Research Article - (2023) Volume 11, Issue 1
A Prospective Randomized Study to Compare the Effect of 0.125% Bupivacaine with Fentanyl or without Fentanyl via Extrapleural Paravertebral Catheter for Continuous Postoperative Analgesia in Thoracic Surgeries
Brejendra Singh Gill*, Kaushal kabir, Madhuri Bharang and KK Arora
*Correspondence: Dr. Brejendra Singh Gill, Department of Anaesthesiology, MY Hospital and MGM Medical College, Indore, MP, India, Email:
Abstract
The most common problem of any surgical intervention is postoperative pain, which requires appropriate analgesia. The differential responses to the tissue injury during incision are often influenced by many variables including global (i.e. age, personality, gender, surgical approach, genetic, preexisting pain syndrome) and specific (i.e. anxiety, anger, fear, depression, psychological factors). Pain is a complex process for the patient and the Anaesthesiologist who are tasked with managing it. Four processes cause pain perception: Transduction, transmission, modulation and perception. Postoperative pain is related to many factors, including the amount of soft tissue injury, resulting inflammation and rib injury as in the case of a thoracic surgical procedure.
Keywords
Bupivacaine, Thoracic surgeries, Surgery, Manuka tree, SPSS
Introduction
Post-thoracotomy pain is one of the severe sorts of postoperative pain. The insufficient treatment of post-thoracotomy pain results in reduced pulmonary compliance, inability to breathe deeply or cough forcefully and retention of secretions, atelectasis and pneumonia. Several techniques are available for management of pain in thoracic surgery, including paravertebral, intercostals, interpleural and epidural blocks with local anaesthetics and opioids [1].
Thoracotomy pain arises due to intercostal nerve damage. Due to this pain, respiratory functions compromise leading to post-op pulmonary complications and patient stay for a long time in hospital thus increases the burden. There are many drugs and techniques for relief of postoperative pain, regional technique or systemic analgesics are common. Systemic opioids carry the risk of respiratory depression and NSAIDS are poor analgesics for thoracotomy incision. Extrapleural paravertebral catheter is an alternative technique to decrease the pain in thoracotomy [2].
Numerous studies have evaluated the efficacy of combined narcotic/local anesthetic epidurals and found them to provide excellent pain relief. An alternative method of providing post-thoracotomy analgesia is the use of continuous infusion of local anesthetics via extrapleural catheter. This form of analgesia shows excellent results with minimal complications. For the placement of extrapleural catheters an 18 gauge tuohy needle is placed through the chest wall at a convenient site two interspaces below the thoracotomy incision and few centimeters away from the chest tube site. The needle’s stylet is removed, and an epidural catheter is passed through the needle and is placed inside the extrapleural space. We carried out this study to prospectively compare the effect of 0.125% bupivacaine with Fentanyl or without fentanyl via extrapleural paravertebral catheter insertion for continuous postoperative analgesia in patients undergoing thoracic surgeries [3].
Materials and Methods
This prospective, randomized, comparative study was conducted for a period of one year in the Department of Anaesthesiology, MY Hospital and MGM medical college, Indore [4].
Sample size
The study was comprised of 40 patients divided in to two groups of 20 each scheduled for elective thoracic surgery under general anaesthesia. The sample size was calculated using G* power, software version 3.1.9.2 and 95% confidence level and 80% power for two groups using ‘t’ test (mean difference between two independence groups) for large effect size ‘d’ (0.8) [5].
Inclusion criteria
• Patients posted for thoracic surgery (decortications, pleurectomy).
• Age group 18-65 year of age.
• ASA grade I, II.
Exclusion criteria
• Patient refusal.
• ASA grade III, IV.
• Hypersensitivity to local anaesthetics.
• Coagulation profile deranged.
• Platelet count <50000.
• Non intact pleura at paravertebral space.
• Adhesion, infection, tumor, scarring in paravertebral space.
Ethical clearance
The study was approved by the institutional ethics and scientific review committee of MGM Medical College and MY hospital Indore prior to commencement [6].
Randomization
Patients were randomly allocated by chit method just before surgery to group 1(B) or group 2 (B+F) comprising 20 patients each [7].
