Research - (2021) Volume 9, Issue 6
A Comparative Study of Typhidot and Diazo Test in Early Detection and Diagnosis of Typhoid Fever in Children
S Sundari*, M Shafath Ahmed and Pooja Pradeep
*Correspondence: S Sundari, Department of Paediatrics, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, India, Email:
Abstract
The present study was to compare the sensitivity and specificity of Typhidot and Diazo test with blood culture as gold standard for diagnosis of Typhoid fever in children. This was a cross- sectional comparative study done on 100 children clinically suspected to have Typhoid fever at Sree Balaji Medical College and Hospital, Chennai. Blood sample was collected for Typhidot and blood culture and Urine sample was collected for Diazo test. The data collected was analysed using suitable statistical tests. It has been observed from the study that 26 children had positive blood culture. The sensitivity, specificity, positive predictive value and negative predictive value for Typhidot assay was 88.46%, 86.49%, 69.7% and 95.5% respectively. The sensitivity, specificity, positive predictive value and negative predictive value for Diazo test was 73.08%, 79.73%, 55.8% and 89.4% respectively .The present study includes Typhidot assay has higher sensitivity and specificity compared to Diazo test in diagnosis of Typhoid fever in children. Although Typhidot is superior to Diazo test, the present study shows a reasonable value of sensitivity and specificity for Diazo test. Hence it can be used in resource poor settings as it is economic and easy to perform.
Keywords
Typhidot, Diazo test, Culture, Sensitivity, Leptospirosis, IgM, Paediatrics
Introduction
Typhoid fever is an endemic disease and is a major public health problem in developing countries where water supply and sanitation are substandard [1]. Global estimate of Typhoid fever is 21 million cases annually, resulting in an estimated 216,000 - 600,000 deaths per year predominantly in children of school age or younger, the majority of which is in Asia [2].
It is one of the most common infectious diseases prevalent in India. In the year 2014 the reported data shows 1.7 million cases and 429 deaths. Maximum cases were reported from Bihar (273,0007 cases with 4 deaths). In south India large number of cases was reported from Andhra Pradesh (186,446 cases and 5 deaths) [2].
Children are disproportionately affected by Typhoid fever, with peak incidence between 5 to 15 years of age.1.It is a life-threatening systemic infection caused by salmonella typhi usually transmitted through feacooral route. Similar but often less severe disease, paratyphoid fever is caused by Paratyphi A, BorC [1].
Early and prompt diagnosis of Typhoid is mandatory among children. With increasing use of antibiotics, clinical presentation is nonspecific and difficult to diagnose clinically. Since the clinical scenarios of common infections like Malaria, Typhoid, Leptospirosis and Scrub are very similar, it is very difficult for treating physician to recognise Typhoid fever on the basis of clinical features. Hence it is mandatory to have a very valid diagnostic test with good sensitivity and specificity for an early detection of enteric fever in children [3].
Confirmation of diagnosis is by isolating the organism from blood, bone marrow, stool or urine. There are no hundred percent sensitive or ideal tests available for Typhoid fever [1]. Although blood culture is the gold standard investigation, it is cumbersome and require elaborate laboratory equipment. Sensitivity is also affected by the amount of blood obtained for culture. It is further reduced with the starting of antimicrobial therapy prior to confirmation of the diagnosis.4Bone marrow culture is more sensitive but it an invasive procedure. Stool cultures are generally positive only after second week of illness and only in 30% of patients [4]. Molecular studies like polymerase chain reaction have high accuracy for diagnosis, but owing to its high cost it remains impractical in many areas where Typhoid fever is endemic [5].
Although Widal test is routinely done as rapid serological screening for Typhoid fever, it has only moderate sensitivity and specificity and hence has limited diagnostic value [6]. Recent advances in immunology have led to discovery of rapid, reliable, easy to perform serological test with higher sensitivity and specificity. Typhidot is one such serological test available for rapid diagnosis [6].
