Review Article - (2022) Volume 10, Issue 7
3D Printing In Dentistry: A Paradigm Shift from Fiction to Reality
Shriya Singi1*, Akash Sibal1 and Aditya Patel2
*Correspondence: Shriya Singi, Department of Dentistry, Datta Meghe Institute of Medical Sciences, Wardha, India, Email:
Abstract
Three-dimensional printing (3D Printing) has been recognized as the pioneer in today’s digital dentistry. Due to the
requirement for customization and personalization of dental products, 3D printing technologies are widely recognised to
enhance dentistry. This review is expected to look into why 3D printing is significant in dentistry, as well as why dentistry
drives research in 3D printing applications. Traditional manufacturing has struggled to make complicated and precise
anatomic models, which 3D printers can now do with ease. The focus of this article is to present a current review of the
various printing techniques, including stereo lithography, selective laser sintering, photopolymer jetting, and powder binder
printers and fused deposition modelling. Furthermore, the implementation of this technology in various fields of dentistry is
given special attention. Dental technology has enhanced diagnostic accuracy, made treatment delivery easier, and
minimized chair time, allowing practitioners to provide more effective treatment. The dentist can use 3D printing to
visualise, record, and create hard and soft tissue models with extreme precision. In a variety of therapy approaches, 3D
printing can be beneficial. It uses the fast developing 3D printing technique to cover research and innovation, therapeutic
methods, teaching, and training. It's a potential clinical tool because it visualises therapy outcomes and offers immense
potential to enhance oral health care. Educational programmes that use 3D-printed models encourage students and
trainees to learn dentistry skills. This study discusses the several 3D printing technologies and its applications in dentistry
Keywords
3D printing, Additive manufacturing, Stereo lithography, Rapid prototyping, Advanced dentistry, Digital dentistry, Advanced printersIntroduction
In the recent years, the medical and health-care industries have witnessed radical transformations. With the rapid growth of technology, the health-care business has evolved its paradigm to provide patients with the safest and least invasive therapeutic approaches. 3D-printing allows the development of custom-made models, prostheses, implants and surgical guides for a variety of uses ranging from patient awareness to prosthetic rehabilitation. Pre-planning, adjusting, and simulating the process is possible because of digital representation of the patient data into a printed format.
The popularity of 3D printing in medical science can be attributable to its cost effectiveness and reduced time consumption when compared to older approaches. It all started in 1983, when Charles Hull used the first 3D printer to print a 3D object for the first time [1].
3D printing is the process of utilising a 3D printer to combine, bind, sinter, or polymerize small volume components to create 3D solid objects from a digital file in the STL format (surface tessellation language file or standard triangulation language file [2]. This article will look at why 3D printing is vital in dentistry, as well as why dentistry drives 3D printing progress.
Literature Review
3D Printing technologies and materials
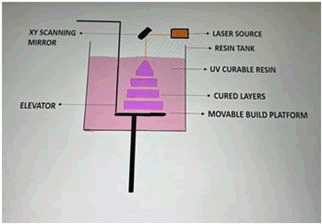
Steriolithography (SLA): In dentistry, Stereo lithography (SLA) is the oldest and most commonly used technology of 3D-printing. In a vat of light-cured photo polymerised resin, a scanning laser is used in stereo lithography equipment to create items one layer at a time. After the laser scans each layer on the liquid resin's surface, a ‘build platform’ drops and once again a coat of material is rubbed over the surface, and the procedure is repeated. Reinforcements are designed in CAD system, printed & then removed from the final product to survive wiping action and gravity. The post-processing step includes removing superfluous resin and hardening it in a UV oven. When utilized for huge things, the procedure is expensive, but it is routinely used in the commercial manufacturing of 3D printed implant drill guides (Figure 1).
Figure 1: Stereolithography.
Advantages: Rapid fabrication can be done using Stereolithographic. Complex shapes with high feature resolution can be created. When used in bulk, the cost of materials is low.