Procedure
After obtaining written informed consent and recording vitals and nil by mouth status as per institutional protocol, all patients were started intravenous fluids. Routine monitors were attached (pulse oximeter for SpO2, Heart Rate (HR), non-invasive blood pressure and ECG). General anaesthesia was given as standard institutional protocol. Intubated with appropriate size double lumen endotracheal tube after giving muscle relaxant. Thoracotomy was done. An extrapleural catheter was inserted by the surgeon under direct vision external to the parietal pleura just before thoracotomy closure. Then an infusion of 0.125% Bupivacaine @0.15 ml/kg/hr in group 1 (B) and 0.125% Bupivacaine with fentanyl 2 mcg/ml @0.15 ml/kg/hr in group 2 (B+F) was started. Then dose or rate of infusion was decreased after 2 days or chest drain removal, as pain subsided [8].
Assessment of postoperative pain and management
The pain score using visual analogue scale was assessed at 1, 6, 12, 18, 24, 48 and 72 hours after the surgery.
Patients who complained of pain with a VAS score of more than or equal to 4 were given Inj. Tramadol 1 mg/kg (rescue analgesia). The peak expiratory flow rate assessed at 12, 24, 48, 72 hrs. The hemodynamic changes and adverse events including sedation, hypotension, nausea, vomiting, pruritus, etc. were assessed in all the patients at 1, 6, 12, 18, 24, 48 and 72 hrs [9].
Statistical analysis
Data was initially collected in the customized proforma designed for the purpose of the study. Then this data transferred to Microsoft Excel for analysis and online statistical software graph pad and Epi info was used for calculating p value. Comparison of means between the two group was done using unpaired‘t’ test. A p value of <0.05 was considered as statistically significant. The final data was presented in the form of tables and (Figures 1-12) [10].
Figure 1: Pie diagram showing distribution according to group.
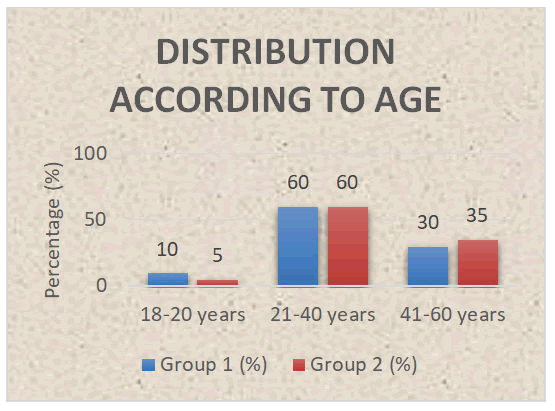
Figure 2: Bar diagram showing distribution according to age.
Figure 3: Bar diagram showing distribution according to gender.
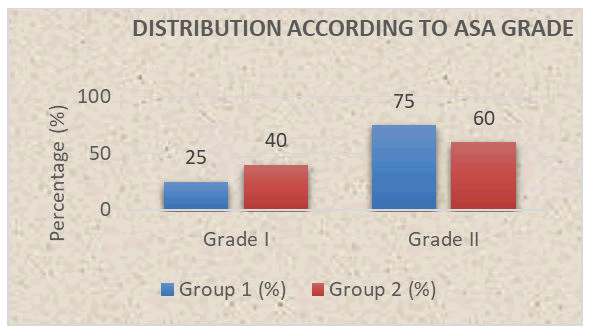
Figure 4: Bar diagram showing distribution according to ASA grade.
Figure 5: Line diagram showing comparison of mean heart rate between the two groups.
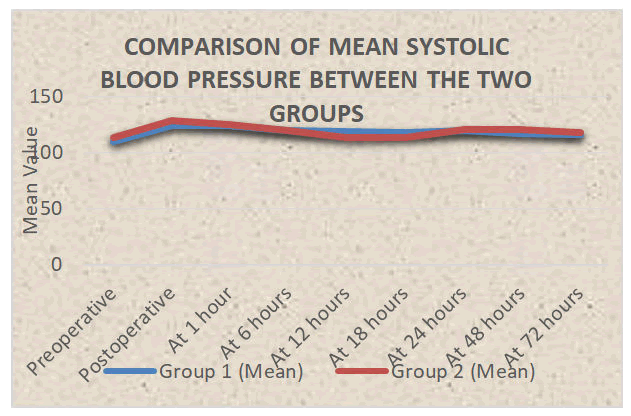
Figure 6: Line diagram showing comparison of mean systolic blood pressure between the two groups.