A simple bedside test like Diazo which has served in epidemic situations in the past should also be reevaluated for patients in rural or remote health settings. Diazo test becomes positive from day 5 of fever and remain positive till day 31 of fever. Average duration of test positivity was 6 to 16 days of fever [7-19]. The present study was undertaken to compare the sensitivity and specificity of Typhidot test and Diazo test in suspected Typhoid cases in our tertiary health care centre in Chennai.
Materials and Methods
Study design
Cross-sectional comparative study.
Study place
Department of Paediatrics, Sree Balaji Medical College and Hospital, Chrompet, Chennai.
Study period
April 1st 2018 to April 1st 2019.
Study population
100 children.
Inclusion criteria
• Children up to the age of 15 years.
• Children with history of fever more than 3 days with clinical symptoms and signs suggestive of Typhoid fever.
Exclusion criteria
Fever patients with alternative diagnosis were excluded from study.
Study method
All the children up to 15 years of age having history of fever more than 3 days with symptoms and signs suggestive of Typhoid fever and attended Department of Paediatrics in Sree Balaji Medical College and Hospital was selected for study. The study was conducted after obtaining the ethical clearance from the ethical committee of the institution. Parents or guardian were informed about the study and consent was taken. The details of clinical symptoms and examination of the patient was done to look for the presence of positive signs and was recorded in the proforma and following investigations were done on the day of admission.
Blood collection
Around 4 ml of blood were collected with aseptic precaution from the children clinically suspected to have Typhoid fever. Around 1-2 ml of blood was used for blood culture. The remaining blood was used for complete blood count and Typhidot test.
Blood culture
1-2 ml of blood was taken under aseptic precaution and inoculated into paediatric blood culture bottle BACT/ ALERT®PF (BIOMERIEUX, USA) and sent to the microbiology department of Sree Balaji Medical College and Hospital. Samples were incubated in the automated BacT/ALERT 3D system (BIOMERIEUX, USA) for 72 hours. According to manufacturer’s instructions, any sample that did not generate any signal within 72 hours of incubation was interpreted as no growth (negative).
The preliminary signal of bacterial growth in BacT/ ALERT bottle was detected and displayed on the 3D monitor of BacT/ALERT system mentioning the detection time. The bottle showing positive signal were subcultured on nutrient agar, blood agar, MacConkey agar and incubated overnight at 37°C. The non-lactose fermenting smooth colonies detected on the plate were picked up for further biochemical, serological and antibiotic sensitivity tests.
Typhidot IgM test
It is a rapid, qualitative, sandwich immunoassay for the detection of IgM antibodies to S. typhi in human serum/ plasma or whole blood specimen.
It qualitatively detects the presence of IgM class of Lipopolysaccharide (LPS) specific to S. typhi in human serum/plasma or whole blood specimens.
Typhidot testing was done on an acute serum by using Typhidot M kit (Enterocheck-WB).
Principle
It utilizes the principle of agglutination of antibodies/ antisera with respective antigen in immuno chromatography format along with use of nano gold particles as agglutination revealing agent. The conjugate pad contains two components-Agglutinating sera for human IgM conjugated to colloidal gold and rabbit globulin conjugated to colloidal gold. As the test specimen flows through the membrane test assembly, the Agglutinating sera for human IgM -colloidal gold conjugate complexes with the S. typhi specific IgM antibodies in the specimen and travels on the membrane due to capillary action. This complex moves further on the membrane to the test region (T) where it is immobilized by the S. typhi specific LPS antigen coated on the membrane leading to formation of a pink to pinkpurple coloured band. The absence of this coloured band in the test region indicates a negative test result.
The unreacted conjugate and unbound complex, if any along with the rabbit globulin - colloidal gold conjugate move further on the membrane and are subsequently immobilized by the Agglutinating sera for rabbit globulin coated on the membrane at the control region (C), forming a pink to pink-purple coloured band. This control band acts as a procedural control and serves to validate the results.
Procedure
• Dispense 5 μL of serum into specimen port A using a micro pipette.
• Add five drops of sample running buffer into buffer port B.
• Read result within five to fifteen minutes (Table 1).
