Research - (2020) Advances in Dental Surgery
A Knowledge Attitude and Practice Survey on Biomimetic Materials Used in Conservative Dentistry and Endodontics Among Dentist
Krishnakanth Jaju and Iffat Nasim*
*Correspondence: Iffat Nasim, Department of Conservative Dentistry and Endodontics, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, India, Email:
Abstract
The purpose of this survey was to assess the knowledge and opinion toward Biomimetic materials used in conservative dentistry and endodontics among the Endodontic postgraduate students, endodontist, intern and general practitioners of India. A questionnaire consisting of 24 questions was formulated and circulated through electronic media among endodontist, interns, endodontic postgraduate students & general practitioners of India. These questions were based on their knowledge and opinion regarding the biomimetic materials used in conservative dentistry & endodontic procedures. This survey revealed that more than three-fourth (96.1%) of the respondents had knowledge about biomimetic materials used in conservative dentistry & endodontics. Most of the respondents (81.2%) felt that this treatment strategy should be incorporated into dentistry. However, the results indicated that one-third (87.8%) of the respondents were using biomimetic materials in their regular practice. The results reflected that endodontists were well versed with the biomimetic materials and were optimistic of implementing it, a need for additional training was felt.
Keywords
Knowledge, Postgraduate students, Endodontist, Biomimetic material, Endodontics
Introduction
In the field of conservative dentistry and endodontics, biomimetic materials have been used for regeneration, repair, and reconstruction. Biomimetic materials are defined as a material that can induce a response from living tissue, organisms, or cells such as the formation of hydroxyapatite. They directly act on vital tissues and promote tissue healing and repair and maintain pulp vitality. It should be bactericidal, bacteriostatic, and sterile in nature, as its ideal requirements. The term biomimetic suggests imitation of nature in other words the material should be in some way reproducing one or more natural phenomena within a biological situation. It also implies that the material will be biocompatible i.e. biologically acceptable to and not rejected by adjacent vital tissue following placement [1]. Such a material may cause low transient, inflammatory response, but it will not release chemical irritants into the vicinity. The secondary meaning of biomimetics refers to mimicking or recovery of the original tooth both in form as well as function, Biomimetics is the study of function, formation or structure of biologically produced substances and materials and biological mechanisms and processes for the purpose of synthesizing similar products by several research in dentistry have evolved with the prospect to mimic oral structures, submicroscopic structures with unique relevance to novel biomaterials [2,3]. In clinical dentistry we are challenged to design and fabricate new biomaterials that can mimic the tooth both in form and function [2-5]. These include:
Glass ionmer cements.
Calcium hydroxide.
Mineral trioxide aggregate.
Calcium phosphate.
Bioactive glass.
Emdogain.
Composites.
Ceramics.
Biodentinethi.
In future, Biomimetic materials will become extremely popular and it is speculated to see unparalleled advances in this field. Hence, it is important to understand what the future endodontists think in this regard [6]. We have numerous highly cited publications on welldesigned clinical trials and lab studies [7-22]. This has provided the right platforms for us to pursue the current study. Our aim is to evaluate the level of awareness regarding these materials among endodontic postgraduate students, endodontist, general practitioners of India and their willingness to practice it.
Mechanism of action
The performance of bioactive materials is largely attributed to its capacity to spontaneously produce an appetite layer when in contact with phosphate-containing physiological fluids [23,24,25,26]. The apatite formation is promoted via an interaction of Ca2+ released from the material with phosphates and is considered as the basis of several inorganic biomaterials such as glass ceramics. Bioactive materials induce cytological and functional changes within pulpal cells, resulting in the formation of reparative dentin at the surface of exposed dental pulp in vital pulp therapy. When placed, it helps in proliferation, migration, and differentiation of odontoblast-like cells that produce a collagen matrix. This unmineralized matrix is then mineralized by osteodentin initially and then by tertiary dentin formation [27].
