Research - (2021) Volume 9, Issue 5
A Comprehensive Study of Intestinal Obstruction
Naveen Kumar V and KS Ravi Shankar*
*Correspondence: KS Ravi Shankar, Department of General Surgery, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, India, Email:
Abstract
The commonest cause of intestinal obstruction in the adults in this study series was obstructed Hernia (42%) followed by postoperative adhesions (30%). Tenderness, guarding, rigidity, rebound tenderness and shock are the cardinal feature of strangulated obstruction. The second most common type of intestinal obstruction was due to postoperative adhesions. Salient features were pain. Postoperative adhesions constituted about 30% of the total cases studied. Volvulus of the sigmoid was 4% in this series, all the cases were undergone laparotomy due to failure in the recovery of symptoms. In all cases where there was vascular compromise, resection and anastomosis was done. Malignancy of the large bowel was seen in 7 cases constituting 14% of cases. 65% of the cases diagnosed as malignancy were in the age group 35 -75 years. Of these 2 cases were managed with Hartman’s procedure and remaining cases was managed with transverse loop colostomy Most of the deaths occurred in malignancy. Although pulmonary tuberculosis more prevalent in India due to advent use of antitubercular drugs incidence of abdominal tuberculosis is becoming less. In our study incidence of ileocaecal tuberculosis was 4% and both were managed with resection and anastomosis.
Keywords
Hernia, Laparotomy, Antitubercular drugs, Ileocaecal tuberculosis
Introduction
Bowel obstruction remains one of the most common intra-abdominal problems faced by general surgeons in their practice whether caused by hernia, neoplasm, adhesions or related to biochemical disturbances intestinal obstruction of either the small or large bowel continues to be a major cause of morbidity and mortality [1]. They account for 12% to 16% of surgical admissions for acute abdominal complaints. Manifestations of acute intestinal obstruction can range from a good appearance with only slight abdominal discomfort and distension to a state of hypovolemic or septic shock (or both) requiring an emergency operation.
To analyse the etiology, management, and outcome of patents with intestinal obstruction [2]. The death due to acute intestinal obstruction is decreasing with better understanding of pathophysiology, improvement in diagnostic techniques, fluid, and electrolyte correction, much potent anti-microbials and knowledge of intensive care. Most of the mortalities occur in elderly individuals who seek late treatment and associated pre-existing diseases like, diabetes mellitus, cardiac diseases, or respiratory disease. Early diagnosis of obstruction, proper technique during surgery and intensive postoperative treatment carries a grateful result.
Materials and Methods
Type of study: Prospective observational study.
Study Period: March 2017–September 2018.
Study Population: 50 patients.
Inclusion criteria
All patients diagnosed to have intestinal obstruction by clinical & radiological method and were intervened surgically irrespective of age group admitted in SBMCH were included in this study.
Exclusion criteria
Patients with intestinal obstruction who were not able to comply with the treatment. Patients who were not consenting for the study. During hospital stay if the patient is decided to put on conservative management were excluded, for the want of definitive intra op diagnosis.
Patients who were having subacute intestinal obstruction treated conservatively were excluded from the study, and only those cases of acute intestinal obstruction which were managed surgically were studied to establish the pathology of intestinal obstruction with an aim to know the mode of presentation, physical findings, radiological and hematological findings, operative findings, and outcome of acute intestinal obstruction.
After the admission of the patient, clinical data were recorded as per Proforma. The diagnosis mainly based on clinical examination and often supported by hematological and radiological examinations.
Results
The incidence of acute intestinal obstruction in all age group was studied from the cases admitted in Department of Surgery of Sree Balaji medical college and hospital during the period March 2017 to September 2018. The data regarding the symptoms and signs and laboratory investigations has been adopted in 50 cases during the study period.
During the period of 19 months, (studied 50 cases in 19 months) the total number of admissions in surgery were 14,236 cases. Of which 120 cases of acute intestinal obstruction were treated during these periods which comprise 0.95% of total number of admissions among these surgically treated cases, 50 cases were randomly selected for the present study. Total number of emergency surgeries done in the department of Surgery were 1,569 and acute intestinal obstruction in this group consisted of about 14.53% of these surgeries.