Table 1: Interpretation of Typhidot M assay.
|
Negative Result: If IgM antibodies to S.typhi are not present, only one coloured band appears in the Control Window (C). |
|
Positive Result: If IgM antibodies to S.typhi are present, two coloured bands appear in the Test (T) and Control Window (C). The intensity of the test band may be more or less than the Control band, depending upon the concentration of IgM antibodies in specimen. |
|
Invalid Result: The test is invalid if no band is visible at fifteen minutes. The test should also be considered invalid if only test band appears and no control band appears. Verify the test procedure and repeat the test with a new device. |
Urine collection
Diazo test
Diazo reagent is prepared from two stock solutions 'A' and 'B', the constituents of which are as follows: (i) Stock solution 'A': Sulphanilic acid-0.5 g, Cone HC1-5 ml, Distilled water-100 ml; and (ii) Stock solution 'B': Sodium nitrite-0.5 g, Distilled water-100 ml. Forty parts of stock solution 'A' is mixed with 1 part of stock solution 'B'. 2 ml of this mixture and 2 ml of early morning urine sample are mixed. To those 5 drops of 30% ammonium hydroxide is added. The sample is shaken well. A positive reaction is indicated by a red or pinkish coloration of the froth (Figure 1).
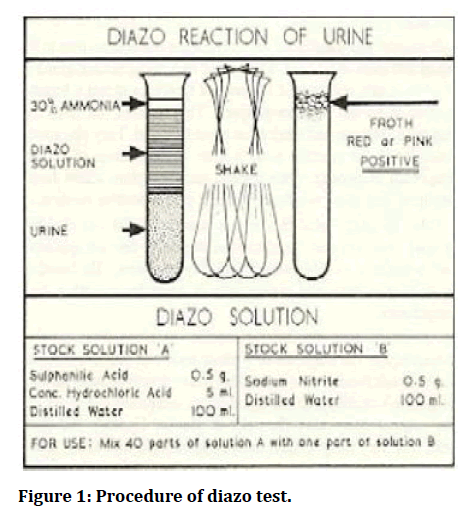
Figure 1: Procedure of diazo test.
Statistical analysis
All the statistical analysis was performed using SPSS statistical software (Version 24). Chi-square test was used to observe statistical difference among the observed value and experimental value of variables. All the difference would be considered statistically significant at pvalue<0.05. Sensitivity, specificity, positive predictive value, negative predictive value, positive and negative likelihood ratios were calculated for typhidot test and diazo test by comparing the results with the gold standard blood culture.
Ethics
Written informed consent was obtained from the parents and institution review board clearance was obtained.
Results
Of the selected cases 38% of the cases belong to the age group of 0-5 years, 50% of the cases belong to the age group of 6-10 years and 12% of the cases belong to the age group of 11-15 years. The youngest patient was 1 year old and the oldest patient was 13 years. The mean age was 6.63 ± 2.92 years (Table 2 and Figure 2). Of the study group 51% of selected cases were male and 49% of the selected cases were female. The male to female ratio is 1:0.96 (Table 3 and Figure 3).
Table 2: Age distribution.
| Age group (Years) | Number of patients | Percentage (%) |
|---|---|---|
| 0-5 | 38 | 38% |
| 6-10 | 50 | 50% |
| 11-15 | 12 | 12% |
| Total | 100 | 100% |
Table 3: Sex distribution.
| Sex | Number of patients | Percentage (%) |
|---|---|---|
| le | 51 | 51% |
| Female | 49 | 49% |
| Total | 100 | 100% |
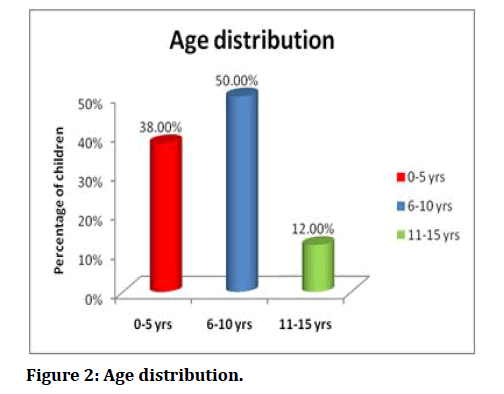
Figure 2: Age distribution.