Disadvantages: Only light curable liquid polymers are available. Resin is unsightly, can induce skin sensitization, and can be irritating when touched or inhaled. Vat life and shelf life are both limited. Heat sterilization is also not possible. It is a high-priced technology.
Photopolymer Jetting (PPJ)
An inkjet print unit jets a light-sensitive polymer into a build platform, which is then cured one by one on an incrementally decreasing platform. Using light cured resin materials and print equipment similar to those used in an inkjet printer, this method lays down layers of photopolymer that are cured using light and transferred to the print head (that is more expensive).In a friable substratum, a support structure is placed down. The materials that can be used to print include resins and waxes for casting, and rubber materials like silicon. Complicated geometries and exquisite details are conceivable, having resolution as low as 16 microns [3].
Advantages: It is relatively fast technique. It is feasible to get a high-resolution with a high-quality finish. Multiple materials, including elastic materials, are accessible in a variety of colours and physical qualities. Technology is less expensive.
Disadvantages: It can be tough to completely remove tenacious support material. Heat sterilisation is not possible. Support material may lead to skin irritation. It uses high cost materials.
Powder binder printer
To print, this device employs an advanced inkjet head. One by one, fluid droplets are made to permeate a homogeneous, single layer of powder. A multi-layer final model is finished, and a new fine particle coating is brushed over the area while the powder bed drops incrementally. The infiltrated powder bears the template; therefore, no additional support is essential. During post-processing methods, an epoxy resin or cyanoacrylate is infiltrated into delicate printed models to boost strength and surface hardness. Despite the fact that templates are fragile and have limited precision, they are nonetheless valuable as study models or visual prototypes. This method of generating a full-contour object has shown to be cost-effective.
Advantages: Materials and technology are less expensive. Colour printing is possible. It is comparatively quick process. Also, the materials do not cause any harm.
Disadvantages: The resolution power is insufficient. There is a mess of powder and a lack of strength. It is not possible to soak or heat sterilise this item [4].
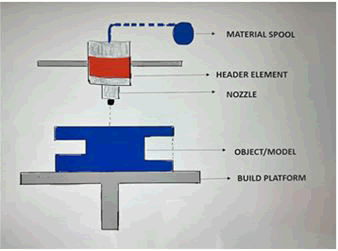
Fused deposition modelling
Schott C Rump developed fused deposition modelling. A temperature-controlled nozzle extrudes a thermoplastic filament material, which hardens almost quickly that is within 1 second. A microprocessor tracks and deposits the material into an incredibly thin layer on a secondary platform by monitoring the nozzle head's movement (Figure 2). Acrylonitrile butadiene styrene ABS, polycarbonates, and poly sulfone are among the materials used. The accuracy of the extruder will be determined by its speed of travel, material flow and the thickness of each 'step.' The majority of low-priced 'home' 3D printers use this method. It enables the creation of simple anatomical models, such as an edentulous jaw, without requiring too much detail [5,6].
Figure 2: Fused deposition modelling.
Advantages: Porosity is high. Mechanical strength is variable. Materials and equipment with a low to mid-price range. Low precision in low-cost equipment is required. Heat sterilisation is an option for some materials.
Disadvantages: It is cost-effective, but only allows for a limited number of materials, such as thermoplastics. For biological materials, shape complexity is limited. Support material must be eliminated.
Selective Laser Sintering (SLS)
The scanning lasers fuse a fine material powder into structures layer after layer as the powder bed descends consecutively, and a fresh small layer of material is evenly dispersed over the surface [7,8]. Because the designs are supported by the adjacent powder, a significant degree of resolution (60 m) can be achieved without the need of any support material. Nylon is one of the most robust and flexible elastomeric materials known, as are metal containing nylon blends.
Advantages: Nylon, elastomers, and composites are among the polymeric materials available. It involves the process that is self-sustaining. Nylon and other polymeric materials can be autoclaved. The mechanical functionality of a printed object may be complete. If used in large quantities, lower-cost materials are available.
Disadvantages: Significant infrastructure, such as compressed air and climate control, is required. Powders are a pain to work with. A risk of inhalation exists. High priced technology. Surface is rough.