As per the below table and bar chart, the maximum incidence in the present study group is 51 -60 and 61-70 with 17 and 14 cases out of 50 cases (Table 1 and Figure 1). Male patients were more commonly affected when compared to female patients in the below table (Table 2 and Figure 2). Table 3 and Figure 3 represents socio-economic status.
| Age (years) | Male | Female | Total |
|---|---|---|---|
| 11 to 20 | Nil | Nil | Nil |
| 21 to 30 | 1 | 3 | 4 |
| 31 to 40 | 6 | 3 | 9 |
| 41 to 50 | 4 | 1 | 5 |
| 51 to 60 | 11 | 6 | 17 |
| 61 to 70 | 7 | 7 | 14 |
| 71 to 80 | 1 | 0 | 1 |
| Total | 30 | 20 | 50 |
Table 1: Age incidence.
| Sex | Number of cases | Percentage |
|---|---|---|
| Female | 20 | 40 |
| Male | 30 | 60 |
Table 2: Sex incidence.
| Socio-economic | Number of cases | Percentage |
|---|---|---|
| Poor | 38 | 76 |
| Middle | 12 | 24 |
| Upper | 0 | 0 |
| Total | 50 | 100 |
Table 3: Socio-economic status.
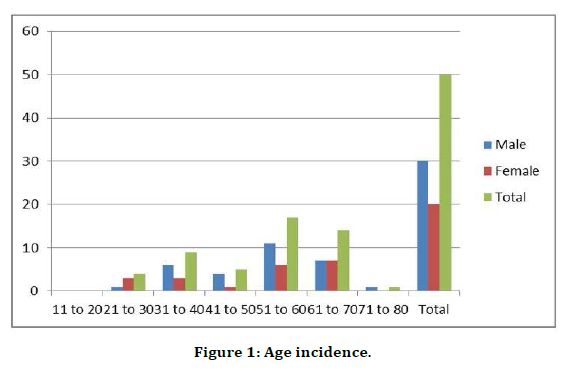
Figure 1. Age incidence.
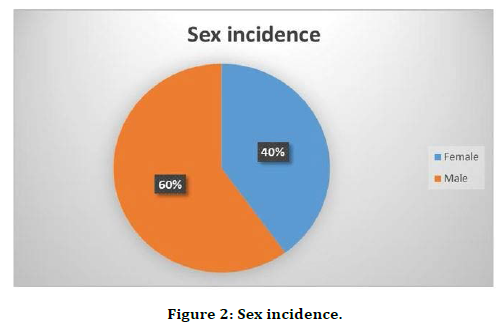
Figure 2. Sex incidence.
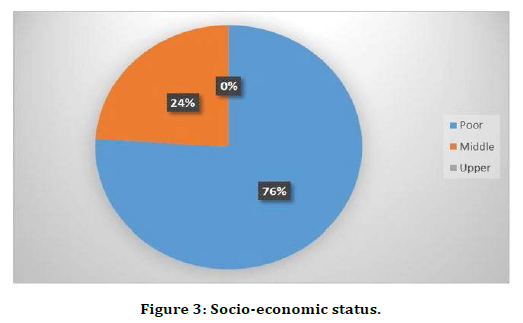
Figure 3. Socio-economic status.
In the present study of 50 cases, 32 patients were taking non-vegetarian which contains more of fatty diets. The remaining 18 patients were vegetarian which only contained high fiber diet (Table 4 and Figure 4).
| Diet | Number of Cases | Percentage |
|---|---|---|
| Veg | 18 | 36 |
| Non-veg | 32 | 64 |
| Total | 50 | 100 |
Table 4: Diet.
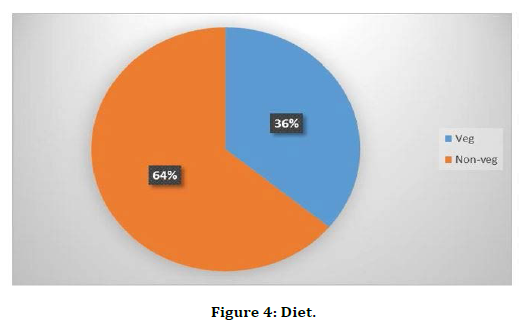
Figure 4. Diet.