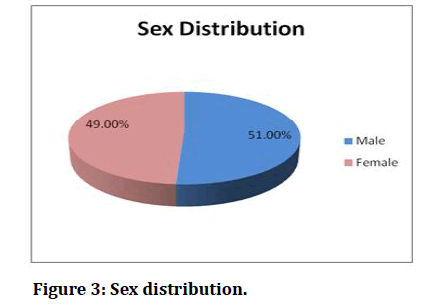
Figure 3: Sex distribution.
Among participants, 46% (46) belonged to lower class and 31% (31) belonged to lower middle class. While 12% (12) and 11% (11) belonged to middle class and upper middle class, respectively. None of the participants in this study belonged to upper class (Table 4 and Figure 4).
Table 4: Socioeconomic status.
| Socioeconomic status | Frequency | Percentage (%) |
|---|---|---|
| Lower | 46 | 46% |
| Lower middle | 31 | 31% |
| Middle | 12 | 12% |
| Upper middle | 11 | 11% |
| Upper class | 0 | 0% |
| Total | 100 | 100% |
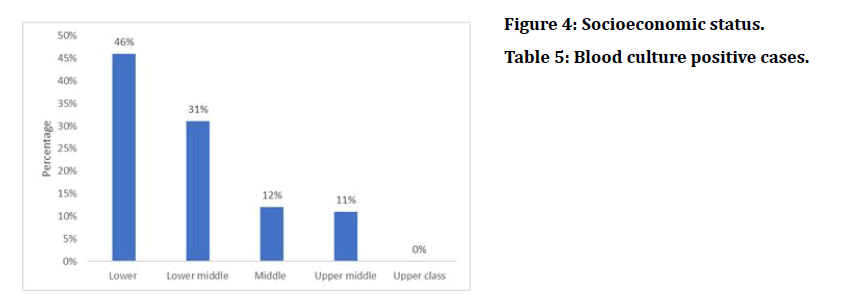
Figure 4: Socioeconomic status.
Out of 100 children, 26 children had S. typhi grown in blood culture method. They are culture positive and confirmed cases of typhoid fever since blood culture method is considered as yardstick for diagnosing typhoid fever (Table 5 and Figure 5).
Table 5: Blood culture positive cases.
| Blood culture positivity | |||
|---|---|---|---|
| Sl. No. | Valid | Frequency | Percentage (%) |
| 1 | Positive | 26 | 26% |
| 2 | Negative | 74 | 74% |
| 3 | Total | 100 | 100% |
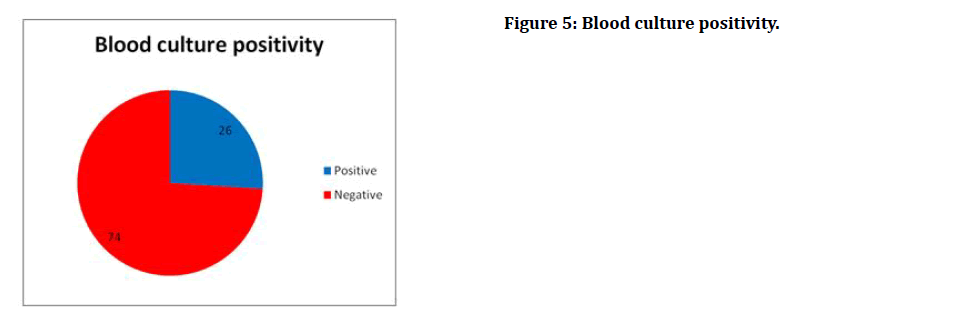
Figure 5: Blood culture positivity.
It has been observed from the study that out of all the positive cases, 34.6% of the patients had a temperature between 99-100oF, 46.2% had between 101-102oF, 15.4% had between 103-104oF and 3.8% had a temperature >104oF during the time of admission (Table 6 and Figure 6).
