Case Report - (2022) Volume 10, Issue 11
A Case of Post Traumatic D10-D11 and L1-L2 Wedge Compression Fracture with Spondylodiscitis of D11
Pratik Mahapatra, Vijay Narasimman Reddy* and Mervinrosario
*Correspondence: Dr. Vijay Narasimman Reddy, Department of Orthopaedics, Sree Balaji Medical College, Chromepet, Chennai, Tamilnadu, India, Email:
Abstract
Introduction: Thoraco lumbar fractures occur as a result of motor vehicle trauma or fall from a height, with the remainder caused by athletic participation and assault. Neurological injury complicates the fractures at the thoracic lumbar level. Case report: A 68-year-old male was brought to the hospital by his family members with complains of low back ache with pain radiating to the back of lower limb. There was a history of fall from bus 2 months back. X-ray and MRI co-relation confirmed D10-D11 and L1-L2 wedge compression with spondylodiscitis of D11. He was managed with posterior stabilisation at D8, D9, D10, D12, L2, L3 with laminectomy at D11 and discectomy at D10-D11 disc.
Conclusion: Thoraco lumbar vertebral fracture has the best outcome when surgical management is the management modality.
Keywords
Thoraco lumbar vertebral, Neurological, Spondylodiscitis
Introduction
Injuries of the thoracolumbar spine occur in between T11 to L2 between upper and middle thoracic column and lumbar spine [1-5]. The upper 3/4th is protected by ribcage and mostly the fractures are stable. However due to the narrow spinal canal cord damage is too common. The spinal cord ends at L1 and below that level it is the lower nerve roots that are at risk. The common mechanisms of injury are compression, rotation/ translation and distraction [6].
Case Presentation
A 68-year-old male was brought to the hospital by his family members with complains of low back ache with pain radiating to the back of lower limb. There was a history of fall from bus 2 months back after which his pain in lower back kept on increasing and became more severe 2 weeks before coming to the hospital. The patient was conscious and oriented with no history of loss of consciousness or any episode of vomiting. His bowel and bladder habits were normal. His medical surgical, allergic history was unremarkable. There was no history of fever or weight loss, morning chills etc. Physical examination revealed no loss of sensation. His power of EHL on right and left side was 4/5, HIP (flexion/extension) on each side was 3/5. Knee (flexion/extension) on each side was 4/5. X-ray and MRI were taken and from it wedge compression of D10-D11 and L1-L2 with spondylodiscitis of D11 was concluded. Routine blood investigation was done and patient had elevated TLC and ESR. Broad spectrum antibiotics Cefoperazone+Sulbactam and Amikacin was started to which patient responded well. The patient was explained about the condition, surgical procedure, and prognosis. The patient consented for the surgery. Before the day of surgery patient was asked to be on nil per oral. On the day of surgery patient was shifted to pre OP and after assessment by anaesthetist was shifted to the OT where he was given general anaesthesia. After intubation patient was put in prone position and parts prepared and draped. Through posterior midline approach a 20 cm long incision was made over the spinous process. Skin and subcutaneous tissue cut and retracted. Erector spinae muscles raised from the attachment. Spinous process, transverse process, pedicle, facet joint visualised. Pedicle screw inserted at the level of D8, D9, D10, D12, L2, L3, L4 (intersecting line between the imaginary line drawn through the mid transverse process and the lateral border of the superior facet joint). Screws were then connected using Harrington rods. The transverse connection was placed between the two rods at level of D11. Laminectomy was done at D11 and discectomy done at D10, D11 level. Spinous process of all the respective vertebrae was removed. Thorough wound wash was given. Wound was closed in layers and drain was kept in situ and sterile dressing was done. Post OT patient was shifted to ICU for observation where he was extubated without any complications and was shifted to ward on the same day. Patient received regular antibiotics, analgesics, physical therapy as well as regular dressing was done. On discharge his condition was stable (Figures 1 and 2).
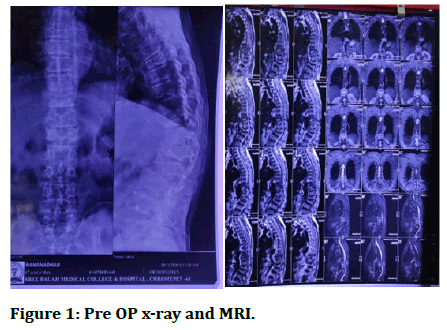
Figure 1: Pre OP x-ray and MRI.
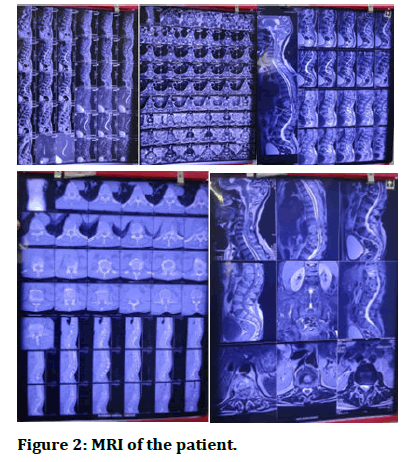
Figure 2: MRI of the patient.