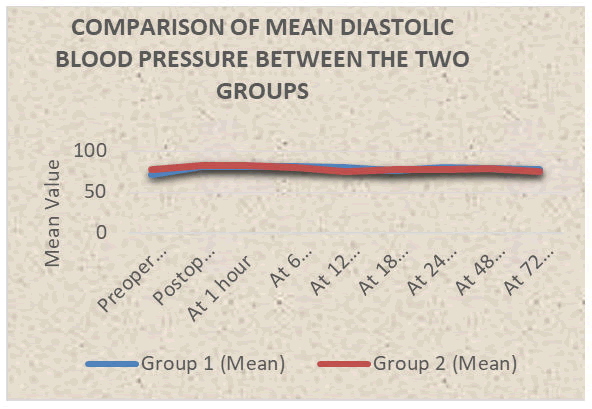
Figure 7: Comparison of mean diastolic blood pressure between the two groups.
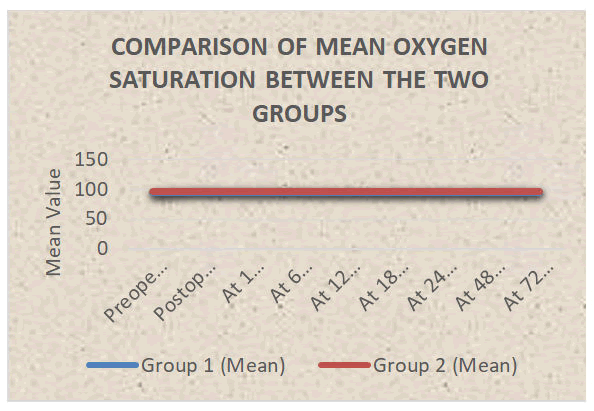
Figure 8: Comparison of mean SpO2 between the two groups.
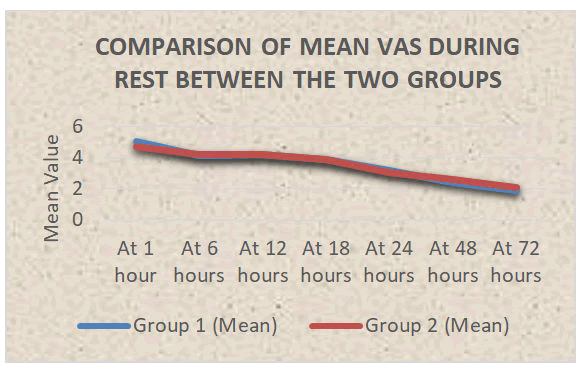
Figure 9: Comparison of mean VAS during rest between the two groups.
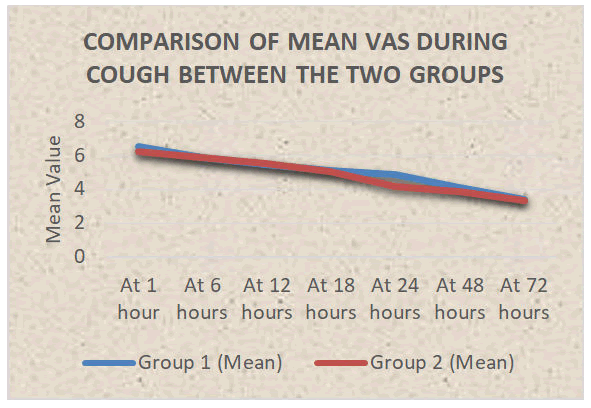
Figure 10: Comparison of mean VAS during cough between the two groups.
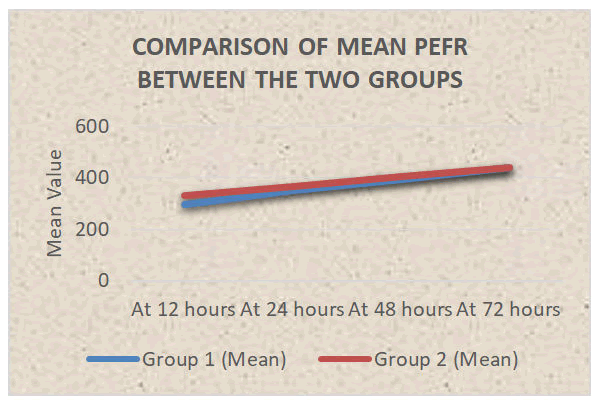
Figure 11: Comparison of mean PEFR between the two groups.