Table 6: Temperature at admission of blood culture positive cases.
| Temperature | Number | Percentage |
|---|---|---|
| 99-100oF | 9 | 34.60% |
| 101-102oF | 12 | 46.20% |
| 103-104oF | 4 | 15.40% |
| >104oF | 1 | 3.80% |
| Total | 26 | 100% |
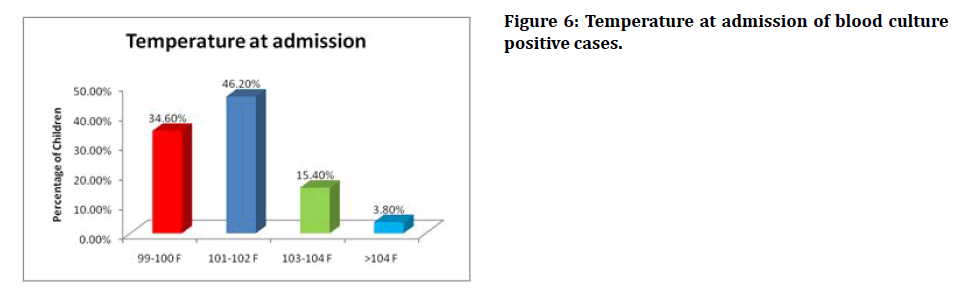
Figure 6: Temperature at admission of blood culture positive cases.
Out of blood culture positive confirmed cases of typhoid, 57.7% of the cases had symptoms of vomiting while 42.3% of the cases did not have any symptom of vomiting (Table 7 and Figure 7).
Table 7: Vomiting among blood culture positive cases.
| Vomiting | |||
|---|---|---|---|
| Sl. No. | Valid | Frequency | Percentage (%) |
| 1 | Present | 15 | 57.70% |
| 2 | Absent | 11 | 42.30% |
| 3 | Total | 26 | 100% |
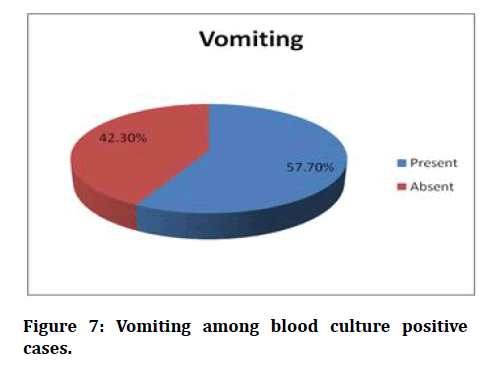
Figure 7: Vomiting among blood culture positive cases.
Discussion
Though typhoid fever is a common infection in children, it is difficult to diagnose because of its nonspecific symptoms and signs. However it is necessary to diagnose early to initiate appropriate antibiotic therapy because delay in starting antibiotic treatment may lead to several morbidities and even death. The gold standard for diagnosing typhoid fever has always been the blood culture method but it is time consuming, requires elaborate laboratory equipment and a level of technical expertise which may not be present in resource poor laboratories.
This delay may result in complications of typhoid fever. The study was primarily carried out to compare the Typhidot assay with age old Diazo test while taking blood culture as gold standard method. The results and observation of the present study comprising of 100 children has been discussed and compared with previously reported studies.
Age group
It has been observed from the study that the mean age of the patients under consideration was 6.63 years. Majority of the patients (50%) were in the age group of 6-10 years which is similar to the study where most common age group was 5-10 years.
Sex
It has been observed from the study that the male to female ratio in the study subjects were found to be 1:0.96 which is comparable with that of Mackie et al. [20] which had a male to female ratio of 1:1 and also comparable to the study where male to female ratio was 1:1 [21].
Socioeconomic status
It our study majority of children (46%) belonged to lower class. This is in conjunction to the observation made by Ram et al. [22] where majority of cases came from lower socio economic classes with poor personal hygiene.
Symptom and signs analysis
The presenting symptoms of the 26 blood culture positive, confirmed cases of typhoid fever is as follows (Table 8).