Materials and Methods
A cross-sectional survey was conducted across dental colleges of India in October 2019. A questionnaire consisting of 24 questions was formulated. These questions can be divided into three parts, namely knowledge, attitude, and practice. Based on responses from the endodontic postgraduate students, Endodontist, General practitioners & Interns to this multiple choice-based questionnaire, the survey was analyzed.This questionnaire was circulated among the endodontic postgraduate students through electronic media after approval of the ethical committee of Saveetha Dental College, Chennai.
Results and Discussion
Of 200 questionnaires sent, 155 were filled and sent back yielding a response rate of 77.5%. Among the participants, 60% were males, 40% were females. All the participants provided a reply for each question. 85 (54.8%) Endodontist, 55 (35.5%) Endodontic postgraduates, 15 (9.7%) of General practitioners participated in the survey regarding biomimetic materials used in conservative dentistry & endodontics. Majority of the participants 75% had knowledge regarding biomimetic materials used in conservative dentistry &endodontics (Table 1). About 80% of them were aware of advantages and disadvantages of biomimetic materials (Table 2). The participants (70%) were highly positive about introduction of biomimetic materials in conservative dentistry and endodontics (Table 3) (Figures 1-6).
| No | Questions | Options | % of respondents n (%) |
|---|---|---|---|
| 1 | Are u aware of biomimetic materials used in conservative dentistry & endodontics | Yes | 148(96.1%) |
| No | 6(3.9%) | ||
| 2 | Biomimetic materials are | Materials that stimulates tooth material but additionally some bioactive properties are present | 121(78.6%) |
| Materials used in apexogenesis and apexification cases | 21(13.6%) | ||
| Materials in which bio active materials are added | 9(5.8%) | ||
| Materials which have ability to reproduce by themselves | 3(1.9%) | ||
| 3 | Which of the following are biomimetic material | Bio dentine | 13(8.4%) |
| MTA | 11(7.1%) | ||
| GIC | 14(9.1%) | ||
| Calcium Hydroxide | 6(3.9%) | ||
| All of the above | 110(71.4%) | ||
| 4 | Which of the following are uses of MTA | Apexification | 3(1.9%) |
| Apexogenesis | 7(4.5%) | ||
| Root perforation repair | 17(11%) | ||
| Pulp Capping | 4(2.6%) | ||
| All of the above | 123(79.9%) | ||
| 5 | Which of the following is advantages of MTA | Handling properties | 35(22.7%) |
| Setting time | 3(1.9%) | ||
| Vasoconstrictive | 114(74%) | ||
| High cost | 2(1.3%) | ||
| 6 | Which of the following is disadvantage of MTA | More radio opaque | 1(0.6%) |
| Alkaline pH | 3(1.9%) | ||
| Long setting time | 145(94.2%) | ||
| Hardens in presence of moisture | 5(3.2%) | ||
| 7 | Are you aware of the use of bioactive glass in conservative dentistry? | Class V cavity | 9(5.8%) |
| Treatment of Dentin hypersensitivity | 139(90.3%) | ||
| Pit and fissure sealants | 3(1.9%) | ||
| Bleaching discoloured teeth | 3(1.9%) |
Table 1: Shows knowledge-based questions towards digital dentistry.
| No | Questions | Options | % of respondents n (%) |
|---|---|---|---|
| 1 | How often do you use bio dentin in the management of deep carious lesion | In every case | 5(3.2%) |
| In most cases | 19(12.3%) | ||
| In some cases | 121(78.6%) | ||
| Don’t use | 9(5.8%) | ||
| 2 | Which material would you prefer in root resorption cases | Gutta Percha | 7(4.5%) |
| Bio dentine | 13(8.4%) | ||
| Root end filling with MTA and obturation with G.P | 133(86.4%) | ||
| GIC | 1(0.6%) | ||
| 3 | Which pulp capping agent do you often prefer | Bio dentine | 32(20.8%) |
| ZOE | 5(3.2%) | ||
| MTA | 115(74.7%) | ||
| Zinc Phosphate | 2(1.3%) | ||
| 4 | Do you evaluate success rate in follow-up visits after use of MTA in apexification cases? | Yes | |
| 148(96.1%) | |||
| No | 6(3.9%) | ||
| 5 | Do u think bio dentin is an effective material in deep caries management | Handling properties | 35(22.7%) |
| Setting time | 3(1.9%) | ||
| Vasoconstrictive | 114(74%) | ||
| High cost | 2(1.3%) | ||
| 6 | Do u recommend use of biomimetic materials in endodontics | Strongly Agree | 125(81.2%) |
| Agree | 29(18.8%) | ||
| Strongly Disagree | ------- | ||
| Disagree | ------- | ||
| 7 | Would you prefer biomimetic material in your regular practice | Yes | 149(96.8%) |
| No | 5(3.2%) |
Table 2: Shows Attitude based questionnaires towards digital dentistry.