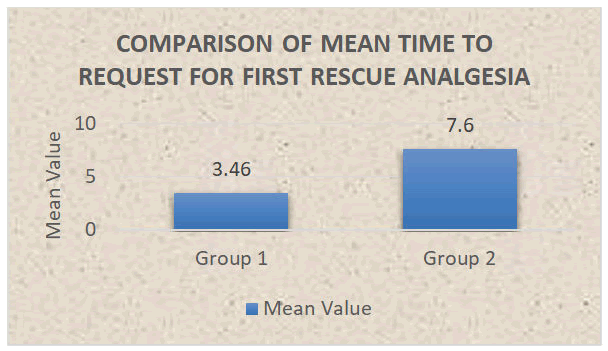
Figure 12: Bar diagram showing comparison of mean time to request for first rescue analgesia.
Results and Discussion
Thoracic surgeries are associated with severe postoperative pain. Pain is mainly associated with the incision that is made. Control of pain following a thoracic surgery is very important concern as uncontrolled pain may lead to respiratory complications like atelectasis, diaphragmatic dysfunction, respiratory failure, splinting, and ineffective cough resulting in pneumonia. Local anesthetics were given through extrapleural catheter to reduce postoperative pain in thoracic surgery patients. In our study the patients were comparable with respect to age, gender and demography wise distribution. The mean preoperative heart rate was 100.2 ± 12.76 per minute In group 1 (B) and 94.4 ± 6.95 per minute in group 2 (B+F). The mean heart rate was comparable between the two groups at preoperative, postoperative, at 1 hour and at 6 hours postoperatively (P>0.05), while the mean heart rate was significantly lower in group 2 (B+F) at 12 hours, 18 hours, 24 hours and at 72 hours postoperatively (P<0.05) in comparison to group 1 (B).
The mean systolic blood pressure, mean diastolic blood pressure, mean oxygen saturation and mean pain score (VAS) both during rest and during cough were comparable between the two groups at all the time intervals (P>0.05). The mean VAS during rest at 1 hour postoperatively was 5.1 ± 0.91 In group 1 (B), and 4.7 ± 1.3 In group 2 (B+F), the mean pain score (VAS) was comparable in both the groups in all time intervals. However the pain is controlled in both the groups effectively. In group 1 (B), the mean VAS during cough at 1 hour postoperatively was 6.5 ± 0.83, and In group 2 (B +F), the mean VAS during cough at 1 hour postoperatively was 6.2 ± 1.01, The mean VAS during cough was comparable between the two groups at all-time intervals (P>0.05) [11].
The mean PEFR was also comparable between the two groups at 12 hours (P=0.114), at 24 hours (P=0.432), at 48 hours (P=0.495) and at 72 hours (P=0.832). In both the groups, we have noticed, improvement in PEFR from 12 hours to 72 hours that is in group1 (B) 300.00 ± 79.07 L/min at 12 hours and 440.50 ± 63.12 L/min at 72 hours while in group 2 (B+F) 332.50 ± 42.41 L/min at 12 hours and 444.00 ± 36.91 L/min at 72 hours. From above values, we observed improvement in lung functions.
These findings correlate with and in which they found that extra-pleural infusion of local anaesthetics is a simple and easy technique, with low risk of complications and provides effective pain relief as well as an improvement in post-operative pulmonary function.
The mean time taken for request to first analgesia in group 1 (B) was 3.46 ± 4.22 hours and in group 2 (B+F) was 7.60 ± 6.95 hours and this mean time was found to be statistically comparable between the two groups (P=0.091). The reason for non-significant could be due to less number of patients requesting for rescue analgesia in both the groups. There were no infusion related complications and toxicity in our both groups even after 72 hours of bupivacaine infusion. Safety profile was documented in who also not found any toxicity even after 120 hours of bupivacaine infusion. Safety profile was also documented in this study they found no associated adverse effects of use of extrapleural bupivacaine infusion [12].
Rationale of study
Adjuvant increases the efficacy and potency of local anesthetics drugs thus improves the analgesia and prolongs the duration of analgesia. Opioids are usually used as additive, Lipophilic drugs like Fentanyl has less side effects and improves analgesia. By this study we want to compare the quality and duration of analgesia. As pain decreases, the respiratory function subsequently improves and patient gets discharge earlier from hospital and the hospital burden also decreases in terms of stay and cost [13].
Conclusion
It can be concluded that continuous extrapleural paravertebral catheter infusion of local anaesthetics is effective in the management of postoperative pain in patients undergoing thoracic surgeries. Group 2 (B+F) has longer duration of analgesia and later requirement of first rescue analgesia, better PEFR compared to group 1 (B), though it is not statistically significant.