Discussion
Treatment depends on: Type of fracture, neurological involvement, and concomitant injures. In case of minor injuries of fracture of transverse process and that of pars interarticularis if an acute fracture heals properly if patient is prepare to forego sporting activity for several months. Unilateral pars fractures usually go to union with conservative treatment. In patients of flexion injury with minimal wedging and with stable fracture they are kept in bed for 1-2 weeks before mobilizing [7]. Those with 20-40% moderate wedging can be mobilised after a week with patient wearing thoraco lumbar brace with back being in extension. After 3 months repeat x-ray is taken and if no instability is present the brace is discarded gradually. On the other hand, if deformity increases or patient starts to have neurological signs surgery becomes the choice. If the collapse of anterior vertebral height becomes more than 40% it indicates damage of posterior ligament. Patients with fracture with paraplegia patient will need nursing care post-surgery so hospital stay is shortened to fasten the rehabilitation. In fracture dislocation with a partial neurological deficit, there is also no evidence that surgical stabilization and decompression provides a better neurological outcome than conservative treatment [8]. If surgical decompression and stabilization are performed, this may require a combined posterior and anterior approach. In fracture dislocation without neurological deficit, surgical stabilization will prevent future neurological complications and allow earlier rehabilitation [9]. When specialized surgery cannot be performed, these injuries can be managed non-operatively with postural reduction, bed rest and bracing. For patients with neurological impairment who have the benefit of being treated in a specialized spinal injuries unit, a strong case can be made for managing them also by non-operative methods (Figure 3) [10].
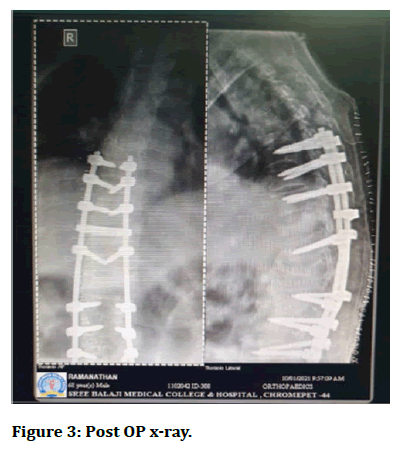
Figure 3: Post OP x-ray.
Conclusion
Management for D10-D11 and L1-L2 wedge compression fracture with spondylodiscitis of D11 in this case was managed through posterior stabilisation at D8, D9, D10, D12, L2, and L3 with laminectomy at D11 and discectomy at D10-D11. Postoperatively, patient’s condition was getting better as shown by increasing motoric power. We can now conclude that the best management for thoraco lumbar fracture with or without comorbid disease is surgery.
References
- Blom A, Warwick D, Whitehouse M. Apley and Solomon’s system of orthopaedics and trauma. 10th Edition, CRC Press. 2018.
- Egol K, Koval KJ, Zuckerman J. Handbook of fractures. 6th Edition, Lippincott Williams and Wilkins, 2019.
- Weinstein SL, Buckwalter JA. Turek’s Orthopaedics: principles and their applications. 6th Edition, Lippincott Williams and Wilkins, 2005.
- Dai LY, Jiang SD, Wang XY, et al. A review of management of thoracolumbar burst fractures. Surg Neurol 2007; 67:221-231.
- Mclain RF, Burkus Jk, Benson DR. Segmental instrumentation for thoracic and thoracolumbar fractures: Prospective analysis of construct survival and five year follow up. Spine J 2001; 1:310-323.
- Aebi M. Classification of thoracolumbar fractures and dislocations. Eur Spine J 2010; 1:S2-S7.
- Mikles MR, Stchur RP, Graziano GP. Posterior instrumentation of thoracolumbar fractures. J Am Acad Orthop Surg 2004; 12:424-435.
- Guven O, Kocaoglu B, Bezer M, et al. The use of screw at the fracture level in the treatment of thoracolumbar burst fractures. J Spinal Disord Tech 2009; 22:417-421.
- Andress HJ, Braun H, Helmberger T, et al. Long term results after posterior fixation of thoraco lumbar burst fractures. Injury 2002; 33:357-365.
- Olerud S, Karlstrom G, Sjostrom L. Transpedicular fixation of thoracolumbar vertebral fractures. Clin Orthop Relat Res 1998; 227:44-51.
Author Info
Pratik Mahapatra, Vijay Narasimman Reddy* and Mervinrosario
Department of Orthopaedics, Sree Balaji Medical College, Chromepet, Chennai, Tamilnadu, IndiaCitation: Pratik Mahapatra, Vijay Narasimman Reddy, Mervinrosario, A Case of Post Traumatic D10-D11 and L1-L2 Wedge Compression Fracture with Spondylodiscitis of D11, J Res Med Dent Sci, 2022, 10 (11): 055-057.
Received: 02-Sep-2022, Manuscript No. JRMDS-22-57339; , Pre QC No. JRMDS-22-57339(PQ); Editor assigned: 06-Sep-2022, Pre QC No. JRMDS-22-57339(PQ); Reviewed: 21-Sep-2022, QC No. JRMDS-22-57339; Revised: 03-Nov-2022, Manuscript No. JRMDS-22-57339(R); Published: 10-Nov-2022