Applications of 3D printing in dentistry
Oral and maxillofacial surgery: Maxillofacial along with craniofacial surgeons benefit greatly from 3D imaging and 3D stereo lithography. Maxillofacial reconstruction is typically difficult because of its close proximity, intrinsic complicated architecture and confined access to numerous essential systems such as major veins, nerves, orbit, brain, sinus, and others, as well as its impact on the patient's aesthetics and psychological well-being. Surgeons all over the world praised 3D imaging techniques and stereo lithography models for displaying the "undiscovered dimension" of traditional imaging after its introduction in surgery. Patients may now visualize and comprehend the type and degree of their ailment, as well as the treatment plan and its consequences, and surgeons can now envision the extent of disease, design osteotomies, adjust the equipment’s, and simulate/modify the surgical procedures.
3D models are particularly desirable in today's scenario due to its personalization and high patient compliance, its potential to replicate surgery and osteotomies pre-operatively along with its capacity to foresee the results of the recommended treatment plans. These Three-Dimensional (3D) models are used to teach novice clinicians [9]. How to improvise and practise their surgical skills in order to gain more hands-on experience. Dental implants, maxillofacial prostheses, orthographic operations, Tempera-mandibular Joint surgeries, distraction ontogenesis, orbital reconstructions cancer resections, jaw reconstructions and other professions all use 3D models [10,11].
Using additive manufacturing, fine mesh/lattice structures can be added to the surface of surgical implant to aid Osseo integration. These structures give the implants more strength to tolerate high stresses in key places, such as maxillofacial implants. Metal 3D printing can also be used to make surgical equipment such scalpels, forceps, haemostats, and clamps. Compared to stainless steel, they are less expensive. The craniofacial anatomic models were the first application of computer-aided design & manufacture in field of oral surgery.
3D printing is the optimal instrument for oral surgery education and training since it has so many clinical applications [12]. 3D printing opens up new possibilities in the realm of reproducing or facial anatomies and complicated geometries with extreme precision, which may be used to prepare students and clinicians for a variety of maxillofacial procedures. The enlarged 3D-printed anatomical representations might help students learn 3D spatial orientation and facilitate communication between clinicians and patients.
Orthodontics: Orthodontics is a dental specialty that focuses on the diagnosis and treatment of misaligned teeth and jaws. Recognizing and diagnosing malocclusions, devising treatment plans, assisting in clinical work-ups, and evaluating therapy progress all need accurate presentation of the patient's dental arches and teeth. Previously, plaster models were employed to mimic a patient's dental arches, which was a concern because stone replicas were bulky, time consuming, and much more vulnerable to human error and damages. Furthermore, each patient required multiple sets of replicas to assess their prognosis during treatment, requiring time and space in the dentist's office for storage and handling. Because to the advent of digitization and 3D technology, dental casts may now be scanned and 3D models made.
The patient's information is saved in a digitalized format which is used as a template to make the final cast, if necessary [13]. Such 3D printed modules are precise, allowing them to be employed for therapeutic purposes [14]. Traditional orthodontic treatment involves precisely coordinating movement to reposition malposition teeth. It is accomplished while using brackets and metal wires to apply pressure to single tooth or to the complete arch. These have the potential to fail, requiring emergency visits and interfering with proper dental hygiene, leading to lower treatment efficacy. Aligners and night guard are made with greater precision, speed, and efficiency using 3D printing. Clear aligners are the most recent orthodontics trend, and they solve the majority of the difficulties associated with traditional braces [15]. Using 3D software, the orthodontist customizes the treatment plan as well as develops a system to determine the amount of effort needed for every tooth to attain the ideal position. Aligners have been created & delivered to users under the supervision of a clinician. The aligners are clinically undetectable, simple to clean because they are easily removable allowing for thorough mouth cleaning and flossing, require few dental appointments and have shown positive results.