The present study the most common symptoms were pain abdomen (88%) and vomiting (78%), and the most common signs were tachycardia (80%) and tenderness (28%) (Table 5 and Figure 5).
| Symptoms and signs | Number of cases | Percentage |
|---|---|---|
| Pain abdomen | 44 | 88 |
| Vomiting | 39 | 78 |
| Distension | 33 | 66 |
| Constipation | 27 | 54 |
| Tachycardia | 40 | 80 |
| Previous surgical scar | 22 | 44 |
| Tenderness | 14 | 28 |
| Rigidity | 13 | 26 |
| Mass | 12 | 24 |
| Visible peristalsis | 4 | 8 |
Table 5: Symptoms and signs.
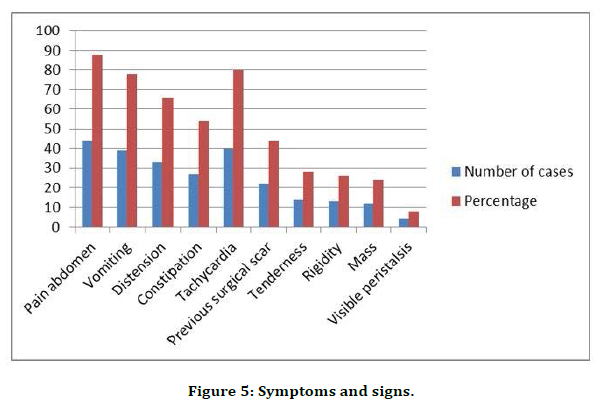
Figure 5. Symptoms and signs.
Incidence of Different Aetiology
The most common cause of intestinal obstruction in our study was Obstructed hernia. The next common was Postoperative Adhesions. Other conditions include malignancy, tuberculosis, intussusception, volvulus, mesenteric ischemia in descending frequency (Table 6 and Figure 6).
| Clinical condition | Number of cases | Percentage |
|---|---|---|
| Obstructed hernia | 21 | 42 |
| Postoperative Adhesions | 15 | 30 |
| Volvulus | 2 | 4 |
| TB abdomen | 2 | 4 |
| Malignancy | 7 | 14 |
| Intussusception | 2 | 4 |
| Mesenteric ischaemia | 1 | 2 |
| Total | 50 | 100 |
Table 6: Causes of intestinal obstruction in adults.
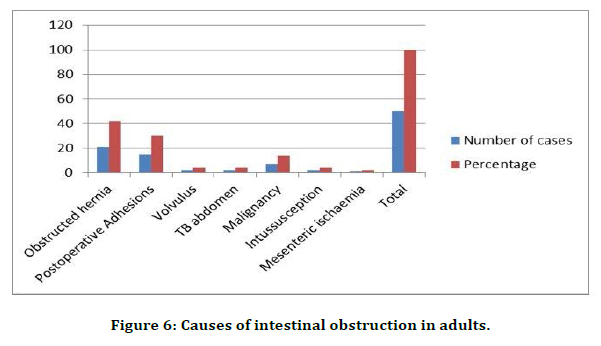
Figure 6. Causes of intestinal obstruction in adults.
In our study of 50 cases as accordingly with the etiology the management and the surgical procedure was done as shown in the table and pie diagram, release of adhesion with hernioplasty done in 32% of the cases, release of adhesions only done in 30% cases & resection anastomosis in 18% of cases (Table 7 and Figure 7).
| Management | Number of cases | Percentage |
|---|---|---|
| Release of adhesions & hernioplasty | 16 | 32 |
| Release of adhesions | 15 | 30 |
| Derotation of Volvulus & Sigmoidopexy | 2 | 4 |
| Resection & Anastomosis | 9 | 18 |
| Hartman’s procedure | 2 | 4 |
| Resection Anastomosis and Herniorrhaphy | 5 | 10 |
| Transverse Loop Colostomy | 1 | 2 |
| Total | 50 | 100 |
Table 7: Management.
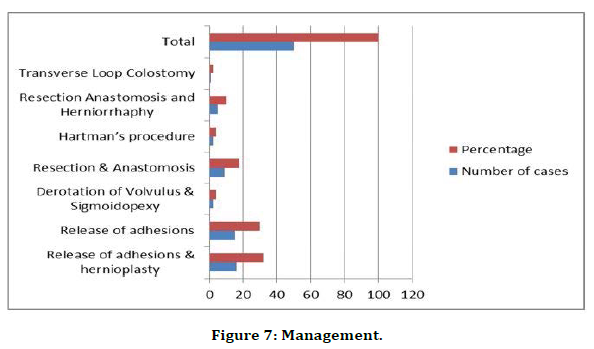
Figure 7. Management.