| No | Questions | Options | % of respondents n (%) |
|---|---|---|---|
| 1 | Which of the following biomimetic materials do you think is better in endodontics | Bio dentine | 41(26.6%) |
| Bioaggregate | 8(5.2%) | ||
| MTA | 104(67.5%) | ||
| Calcium Hydroxide | 1(0.6%) | ||
| 2 | Which biomimetic material do you think showed higher clinical and radiographic success in root perforation repair cases | Decalcified Freezed Dried Bone | 1(0.6%) |
| Bio dentine | 37(24%) | ||
| GIC | 5(3.2%) | ||
| MTA | 111(72.1%) | ||
| 3 | How often do you use biomimetic material in your regular practice | 0 cases per month | 148(96.1%) |
| 2-5 cases per month | - | ||
| 5-7 cases per month | - | ||
| 7 – 10 cases per month | 6(3.9%) | ||
| 4 | Of the following most commonly used biomimetic material in your regular clinical practice is | MTA | 109(70.8%) |
| Biodentine | 24(15.6%) | ||
| Calcium Hydroxide | 20(13%) | ||
| Bioaggregate | 1(0.6%) | ||
| 5 | Which sealer do you use during root canal treatment | ZOE | 124(80.5%) |
| Ah plus | 20(13%) | ||
| Endosequence BC sealer | 6(3.9%) | ||
| Calcium Hydroxide | 4(2.6%) | ||
| 6 | Which obturating material do you use in root canal treatment | Gutta percha | 126(81.8%) |
| MTA | 27(17.5%) | ||
| Resilon | ------- | ||
| Bioceramic Guttapercha | 1(0.6%) |
Table 3: Shows Practice based questionnaires towards digital dentistry.
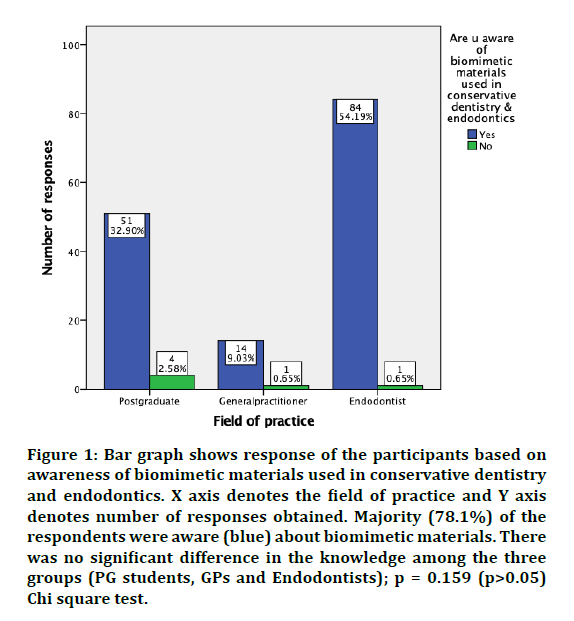
Figure 1: Bar graph shows response of the participants based on awareness of biomimetic materials used in conservative dentistry and endodontics. X axis denotes the field of practice and Y axis denotes number of responses obtained. Majority (78.1%) of the respondents were aware (blue) about biomimetic materials. There was no significant difference in the knowledge among the three groups (PG students, GPs and Endodontists); p = 0.159 (p>0.05) Chi square test.