Prosthodontics: Every phase of the prosthetic rehabilitation of teeth and jaws is influenced by 3D technology. Intra-oral scanners allow for the computerised recording of a patient's dental arches using optical impressions, considerably reducing chair time [16]. Dental labs employ digital data to create removable dyes, stone replicas, wax designs, prosthetic designs, laminate try-ins, as well as surgical guides with CAD/CAM equipment. Solitary imaging and the manufacture of digitally enhanced fixed prostheses are possible with intraoral scanners. When digital impressions were compared to traditional impressions, researchers discovered the technologically created dies and temporary restorations had less peripheral and intrinsic inconsistencies [17].
Implant dentistry: Dental implants are immensely popular among physicians and patients because of their high success rate. Because modern dental implants are put endossteally, that is, inside the bone, they are often in close proximity to essential tissues such as blood arteries, nerves, and the maxillary sinus.
The clinician can now use 3D imaging to examine the operating area prior to surgery, assess the proximity of critical structures and design a therapeutic outcome to prevent or alter implant angulations. To minimise chair time and increase patient comfort, virtual surgical planning with 3-D software allow the clinician to design and practise implant procedure prior to surgery, as well as manufacture surgical drill guides, temporary restorations, and other items [18]. In comparison to manual or bespoke manufacture, it also saves time because 3D-printing the necessary parts takes less time. Furthermore, the likelihood of differences and miscalculations during fabrication is reduced, resulting in greater productivity at the chair side and throughout the procedure.
Endodontic: A minimally invasive therapeutic strategy is critical in today's environment. Drill templates are prepared using digitally created patient images and utilised in guided endodontic to get endodontic clearance and direct the drills suitably. Drill guides that have been pre-planned are effective because they are safe and limit the risk of perforation [19]. Auto transplantation is a technique that involves restoring edentulous space by replacing a patient's natural teeth that has been avulsed owing to injury or transferring a tooth from one site within the dental arch to another. The periodontal ligament's vitality, which provides a store for living cells that can renew after the tooth is transplanted in its new position, is critical to the success of the auto transplanted tooth. Preparing the recipient bone bed in the alveolar socket prior to teeth transplants increases the extra oral time of the tooth to be transplanted lowering its viability. We can now use a pre-prepared 3D printed tooth model to prepare the recipient site before the transplanted tooth is extracted [20]. Because the recipient site has already been prepared using its own 3D model and can be transplanted to the site immediately after extraction; the viability of the transplanted tooth is preserved by limiting extra oral exposure time. As a result, we can see that 3D printing in both surgical and non-surgical endodontic has a bright future.
Periodontics: Periodontology is another field of dentistry where 3D printing is being employed, with research focusing on regenerative periodontology and 3D-printed guidelines for aesthetic gingival correction. The periodontal tissue is a multi-component system that includes bone, gingiva, and cemented. For gingivectomy treatments and smile design, patient-specific surgical guidelines are printed and employed. These templates are well-known for their precision, customisation, and accuracy. In the domain of periodontal tissue regeneration and operations, improvements over conventional approaches can be achieved through the use of personalised goods.
3D printed bio-scaffolds are replacing traditional bone grafting techniques. Guided Bone Regeneration (GBR), sinus augmentation, vertical bone augmentation, socket preservation, and Guided Tissue Regeneration (GTR) are just a few of the periodontal and alveolar regenerative procedures that they are used in [21]. The ability to tailor scaffolds to the patient's needs, adequate mechanical strength, good porosity, maintaining a proper template for cell regeneration, a wide range of bio-materials to choose from, biodegradability, and biocompatibility are just a few of the features that make 3D scaffolds an appealing alternative to traditional grafts.
Periodontal examination, scoring, and indexing methods were previously taught to dentistry students using manikins, dental models, or directly on patients Students have regularly encountered difficulties while probing patients for examination, resulting in patient discomfort such as pain and bleeding [22].
As a result, it would be a good idea to print 3D models of periodontal tissues, and anomalies with their particular tissue features to build adequate skill before operating on the patient. Furthermore, additive manufacturing encourages the printing of models of patients with gingival aesthetic problems, which can then be utilised to train and prevent procedural errors [23].