Limitation of Study
Although this study has tried to meet its aims and objectives in all aspects, there are few limitations to it. We conducted a single-centre study, we did not compare the efficacy of extrapleural catheter with thoracic epidural and inter pleural analgesia in our study, total sample size 40 (20 in each group), if sample size are large then results will be more precise. To overcome these limitations, a multicentric study with larger sample size is needed to obtain more conclusive results.
Conflict of Interest
None.
Source of Funding
None.
References
- Eccleston C. Role of psychology in pain management. Br J Anaesth 2001; 87:144-152. [Crossref] [Google Scholar] [PubMed]
- Perttunen K, Nilsson E, Heinonen J, et al. Extradural paravertebral and intercostal nerve blocks for postthoracotomy pain. Br J Anaesth 1995; 75:541-547. [Crossref] [Google Scholar] [PubMed]
- Kolettas A, Lazaridis G, Baka S, et al. Postoperative pain management. J Thora Dis 2015; 7:S62-S72. [Crossref] [Google Scholar] [PubMed]
- Richardson J, Sabanathan S, Eng J, et al. Continuous intercostal nerve block versus epidural morphine for postthoracotomy analgesia. Ann Thorac Surg 1993; 55:377-380. [Crossref] [Google Scholar] [PubMed]
- Kaiser AM, Zollinger A, de Lorenzi D, et al. Prospective, randomized comparison of extrapleural versus epidural analgesia for postthoracotomy pain. Ann Thorac Surg 1998; 66:367-372. [Crossref] [Google Scholar] [PubMed]
- Faber LP. Epidural analgesia: Different strokes for different folks. Ann Thorac Surg 1990; 50:862-863. [Crossref] [Google Scholar][PubMed]
- Matthews PJ, Govenden V. Comparison of continuous paravertebral and extradural infusions of bupivacaine for pain relief after thoracotomy. Br J Anaesth 1989; 62:204-205. [Crossref] [Google Scholar] [PubMed]
- Deneuville M, Bisserier A, Regnard JF, et al. Continuous intercostal analgesia with 0.5% bupivacaine after thoracotomy: A randomized study. Ann Thorac Surg 1993; 55:381-385. [Crossref] [Google Scholar] [PubMed]
- Cook E, Downs C. Analgesia after thoracotomy-the role of the extrapleural paravertebral catheter. Aus Anaest 2005; 103-117. [Google Scholar]
- Eng J, Sabanathan S. Continuous extrapleural intercostal nerve block and post-thoracotomy pulmonary complications. Scand J Thorac Cardiovasc Surg 1992; 26:219-223. [Crossref] [Google Scholar] [PubMed]
- Barron D, Tolan M, Lea R, et al. A randomized, controlled trial of continuous extra-pleural analgesia postthoracotomy: Efficacy and choice of local anaesthetic. Eur J Anaesthesiol 1999; 16:236-245. [Crossref] [Google Scholar] [PubMed]
- Berrisford RG, Sabanathan S, Mearns S, et al. Hamdi plasma concentrations of bupivacaine and its enantiomers during continuous extrapleural intercostal nerve block British. J Anaest 1993; 70:201-204. [Crossref][Google Scholar][PubMed]
- Carabine UA, Gilliland H, Johnston JR, et al. Pain relief for thoracotomy. Comparison of morphine requirements using an extrapleural infusion of bupivacaine. Reg Anest 1995; 20:412-417. [Google Scholar][PubMed]
Author Info
Brejendra Singh Gill*, Kaushal kabir, Madhuri Bharang and KK Arora
Department of Anaesthesiology, MY Hospital and MGM Medical College, Indore, MP, IndiaCitation: Brejendra Singh Gill, Kaushal kabir, Madhuri Bharang, KK Arora, A Prospective Randomized Study to Compare the Effect of 0.125% Bupivacaine with Fentanyl or without Fentanyl via Extrapleural Paravertebral Catheter for Continuous Postoperative Analgesia in Thoracic Surgeries, J Res Med Dent Sci, 2023, 11 (01): 279-283.
Received: 20-Dec-2021, Manuscript No. JRMDS-22-50234; , Pre QC No. JRMDS-22-50234 (PQ); Editor assigned: 24-Dec-2021, Pre QC No. JRMDS-22-50234 (PQ); Reviewed: 07-Jan-2022, QC No. JRMDS-22-50234; Revised: 02-Jan-2023, Manuscript No. JRMDS-22-50234 (R); Published: 30-Jan-2023