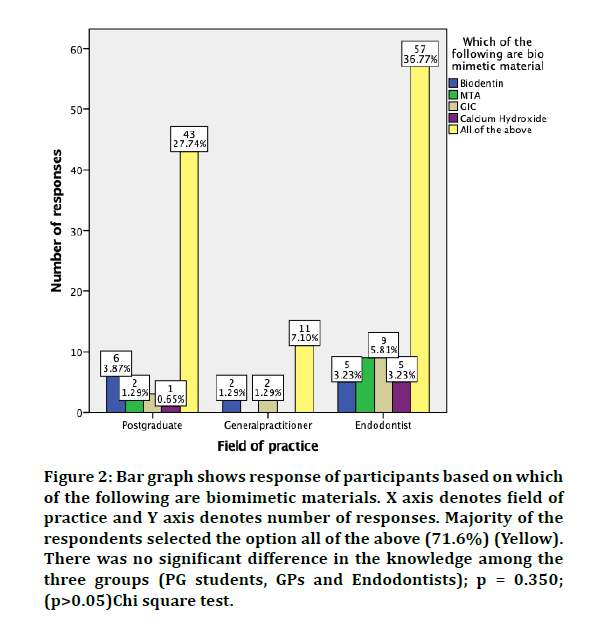
Figure 2: Bar graph shows response of participants based on which of the following are biomimetic materials. X axis denotes field of practice and Y axis denotes number of responses. Majority of the respondents selected the option all of the above (71.6%) (Yellow). There was no significant difference in the knowledge among the three groups (PG students, GPs and Endodontists); p = 0.350; (p>0.05)Chi square test.
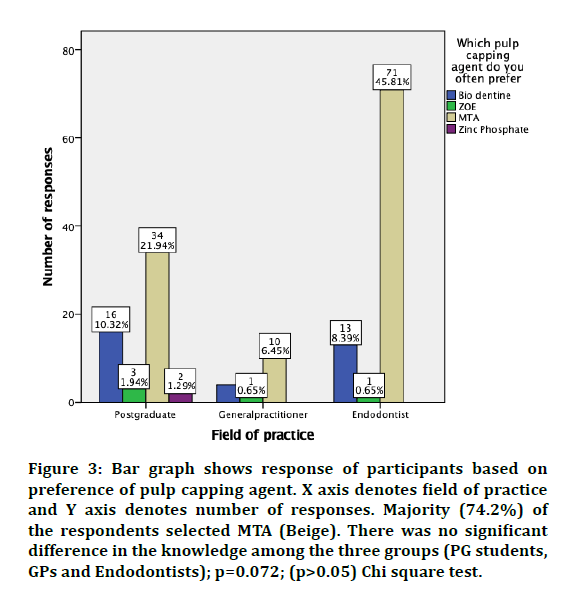
Figure 3: Bar graph shows response of participants based on preference of pulp capping agent. X axis denotes field of practice and Y axis denotes number of responses. Majority (74.2%) of the respondents selected MTA (Beige). There was no significant difference in the knowledge among the three groups (PG students, GPs and Endodontists); p=0.072; (p>0.05) Chi square test.
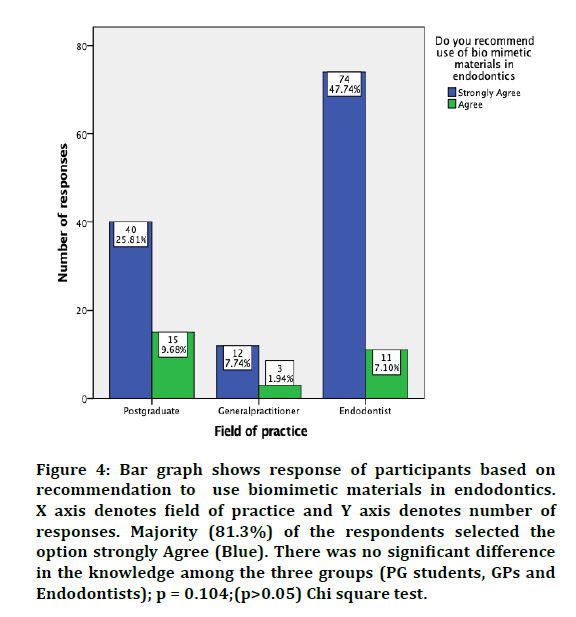
Figure 4: Bar graph shows response of participants based on recommendation to use biomimetic materials in endodontics. X axis denotes field of practice and Y axis denotes number of responses. Majority (81.3%) of the respondents selected the option strongly Agree (Blue). There was no significant difference in the knowledge among the three groups (PG students, GPs and Endodontists); p = 0.104;(p>0.05) Chi square test.
