Research Article - (2024) Volume 12, Issue 6
*Correspondence: Avleen Kaur, Department of Ophthalmology, India, Email:
Abstract
Introduction: Cataract is a gradually progressive disease of the eye which is defined as the clouding of the normally clear lens or its capsule. It is a significant cause of blindness around the world which requires removal of cataract by surgical means. The results of cataract surgery can be significantly impacted by the presence of a variety of preoperative systemic disorders. In India, age-related cataracts that require surgery are increasingly prevalent, and non-communicable diseases (NCDs) like diabetes mellitus, hypertension, and heart problems are becoming more and more common. Aim: To determine the pattern of systemic comorbidities and study the sociodemographic characteristics in patients presenting with cataract. Material and methods: This prospective, hospital based, observational study was conducted in the eye OPD OF Department of Ophthalmology, Government Medical College Jammu over a period of 1 year from November 2021 to October 2022. A total of 500 patients were included in the study. Data was collected using a structured proforma and analysed using SPSS inc. v.16. Results: The present study found that the most common affected age group to be 61 to 70 years with females (53.6%) preponderance. The majorities (62.2%) of participants were from rural area and hypertension was the most common associated systemic comorbidity in our study patients (10.6%). Conclusion: It is essential to properly manage and evaluate systemic comorbidities prior to cataract surgery in order to prevent any pre-operative, intra operative or post-operative visual outcomes in such patients. Adequate measures should be undertaken wherever possible in order to enhance visual results.
Introduction
Cataract is a gradually progressive disease of the eye which is defined as the clouding of the normally clear lens or its capsule. It is a significant cause of blindness around the world which requires removal of cataract by surgical means [1]. Presence of various preoperative systemic diseases can have a significant effect on the outcomes of cataract surgery [2]. Age-related cataracts that require surgery are very common in India, and the frequency of Non-Communicable Diseases (NCDs) such diabetes mellitus, hypertension, and heart condition is raising quickly [3]. The increasing prevalence of neurodegenerative disorders, diabetes mellitus, hypertension, cardiovascular pathologies and osteoarticular processes has a great impact on the society. In order to appropriately manage eye disorders, it is pivotal to achieve an early and accurate diagnosis of systemic diseases. This type of integrated approach is essential to prevent blindness and comorbidities [4]. The previously available data showed that diabetic patients who underwent cataract surgery resulted in increased central macular thickness but decreased choroidal thickness due to choroidal metabolic suppression and resulting in decrease in sub foveal choroidal thickness leading to vision impairments [5]. As well as various studies have shown that the increased levels of different systemic inflammatory markers including IL-6, TNF-alpha and C-reactive protein in patients with hypertension, which are believed to promote formation of cataract [6].
Materials and Methods
This prospective, hospital based, observational study was conducted in the eye OPD of Department of Ophthalmology, Government Medical College Jammu over a period of 1 year from November 2021 to October 2022 after due approval from Institutional Ethics Committee of GMC, Jammu vide letter no. IEC/GMC/2022/959. A total of 500 patients presenting with cataract and having systemic co-morbidities were included in the study after obtaining the informed consent. A detailed history was taken and a thorough systemic and ocular examination was done for all patients which included visual acuity analysis using Snellen’s visual acuity chart, intraocular pressure measurement using non-contact tonometer, slit lamp examination to evaluate anterior segment and grade the cataract, fundus examination using a 90-D non-contact slit lamp bio microscopy, indirect ophthalmoscopy on a fully dilated pupil and a USG B-Scan in patients where fundus could not be visualised due to hazy media. The data was collected using a structured proforma, recorded in Microsoft Excel sheet and the statistical analysis was done using SPSS inc. v.16.
Results and Observations
In our study the most common affected age group was 61 to 70 years (Table 1) with female (53.6%) preponderance (Figure 1).
| AGE GROUP (YEARS) | NUMBER(N) | PERCENTAGE (%) |
|---|---|---|
| Up to 50 years | 11 | 2.2 |
| 51-60 years | 116 | 23.2 |
| 61-70 years | 195 | 39 |
| 71-80 years | 133 | 26.6 |
| 81-90 years | 44 | 8.8 |
| >90 years | 1 | 0.2 |
Table 1: Age distribution of patients (N=500)
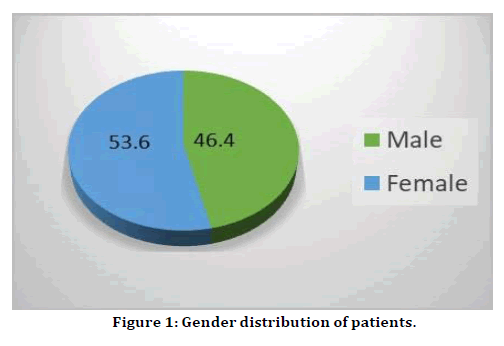
Figure 1. Gender distribution of patients.