In the present study group there were 5 cases of septicemia, 2 cases of respiratory tract infection and 2 cases of wound infection (Table 8 and Figure 8).
| Postoperative complications | Number of cases |
|---|---|
| WI | 2 |
| RTI | 2 |
| Wound dehiscence | - |
| Faecal fistula | - |
| Septicaemia | 5 |
Table 8: Postoperative complications.
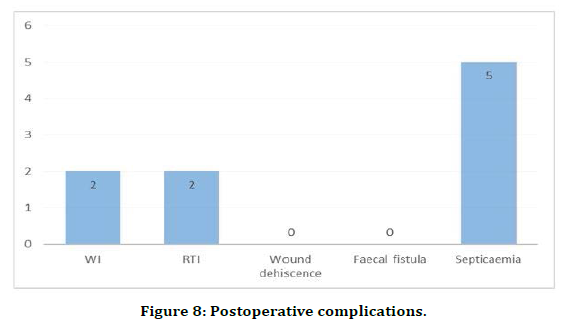
Figure 8. Postoperative complications.
In the present study of 50 cases, about 7 patients died with the percentage of 14%. Most deaths due to complications like septicemia, peritonitis, respiratory infection (Table 9 and Figure 9).
| Mortality | Number of cases | Percentage |
|---|---|---|
| Cured | 43 | 86 |
| Dead | 7 | 14 |
Table 9: Mortality.
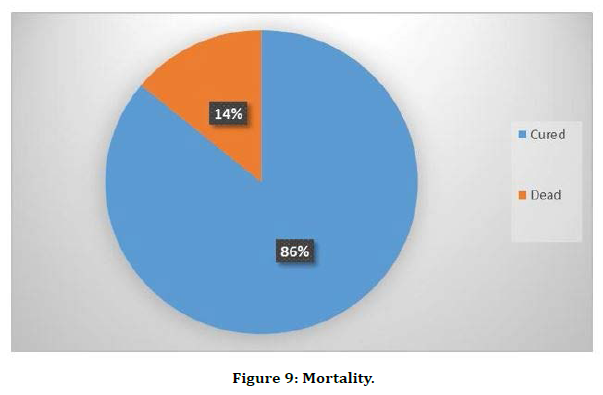
Figure 9. Mortality.
In the present study 7 persons died during postoperative period. The analysis of cause of death is shown below (Table 10). Table 11 explains the follow up status.
| Age and sex | Symptoms prior to admission | Operative Findings | Operative procedure | Cause of Death |
|---|---|---|---|---|
| 55/F (Case No. 8) | 3 days | Carcinoma sigmoid colon | Resection and anastamosis | Septicaemic Shock |
| 72/M (Case No.11) | 8 days | Carcinoma Rectum | Hartman’s Procedure | RTI |
| 65/M (Case No.21) | 5 days | Mesenteric Ischaemic | Resection anastamosis | Septicaemic Shock |
| 45/M (Case No.36) | 3 days | Carcinoma Caecum | Resection and anastamosis | RTI |
| 58/F (Case No. 37) | 5 days | Carcinoma ovary with sigmoid colon Infiltration | Transverse loop colostomy | Septicaemic Shock |
| 63/M (Case No.39) | 3 days | Carcinoma Rectum | Hartman’s Procedure | Septicaemia |
| 55/M (Case No.43) | 4 days | Carcinoma Colon | Resection and anastamosis | Septicaemia |
Table 10: Analysis of cause of death.
| Follow-up | Follow-up status | ||
|---|---|---|---|
| complications | One month | 3rd Month | 6th Month |
| A. Wound infection | 1 | Nil | Nil |
| B. Septicemia | Nil | Nil | Nil |
| C. Enterocutaneous Fistula | Nil | Nil | Nil |
| D. Prolonged ileus | Nil | Nil | Nil |
| E. Fever | 2 | 3 | Nil |
| F. Respiratory infection | 2 | 1 | Nil |
| G. Death | Nil | Nil | Nil |
| H. Recurrent obstruction | Nil | Nil | Nil |
Table 11: Follow-up status.
