcinoid: a tertiary cancer center experience. Ann Surg Oncol 2006; 370â??376.
- Mc Cusker ME, Cote TR, Clegg LX, et al. Primary malignant neoplasms of the appendix: a population-based study from the surveillance, epidemiology and end-results program, 1973-1998. Cancer 2002; 3307â??3312.
- Anderson NH, Somerville JE, Johnston CF, et al. Appendiceal goblet cell carcinoids: a clinicopathological and immunohistochemical study. Histopathology 1991; 61â??65.
- Van Eeden S, Offerhaus GJ, Hart AA, et al. Goblet cell carcinoid of the appendix: a specific type of carcinoma.Histopathology 2007; 763â??773.
- Tang LH, Shia J, Soslow RA, et al. Pathologic classification and clinical behavior of the spectrum of goblet cell carcinoid tumors of the appendix. Am J Surg Pathol 2008; 1429â??1443.
Author Info
Department of Pathology, Madha Medical College and Hospital, Chennai, Tamil Nadu, IndiaCitation: Sushma Nayar, A Rare Case of Goblet Cell Carcinoid, J Res Med Dent Sci, 2022, 10 (7): 148-155.
Received: 09-May-2022, Manuscript No. JRMDS-22-55529; , Pre QC No. JRMDS-22-55529; Editor assigned: 12-May-2022, Pre QC No. JRMDS-22-55529; Reviewed: 26-May-2022, QC No. JRMDS-22-55529; Revised: 02-Jul-2022, Manuscript No. JRMDS-22-55529; Published: 09-Jul-2022