Paediatric dentistry: In a developing child with mixed dentition, premature tooth loss causes a loss in dental arch length, causing the child to have misaligned teeth. As a solution, dentists frequently recommend space-maintainers to maintain the current arch length while avoiding the necessity for future corrective orthodontic therapy. Construction of space maintainers is usually a time-consuming operation that entails putting together several components into a single device.
Because of low patient conformity in the child population, the lifespan of these space maintainers is sometimes questioned. Studies have discovered successful application of a three dimensionally printed Band and loop space maintainers [24]. 3D printed space maintainers have the advantages of being configurable, being able to be created in single parts, and eliminating the needs for lengthy laboratory and chair-side delays. The Three-Dimensionally printed space maintainer is dependable since they do not require each component soldering, reducing the danger of breakage.
Discussion
Three-dimensional (3D) printing is a rapidly developing technology that has gained worldwide acceptance in dentistry. There are various emerging technologies and materials available to aid the 3D printing process. Dentistry is widely acknowledged to benefit from these technologies due to its need to customize and personalize dental products. In dentistry, 3D printing already has diverse applicability and holds a great deal of promise to make possible many new and exciting treatments and approaches to manufacturing dental restorations.
As stated above, we have seen various applications and the scope of this technology in different fields of dentistry highlighting its huge impact on healthcare. A review of literature done by Liwei Lin et al. discussed 3D imaging technologies and the recent advances in 3D digital processing techniques in dentistry in an effort to give a new perspective and greater understanding of the current development of 3D printing technologies in dentistry.
However, along with this new technology comes new opportunity; the challenge that we face is to not look at 3D printing as a new tool to do what we have always done but to look at it as a technology that will allow us to be more creative, to develop new materials which are more predictable, less invasive and less costly. Overall, 3D printing-based technologies have a tremendous potential to transform treatment methodology, research, and educational streams of dentistry ameliorating oral health care.
Conclusion
3D Printing is revolutionizing digital dentistry by expanding diagnostic, therapeutic, and educational possibilities. The industry's faster research and optimism would provide more avenues to assist in the revolutionization of digital dentistry. In the discipline of dentistry, several technologies have been used for a variety of reasons. All elements of dental field are being influenced by 3D imaging and modelling, as well as CAD/CAM technologies. 3D printing involves precise creation of one-of-a-kind, complicated geometrical forms from digitalized information into a range of substances, either locally or in commercial centres. A 3D printer can currently manufacture practically everything we make for our patients. However, no single technology can meet all of their needs.
While deciding on the best printing technique, take into account the material's medical properties, the amount of time required, and the print product's desired resolution. Although 3D printers are becoming more affordable, the cost of operation, maintenance, materials and the requirement for qualified operators, as well as the necessity for post-processing and compliance to rigorous health and safety regulations, must all be carefully considered. Despite these reservations, 3D printing will undoubtedly play a significant role in dental care in the future. The convergence of scanners, milling, simulation, CAD and 3D printing technology, as well as dentistry's innate enthusiasm and originality, make this an incredible experience to be in the field.
References
- Zaharia C, Gabor AG, Gavrilovici A, et al. Digital dentistry-3D printing applications. J Interdiscip Med 2017; 2:50-53.
- Mahamood S, Khader MA, Ali H. Applications of 3-D printing in orthodontics: a review. Int J Sci Study 2016; 3:267-270.
- Ibrahim D, Broilo TL, Heitz C, et al. Dimensional error of selective laser sintering, three-dimensional printing and PolyJetâ?¢ models in the reproduction of mandibular anatomy. J Craniomaxillofac Surg 2001; 37:167-173.
- Dawood A, Marti BM, Sauret-Jackson V, et al. 3D printing in dentistry. Br Dent J 2015; 219:521-529.
- Van Noort R. The future of dental devices is digital. Dent Mater 2012;28:3-12.
- Subburaj K, Nair C, Rajesh S, et al. Rapid development of auricular prosthesis using CAD and rapid prototyping technologies. Int J Oral Maxillofac Surg 2007; 36:938-943.