Discussion
Obstructed hernia continues to be the most common surgical emergency. A total of 120 patients presented with features of acute intestinal obstruction. Among these 50 cases of operated cases were randomly selected for the present study.
Disease incidence
In our clinical study incidence of acute intestinal obstruction is 0.95% of total surgical cases. In Souvik Adhikari et al. series incidence was 9.87% of total surgical cases. In Bhargava Anderson’s series incidence was 3% of total surgical cases. The commonest cause was found to be obstructed/ strangulated hernia, followed by post-operative adhesions, malignancy, intussusception, volvulus, tuberculosis and mesenteric ischaemia. In developing countries like India, the commonest cause used to be obstructed/strangulated hernia.
Previous studies reported an incidence of 9.87%, Bhargava and Anderson series reported an incidence of 3%. In our hospital 1569 cases of total emergency surgeries were done in March 2017 to September 2018, of which 120 cases of intestinal obstruction comprising of 0.95% incidence were present. Among these 50 cases were selected as random study group.
Clinical features
The clinical feature of intestinal obstruction pain abdomen, vomiting distension of abdomen and constipation are not present in all cases. Pain abdomen was present in 88% of the cases in the present study, whereas the vomiting was present in 78% of the cases. Whereas distension was present in 66% and constipation was present in 54% of the cases. The comparative table showing percentage of clinical features by various other study group are as follows.
In the present study, the clinical features of pain abdomen were 88%, vomiting was 78% which comparable with the other study group. Souvik Adhikari et al. and Jahangir Sarwar Khan et al. Only 66% of the patients in the present study group had distension of abdomen. It may be due to early approach to the hospital by patients in the present study.
The mass per abdomen on palpation is present in 24% of the total study, present mostly in Malignancy and ileocaecal tuberculosis. Visible peristalsis is present in 8% of the intestinal obstruction cases. The rectal examination did not reveal any abnormality except in 2 cases of intussusception (4%) and 7 cases of malignancy (14%) where in red currant Jelly stools and rectal growth were th e per rectal findings respectively.
Laboratory investigation
Among the total study population 30% of the cases were having Anaemia otherwise the basic haematological investigation did not yield much statistical significance.
Radiology
The Erect abdomen X-ray helps us in the diagnosis of intestinal obstruction as well as in differentiating the small bowel with large bowel obstruction. Multiple air fluid level can be seen in small multiple intestinal obstruction whereas only gas shadows seen in large bowel observation until the ileocaecal value is competent. Taneja et al. report shows 90% of cases with multiple air fluid level and Savage et al. reports 95% cases with significant findings. In the present study of the 50 cases 60% of X-ray shows multiple air blood levels. Contrast study of barium enema may help to locate the obstruction in the colon but in our study contrast study was not done.
Surgical management
The surgical management for the present study group includes resection anastomosis and herniorrhaphy for many of the cases of obstructed/strangulated hernia where the viability of the bowel was doubtful and also for ischemic bowel which is around 10%, release of constricting agents and hernioplasty was done in 32% of the obstructed/strangulated hernia cases, release of adhesions for postoperative adhesions was done in 30% cases. Two cases were managed with Hartman’s procedure and one case with transverse loop colostomy.
Complications
In the present study group out of 50 cases, complications like septicemia 5 cases, respiratory tract infection 2 cases, wound infection in two cases occurred. The complication of septicemia was more in the cases of malignancy and one case of mesenteric ischemia case where in there was already sepsis at the time of admission, and for these cases bowel surgeries were done which were unprepared. Two cases one with obstructed inguinal hernia and one with the case of carcinoma rectum, the patients had prior comorbid conditions of COPD were suffered from respiratory tract infection.
Mortality
Frequency of mortality in our study is 14% i.e. 7 cases out of 50 cases. Among these 6 cases were due to malignancy and one due to mesenteric ischaemia. The mortality rate in the present study is much comparable to Ramachandran CS et al. study but it is more when compared to previous studies.
Out of 7 cases died, 6 cases were due to malignancy. As the malignancy was more in the aged group and the unprepared bowel surgeries done to the patient led to septicemic condition and resulted in death. Two patients were chronic smoker who suffered respiratory tract infection and died. Hence most of the deaths were due to malignancy which played significant role in the outcome of the disease. The mortality in intestinal obstruction is more in patients who develop strangulation and gangrene of the bowel, also who reached the hospital after 3 days. With all these, the age of the patient, general condition of the patient, duration of symptoms. Operative procedures carry a high role in progress [3-39].