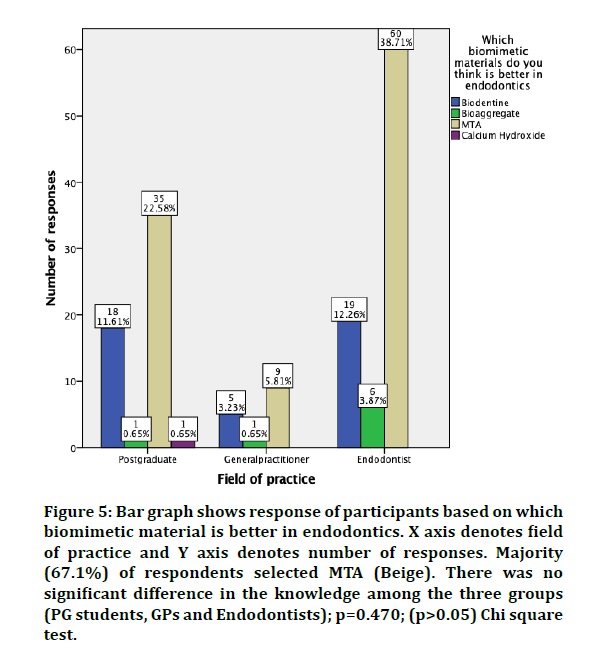
Figure 5: Bar graph shows response of participants based on which biomimetic material is better in endodontics. X axis denotes field of practice and Y axis denotes number of responses. Majority (67.1%) of respondents selected MTA (Beige). There was no significant difference in the knowledge among the three groups (PG students, GPs and Endodontists); p=0.470; (p>0.05) Chi square test.
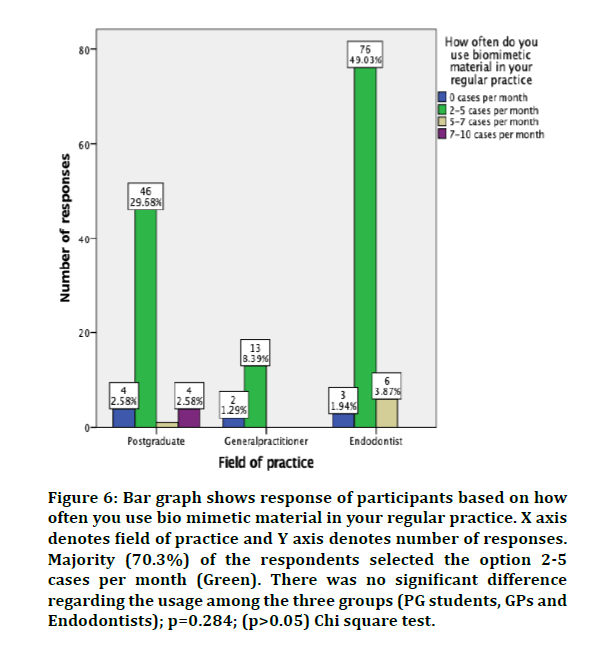
Figure 6: Bar graph shows response of participants based on how often you use bio mimetic material in your regular practice. X axis denotes field of practice and Y axis denotes number of responses. Majority (70.3%) of the respondents selected the option 2-5 cases per month (Green). There was no significant difference regarding the usage among the three groups (PG students, GPs and Endodontists); p=0.284; (p>0.05) Chi square test.