- Deckard C, Beaman JJ. Process and control issues in selective laser sintering. ASME Prod Eng Div (Publication) PED 1988; 33:191-197.
- Kruth JP, Vandenbroucke B, Van Vaerenbergh J, et al. Benchmarking of different SLS/SLM processes as rapid manufacturing techniques. InProceedings of the International Conference Polymers and Moulds Innovations PMI 2005.
- Reddy GV, Alwala A. Training young maxillofacial surgeons or trainees using additive manufacturing. Materials Today: Proceedings. 2018; 5:4046-4049.
- Alwala AM, Arvind UD, Malyala SK, et al. Customization of patient specific distraction device using additive manufacture technology. Materials Today: Proceedings. 2018; 5:4134-4147.
- Malyala SK, Kumar YR, Alwala AM, et al. Benefits of additive manufacturing medical model in orbital floor reconstruction surgery: a case study. J Surg 2017; 13:77-79.
- Werz SM, Zeichner SJ, Berg BI, et al. 3D printed surgical simulation models as educational tool by maxillofacial surgeons. Eur J Dent Educ 2018; 22:500-505.
- Kasparova M, Grafova L, Dvorak P, et al. Possibility of reconstruction of dental plaster cast from 3D digital study models. Biomed Eng Online 2011; 12:1-1.
- Leifert MF, Leifert MM, Efstratiadis SS, et al. Comparison of space analysis evaluations with digital models and plaster dental casts. Am J Orthod Dentofacial Orthop 2009; 136:16-21.
- Jawahar A, Maragathavalli G. Applications of 3D printing in dentistryâ??a review. J Pharma Sci Res 2019; 11:1670-1675.
- Christensen GJ. Impressions are changing: deciding on conventional, digital or digital plus in-office milling. J Am Dent Assoc 2009; 140:1301-1304.
- Chochlidakis KM, Papaspyridakos P, Geminiani A, et al. Digital versus conventional impressions for fixed prosthodontics: A systematic review and meta-analysis. J Prosthet Dent 2016; 116:184-190.
- Vasamsetty P, Pss T, Kukkala D, et al. 3D printing in dentistryâ??Exploring the new horizons. Materials Today: Proceedings 2020; 26:838-841.
- Anderson J, Wealleans J, Ray J. Endodontic applications of 3D printing. Int Endod J 2018; 51:1005-1018.
- Lee SJ, Kim E. Minimizing the extra-oral time in autogeneous tooth transplantation: use of Computer-Aided Rapid Prototyping (CARP) as a duplicate model tooth. Restorative dentistry endod 2012; 37:136-141.
- Asaad F, Pagni G, Pilipchuk SP, et al. 3D-printed scaffolds and biomaterials: review of alveolar bone augmentation and periodontal regeneration applications. Int J Dent 2016.
- Heym R, Krause S, Hennessen T, et al. A new model for training in periodontal examinations using manikins. J Dent Educ 2016; 80:1422-1429.
- Li Z, Liu YS, Ye HQ, et al. Diagnossis and treatment of complicated anterior teeth esthetic defects by combination of whole-process digital esthetic rehabilitation with periodontic surgery. Beijing da xue xue bao. Yi xue ban J Pek UniHealth Sci 2017; 49:71-75.
- Pawar BA. Maintenance of space by innovative three-dimensional-printed band and loop space maintainer. J Indian Soc Pedod Prev Dent 2019; 37:205.
Author Info
Shriya Singi1*, Akash Sibal1 and Aditya Patel2
1Department of Dentistry, Datta Meghe Institute of Medical Sciences, Wardha, India2Department of Conservative Dentistry and Endodontics, Datta Meghe Institute of Medical Sciences, War, India
Received: 09-May-2022, Manuscript No. JRMDS-22-P-49975; , Pre QC No. JRMDS-22-P-49975; Editor assigned: 11-May-2022, Pre QC No. JRMDS-22-P-49975; Reviewed: 25-May-2022, QC No. JRMDS-22-P-49975; Revised: 09-Jul-2022, Manuscript No. JRMDS-22-P-49975; Published: 20-Jul-2022