Table 8: Symptoms and signs analysis.
| Sl. No. | Symptom | Frequency | Percentage |
|---|---|---|---|
| 1 | Fever | 26 | 100% |
| 2 | Nausea | 17 | 65.40% |
| 3 | Vomiting | 15 | 57.70% |
| 4 | Abdominal pain | 15 | 57.70% |
| 5 | Constipation | 1 | 3.80% |
| 6 | Diarrhoea | 5 | 19.20% |
| 7 | Coated Tongue | 20 | 76.90% |
| 8 | Hepatomegaly | 18 | 69.20% |
| 9 | Splenomegaly | 10 | 38.50% |
From the above table we find the most frequent symptoms were fever associated with nausea, vomiting and abdominal pain which was present in more than half of the study population which is similar to the study conducted by Ram [22] in which the most common symptom was fever(100%) followed by anorexia(61%), vomiting(44%) and abdominal pain(18%).
The most commonly observed clinical signs in this study Coated tongue followed by hepatomegaly which is similar to the study conducted by Ram et al. [22] in which common sign observed was coated tongue followed by hepatomegaly.
Blood culture isolates in comparison to previous studies
In our study, 26% of the cases were positive by blood culture which is more or less comparable to the observations made by Kumar et al. [23] and Surendranath et al. [24] who has reported 24% positivity and 28.5% positivity respectively for blood culture.
Comparatively lower sensitivity of blood culture maybe because of ridiculous use of antimicrobial agents and also difficulty in drawing required quantity of blood for cultures in children.
Positivity of Typhidot in comparison to previous studies
It has been observed in the current study that 33% of the cases was positive by Typhidot M test which is found to be consistent with 32.4% reported by Mehmood et al.15 and 50.4% reported by Udayakumar et al.11 (Table 9).
Table 9: Positivity of Typhidot in comparison to previous studies.
| Author Name (year) | Positive percentage |
|---|---|
| Jesudason M et al (2002)23 | 9% |
| Narayanappa et al (2010)24 | 74.30% |
| Mehmood et al. (2015)25 | 32.40% |
| Udayakumar et al. (2017)21 | 50.40% |
| Present study | 33% |
It has been observed in the present study that 34% of the cases have been found to be positive for diazo which is found to be between the values observed by Koneman et al. [18] and Ananthanarayanan et al. [16].
Sensitivity and specificity of Typhidot test in comparison to previous studies
In the present study the sensitivity of the Typhidot was observed to be 88.46% which was found to be comparable to other previous studies. So Typhidot fulfils one of the standards for an ideal diagnostic test as it does not usually miss the diagnosis when compared to Blood Culture.
Conclusion
Symptoms of the typhoid fever in children are nonspecific, however presence of vomiting, abdominal pain, cough, anorexia and diarrhoea in febrile child with history of fever more than 3 days should prompt the paediatrician to consider the possibility of typhoid fever. Likewise, presence of toxic look, coated tongue, abdominal tenderness, hepatomegaly and splenomegaly in a febrile child are suggestive of typhoid fever. Typhidot assay is a rapid, easy to perform and a reliable diagnostic test and can be used in early institution of therapy where the facilities for culturing the blood is not available to diagnose typhoid fever. However, it has limitations due to high cost.In the present study we have compared the specificity and sensitivity of Typhidot test and Diazo test with the blood culture in the diagnosis of typhoid fever. Typhidot shows a sensitivity and specificity of 88.46% and 86.49% respectively, whereas Diazo test showed sensitivity and specificity of 73.08% and 79.73% respectively, in culture proven cases. Hence the sensitivity and specificity of Typhidot is more compared to Diazo test. Although Typhidot is superior to Diazo test, the present study shows a reasonable value of sensitivity and specificity for Diazo test. Hence it can be used in resource poor settings as it is economic and easy to perform.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgement
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Garg S, Sankhe A, Joshi A, et al. Comparison of typhidot IgM test and blood culture in children with clinically compatible enteric fever. Int J Contem Pediatr 2018; 5:2129-32.