MTA has been considered as gold standard since its introduction in dentistry due to its excellent biological and physico-chemical properties. The application of biomimetic technology has demonstrated promising results in the field of dentistry [27,28]. These materials have gained increased acceptance due to their potential biocompatibility, biological and physicochemical properties with the living tissues, acting synergistically with body tissues, their repair role in eliminating body defects like bone loss etc. This survey will have the prime focus on knowledge, attitude and practice of biomimetic materials used in conservative dentistry &endodontics among dentists. Biomimetics term was coined by ottoschmitt in the 1950s [29]. Biomimetic is defined as the study of the structure and function of biological systems as models for the design and engineering of materials and machines [6]. Tooth restored with biomimetic material flexes in a similar manner as natural dentin. Such restorations are more cost-effective, aesthetic and long lasting with minimum to non-existent post-operative sensitivity than traditional restorations [6].
Scope biomimesis copies the principle of synthesizing materials under ambient conditions which reproduces mechanisms found in nature and thus addresses more than one issue. It is the properties of biomimetic materials that simulates physical and mechanical properties of the lost tissue, thus providing an opportunity to introduce and change treatment modalities for the disease. Biomimetic dentistry has potential for transforming everyday dental practice, it is an interdisciplinary approach. It brings the power of chemical, modern biological and physical science to solve real clinical problems. Biomimetic materials function as root canal sealer, filling materials, cements and root and crown repair material and possess features like strengthening the root following obturation, good sealing ability, enhanced biocompatibility, and antibacterial properties. Contemporary biomaterials can overcome the limitations of traditional materials. However, there exists limitations when categorizing them as ideal materials. Several invivo and invitro studies have demonstrated good results, however double blind, and randomized studies of sufficient duration with biomimetic materials needed to confirm long term success. The present study indicates that an exceedingly high percentage of the participants had a sound knowledge about biomimetic materials. Which means that such practices have gained a lot of recognition as compared to its status before a decade. All the participants are ready to use biomimetic materials in their regular practices, patient’s acceptance of such material would be the cost factor. Many participants have used biomimetic materials for their patients.
The knowledge of the participants about Biomimetic materials can be attributed to their curriculum during postgraduate training. It should also be incorporated during undergraduate training so that the awareness regarding such procedures increases among students. The present survey reported a highly positive attitude toward biomimetic materials. The unavailability and cost of required materials can also be a major cause for not practicing it.
Conclusion
The participants of this survey were generally optimistic about use of biomimetic materials, but they emphasized on special training for the same along with readily available materials. More of such surveys should be conducted to evaluate the response on a larger scale. Further, research coupled with professional training will have a far-reaching effect on success of biomimetic material and will thus benefit the patients.
References
- https://oxford.universitypressscholarship.com/view/10.1093/oso/9780199674923.001.0001/oso-9780199674923-chapter-10
- Murr LE. Biomimetics and biologically inspired materials. Handbook of materials structures, properties, processing and performance. 2014; 1–28.
- Rao PR, Ramachandra Rao P. Biomimetics. Sadhana 2003; 28:657–676.
- Tayebi L, Moharamzadeh K. Biomaterials for oral and dental tissue engineering. Woodhead Publishing 2017.
- Slavkin HC. Biomimetics: Replacing body parts is no longer science fiction. J Am Dent Assoc 1996; 127:1254–1257.
- Ali A, Saraf P, Patil J, et al. Biomimetic materials in dentistry. Research Reviews: J Material Sci 2017; 5:1-8.
- Govindaraju L, Neelakantan P, Gutmann JL. Effect of root canal irrigating solutions on the compressive strength of tricalcium silicate cements. Clin Oral Investigations 2017; 21:567–571.
- Azeem RA, Sureshbabu NM. Clinical performance of direct versus indirect composite restorations in posterior teeth: A systematic review. J Conservative Dent 2018; 21:2–9.
- Jenarthanan S, Subbarao C. Comparative evaluation of the efficacy of diclofenac sodium administered using different delivery routes in the management of endodontic pain: A randomized controlled clinical trial. J Conservative Dent 2018; 21:297–301.
- Manohar MP, Sharma S. A survey of the knowledge, attitude, and awareness about the principal choice of intracanal medicaments among the general dental practitioners and nonendodontic specialists. Indian J Dent Res 2018; 29:716–720.
- Nandakumar M, Nasim I. Comparative evaluation of grape seed and cranberry extracts in preventing enamel erosion: An optical emission spectrometric analysis. J Conservative Dent 2018; 21:516–520.