Conclusion
Acute intestinal obstruction remains an important surgical emergency in the surgical field. Success in the treatment of acute intestinal obstruction depends largely upon early diagnosis, skillful management and treating the pathological effects of the obstruction just as much as the cause itself. Erect abdomen X-ray is valuable investigation in the diagnosis of acute intestinal obstruction.
Obstructed hernias are the common cause to produce intestinal obstruction. Clinical radiological and operative findings put together can diagnose the intestinal obstruction. Etiology – P value- 0.001(<0.05), hence the percentage of people with obstructed hernia, post op adhesions, volvulus, TB abdomen and intussusception have higher cure rates when diagnosed early, when compared with malignancy and mesenteric ischemia which has lower cure rates, and the difference is statistically significant. There is no statistically significant difference between cure rates and death rates due to various surgeries, probably because our sample size was small. P value 2.0(>0.05). Mortality is still significantly high in acute intestinal obstruction if the time of presentation to hospital is late, old age and if the diagnosis and intervention is delayed.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgments
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Houghton SG, Medina ARD, Sarr MG. Bowel obstruction. 11th Edn. In: Maingot’s Abdominal operations, Zinner MJ, Ashley SW, eds. New York: McGraw- Hill Medical 2007; 479 -505.
- Markogiannakis H, Messaris E, Dardamanis D, et al. Acute mechanical bowel obstruction: Clinical presentation, etiology, management and outcome. World J Gastroenterol 2007; 13:432.
- Wangensteen OH. Historical aspect of the management of the acute intestinal obstruction. Surgery 1969; 63:363-383.
- Die KH. Roentgen diagnose des ileus ohne koutrastmittel. Arch F Klin Chir 1919; 112:513.
- Akgun Y. Mesosigmoidop1asty as a definitive operation in treatment of acute sigmoid volvulus. Dis Colon Rectum 1990; 39:579-581.
- Decker GAG, du Plessis DJ. The duodenum, jejunum and ileum. 12th Edn. Chapter 4. In: Lee McGregor’s Synopsis of surgical anatomy. Bombay: Wright Verghese; 1986; 30.
- Drake RL, Wayne Vogl A, Mitchell AWM. Abdomen. 2nd Edn. Chapter 4. In: Gray’s Anatomy for students. Philadelphia: Churchill Livingstone Elsevier 2010; 300.
- Ganong WF. Regulation of gastrointestinal function. 19th Edn. Chapter 26. In: Review of medical physiology. Philadelphia, USA: Appleton and Lance 1999; 483.
- Berne RM. Gastrointestinal regulation and motility. 5th Edn. Chapter In: Physiology, Berne RM, Levy MN, Koeppen BM, et al. Mosby Publication 2008; 539.
- Deitch EA, Bridges WM, Ma JW, et al. Obstructed intestine as a reservoir for systemic infection. Am J Surg 1990; 159:394-401.
- Williams NS, Bulstrode CJK, O’Connell RP. Intestinal obstruction. 25th Edn. Chapter 66. In: Bailey and Love’s Short practice of surgery. London: Hodder Arnold; 2008; 1188 -203.
- El-Amin LC, Levine MS, Rubesin SE, et al. Ileocal valve: Spectrum of normal findings at double-contrast barium enema examination. Radiology 2003; 227:52-58.
- Kim SY, Morris JB. Small bowel obstruction. 6th Edn. Chapter 68. In: Shackel Ford’s Surgery of the alimentary tract, Charles J Yeo, ed. Philadelphia: Saunders Elsevier 2007; 1025-1033.
- Browse NL. The abdomen. 4th Edn. Chapter 15. In: Brown’s Introduction to the symptoms and signs of surgical disease. USA: Book Power; 2005; 413.
- Maglinte DD, Heitkamp DE, Howard TJ. Current concepts in imaging of small bowel obstruction. Radiol Clin N Am 2003; 41:263.
- Ali Tavakkolizadeh, Edward E Whang, Stanley W Ashley, et al. Small intestine. 9th Edn. Chapter 28. In: Schwartz’s Principles of surgery, Charles F Brunicardi, Dana K Anderson, Timothy R Billiar, et al. New York: McGraw-Hill Publication; 2010; 980-1011.