- Park K, Park K. Text book of preventive and social medicine, m/s. epidemiology of chronic non-communicable diseases and conditions. 23rd Edn. Jabalpur. M/s Banarsidas Bhanot Publishers 2015; 372-400.
- Muthaiyan J, Moomin MR, Varadarajan P, et al. A comparative study of typhidot test and widal test with the culture- positive typhoid fever in children. Cough 2016; 15:57-7.
- Dutta S, Sur D, Manna B, et al. Evaluation of new-generation serologic tests for the diagnosis of typhoid fever: Data from a community-based surveillance in Calcutta, India. Diagnostic Microb Infectious Dis 2006; 56:359-65.
- Pastoor R, Hatta M, Abdoel TH, et al. Simple, rapid, and affordable point-of-care test for the serodiagnosis of typhoid fever. Diagnost Microbiol Infectious Dis 2008; 61:129-34.
- Sherwal BL, Dhamija RK, Randhawa VS, et al. A comparative study of typhidot M and widal test in patients of typhoid fever. J Indian Academy Clin Med 2004; 5.
- Shivpuri D, Dayal HS, Jain D. Table I diazo test in typhoid fever. Indian Pediatr 2003; 40:270-1.
- Kliegman RM, Behrman RE, Jenson HB, et al. Nelson textbook of pediatrics e-book. Elsevier Health Sciences 2007.
- World Health Organization. Typhoid vaccines: WHO position paper, March 2018–Recommendations. Vaccine 2019; 37:214-6.
- John J, Van Aart CJ, Grassly NC. The burden of typhoid and paratyphoid in India: systematic review and meta-analysis. PLoS Neglected Tropical Dis 2016; 10:e0004616.
- Collier LB, Sussman M. Topley & Wilson's microbiology and microbial infections.
- http://www.jiacm.in/pdf/Journal%2065%20Jan%20to%20March%202017.pdf
- Mandell GL, Bennett JE, Dolin R. Principles and practice of Infectious diseases. Text book. 2005; 147:1913-9.
- Turkington C, Ashby B. Encyclopedia of infectious diseases, fact on file, 1998.
- Papagrigorakis MJ, Synodinos PN, Yapijakis C. Ancient typhoid epidemic reveals possible ancestral strain of Salmonella enterica serovar Typhi. Infection Genetics Evolution 2007; 7:126-7.
- https://www.moscmm.org/pdf/Ananthanarayan%20microbio.pdf
- Padmaja N, Nageswara Rao P. Microbiological study of corneal ulcers at kims, Amalapuram. Med Mycol Occulomylosis 2005; 3:4525-4528.
- Koneman EW, Allen SD, Janda WM, et al. Diagnostic microbiology. The nonfermentative gram-negative bacilli. Philedelphia: Lippincott-Raven Publishers. 1997; 253-320.
- World Health Organization. Background document: The diagnosis, treatment and prevention of typhoid fever.
- https://www.worldcat.org/title/mackie-mccartney-practical-medical-microbiology/oclc/35714221
- http://www.academia.edu/6197409/A_Harcourt_Health_Sciences_Company
- Ram PK, Naheed A, Brooks WA, et al. Risk factors for typhoid fever in a slum in Dhaka, Bangladesh. Epidemiol Infection 2007; 135:458-65.
- Kumar V, Abbas AK, Fausto NR, et al. Cotran pathologic basis of disease. 7th Edn. St. Louis, MO: WB Saunders. 2005.
- Surendranath M. Typhoid fever-current scenario. Indian J Practical Pediatr 2019; 21:95.
Author Info
S Sundari*, M Shafath Ahmed and Pooja Pradeep
Department of Paediatrics, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Pooja Pradeep, M Shafath Ahmed, S Sundari, A Comparative Study of Typhidot and Diazo Test in Early Detection and Diagnosis of Typhoid Fever in Children, J Res Med Dent Sci, 2021, 9(6): 278-285.
Received: 30-Mar-2021 Accepted: 23-Jun-2021