- Teja KV, Ramesh S, Priya V. Regulation of matrix metalloproteinase-3 gene expression in inflammation: A molecular study. J Conservative Dent 2018; 21:592–596.
- Janani K, Sandhya R. A survey on skills for cone beam computed tomography interpretation among endodontists for endodontic treatment procedure. Indian J Dent Res 2019; 30:834–838.
- Khandelwal A, Palanivelu A. Correlation between dental caries and salivary albumin in adult population in Chennai: An in vivo study. Brazilian Dent Sci 2019; 22:228–233.
- Malli Sureshbabu N, Selvarasu K, Nandakumar M, et al. Concentrated growth factors as an ingenious biomaterial in regeneration of bony defects after periapical surgery: A report of two cases. Case Reports Dent 2019; 7046203.
- Poorni S, Srinivasan MR, Nivedhitha MS. Probiotic strains in caries prevention: A systematic review. J Conservative Dent 2019; 22:123–128.
- Rajakeerthi R, Ms N. Natural product as the storage medium for an avulsed tooth–A systematic review. Cumhuriyet Dent J 2019; 22:249–256.
- Rajendran R, Kunjusankaran RN, Sandhya R, et al. Comparative evaluation of remineralizing potential of a paste containing bioactive glass and a topical cream containing casein phosphopeptide-Amorphous calcium phosphate: An in vitro study. Pesquisa Brasileira Odontopediatria Clin Integrada 2019; 19:1–10.
- Ramarao S, Sathyanarayanan U. CRA grid-A preliminary development and calibration of a paper-based objectivization of caries risk assessment in undergraduate dental education. J Conservative Dent 2019; 22:185–190.
- Siddique R, Nivedhitha MS. Effectiveness of rotary and reciprocating systems on microbial reduction: A systematic review. J Conservative Dent 2019; 22:114–122.
- Siddique R, Sureshbabu NM, Somasundaram J, et al. Qualitative and quantitative analysis of precipitate formation following interaction of chlorhexidine with sodium hypochlorite, neem, and tulsi. J Conservative Dent 2019; 22:40–47.
- Siddique R, Nivedhitha MS, Jacob B. Quantitative analysis for detection of toxic elements in various irrigants, their combination (precipitate), and para-chloroaniline: An inductively coupled plasma mass spectrometry study. J Conservative Dent 2019; 22:344–350.
- Bozeman TB, Lemon RR, Eleazer PD. Elemental analysis of crystal precipitate from gray and white MTA. J Endodont 2006; 32:425–428.
- Tay FR, Pashley DH, Rueggeberg FA, et al. Calcium phosphate phase transformation produced by the interaction of the portland cement component of white mineral trioxide aggregate with a phosphate-containing fluid. J Endodont 2007; 33:1347–1351.
- Reyes-Carmona JF, Felippe MS, Felippe WT. Biomineralization ability and interaction of mineral trioxide aggregate and white portland cement with dentin in a phosphate-containing fluid. J Endodont 2009; 35:731–736.
- Gandolfi MG, Taddei P, Tinti A, Prati C. Apatite-forming ability (bioactivity) of ProRoot MTA. Int Endodont J 2010; 43:917–929.
- Sarkar NK, Caicedo R, Ritwik P, et al. Physicochemical basis of the biologic properties of mineral trioxide aggregate. J Endodont 2005; 31:97–100.
- Wang Z. Bioceramic materials in endodontics. Endodontic Topics 2015; 32:3–30.
- Vincent JF, Bogatyreva OA, Bogatyrev NR, et al. Biomimetics: Its practice and theory. J Royal Society Interface 2006; 22:471–482.
Author Info
Krishnakanth Jaju and Iffat Nasim*
Department of Conservative Dentistry and Endodontics, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, IndiaCitation: Krishnakanth Jaju, Iffat Nasim, A Knowledge Attitude and Practice Survey on Biomimetic Materials Used in Conservative Dentistry and Endodontics Among Dentist, J Res Med Dent Sci, 2020, 8 (7): 220-226.
Received: 16-Sep-2020 Accepted: 22-Oct-2020 Published: 29-Oct-2020