- Hayanga AJ, Bass-Wilkins K, Bulkley GB. Current management of small bowel obstruction. Adv Surg 2005; 39:1-33.
- Pickleman JR, Fischer JE. Small and large bowel obstruction. 5th Edn. Chapter 122. In: Mastery of surgery, Boston: Lipincott Williams & Wilkins; 2009; 1380-1387.
- Wilson MS, Ellis E, Menzies D, et al. A review of the management of small bowel obstruction. Ann R Coll Surg Engl 1999; 81:320-8.
- Menzies D, Parker M, Hoare R, et al. Small bowel obstruction due to postoperative adhesions: treatment patterns and associated costs in 110 hospital admissions. Ann R Coll Surg Engl 2001; 83:40-46.
- Kostner FL, Hool GR, Lavery IC. Management of causes of acute large bowel obstruction. Surg Clin N Am 1997; 60-77.
- Krishnan A, Vikram Kate. Adhesive intestinal obstruction. Current perspectives. Chapter 8. In: Recent advances in surgery, Roshan Lal Gupta, ed. New Delhi: Jaypee Brothers 2002; 225-241.
- Ellis Harold DM. The cause and prevention of postoperative pain intraperitoneal adhesions. Surg Gynecol Obstet 1971; 133:497-511.
- Ellis H, Moran BJ, Thompson JN, et al. Adhesion - related hospital readmissions after abdominal and pelvic surgery: A retrospective cohort study. Lancet 1999; 353:1476-1480.
- John E Skandalakis. Small intestine. 2nd Edn. Chapter 10. In: Surgical anatomy and technique. Atlanta: Springer 2004; 430.
- Chang CC, Chen YY, Chen YF, et al. Acute intussusception in Asians; clinical presentation, diagnosis and treatment. J Gastroenterol Hepatol 1997; 22:1767-1771.
- Agaoglu N, Yucel Y, Turkytlmaz S. Surgical treatment of the sigmoid volvulus. Acta Chir Belg 2005; 105:365-368.
- Larkin JO, Thekiso TB, Waldron R, et al. Recurrent sigmoid volvulus early-resection may obviate later emergency surgery and reduce morbidity and mortality. Ann R Coll Surg Engl 2009; 91:205-209.
- Williamson RCN, Jiao LR. Small bowel. 5th Edn. Chapter 14. In: General surgical operations, Kirk RM, ed. England: Churchill Livingstone Elsevier 2006; 209-227.
- Soybel DI. Ileus and small bowel obstruction. 3rd Edn. Chapter 26. In Scientific principles and practice of surgery. Philadelphia: Lipincott Williams & Wilkins 2003; 810.
- Suggs WJ, Young-Fadok TM. Pseudo-obstruction of the colon. 1st ed. In: The practice of general surgery. Philadelphia, PA: Saunders; 2002; 499-502.
- Adhikari S, Hossein MZ, Das A, et al. Etiology and outcome of acute intestinal obstruction: A review of 367 patients in Eastern India. The Saudi J Gastroenterol 2010; 16:285-287.
- Khan JS, Alam J, Hassan H, et al. Pattern of intestinal obstruction a hospital based study. Pakistan Armed Forces Med J 2007.
- Cole GJ. A review of 436 cases of intestinal obstruction in Ibadan. Gut 1965; 6:151.
- Singh H. Acute intestinal obstruction. Arch Surg 1965; 91:389-392.
- Brooks VLH, Butler A. Acute intestinal obstruction in Jamaica. Surg Gynaec Obstet 1996; 122:261-264.
- Playforth RH. Mechanical small bowel obstruction and plea for the earlier surgical intervention. Ann Surg 1970; 171:783-788.
- Sharkeed S. Intestinal obstruction. Am J Surg 1975; 130.
- Ramachandran CS. Acute intestinal obstruction: 15 years’ experience. IJS 1982; 672-679.
Author Info
Naveen Kumar V and KS Ravi Shankar*
Department of General Surgery, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Naveen Kumar V, KS Ravi Shankar, A Comprehensive Study of Intestinal Obstruction, J Res Med Dent Sci, 2021, 9 (5):318-326.
Received: 25-Mar-2021 Accepted: 26-May-2021