Our study found that the most common type of cataract was nuclear sclerosis grade II (NS II) seen in 27.1% of patients (Table 2).
| Ocular comorbidities | Right eye | Left eye | ||
|---|---|---|---|---|
| No. | % | No. | % | |
| NS grade I | 22 | 4.4 | 21 | 4.2 |
| NS grade II | 149 | 29.8 | 122 | 24.4 |
| NS grade III | 59 | 11.8 | 79 | 15.8 |
| NS grade IV | 1 | 0.2 | 6 | 1.2 |
| CC | 30 | 6 | 33 | 6.6 |
| PSC | 40 | 8 | 57 | 11.4 |
| MSC | 115 | 23 | 107 | 21.4 |
| PPC | 10 | 2 | 7 | 1.4 |
| ASC | 1 | 0.2 | 68 | 13.6 |
| None | 73 | 14.6 | 21 | 4.2 |
Table 2: Grade of cataract patients
It was found that majority (62.2%) of participants were from rural area in our study (Figure 2).
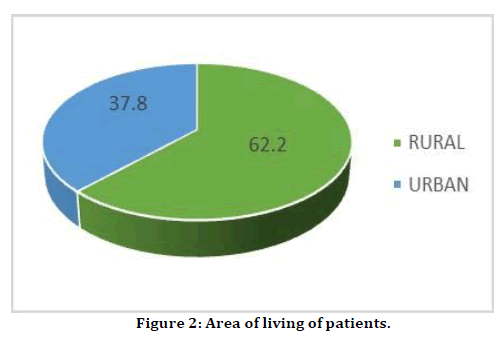
Figure 2. Area of living of patients.
Our study showed that (64%) participants reported no systemic co morbidity and hypertension was the most common systemic comorbidity reported in 10.6% of study participants (Table 3).
| SYSTEMIC CO MORBIDITY | NUMBER | % |
|---|---|---|
| None | 320 | 64 |
| Hypertension | 53 | 10.6 |
| Multiple comorbidities | 51 | 10.2 |
| Type 2 DM | 46 | 9.2 |
| Heart Disease | 8 | 1.6 |
| Rheumatoid Arthritis | 7 | 1.4 |
| Bronchial Asthma | 4 | 0.8 |
| Thyroid disorder | 10 | 2 |
| Chronic Kidney disease | 1 | 0.2 |
Table 3: Associated Systemic Comorbidities in cataract patients
In our study most study participants were in the age group of 61 to 70 years with female preponderance. The majority (62.2%) of participants were from rural area. These findings are consistent with previous studies [7-11]. The most common type of cataract was nuclear sclerosis grade II seen in 27.1% of patients [12]. The present study concluded that hypertension was the most common systemic comorbidity reported among cataract patients [13]. This study has limitations as it included only the patients attending Eye OPD. We need more such studies on a bigger scale with varied population and sample size to determine the pattern of systemic comorbidities in patients presenting with cataract.
Conclusion
This study concludes that it is essential to properly manage and evaluate systemic comorbidities prior to cataract surgery in order to prevent any pre-operative, intra operative or post-operative visual outcomes in such patients. Adequate measures should be undertaken wherever possible in order to enhance visual results.
References
- Vajpayee RB, Joshi S, Saxena R, et al. Epidemiology of cataract in India: combating plans and strategies. Ophthalmic Res. 1999; 31:86-92.
- Willerscheidt AB, Healey ML, Ireland M. Cataract surgery outcomes: importance of co-morbidities in case mix. JCRS. 1995; 21:177-81.
- Sathyan P, Sathyan P. A three year analysis of systemic comorbidities in cataract operated patients in India. JCDR. 2017; 11:NL03.
- Pinazo-Durán MD, Arévalo JF, García-Medina JJ, et al. Ocular Comorbidities and the relationship between eye diseases and systemic disorders. Biomed Res Int. 2016.
- Torabi H, Sadraei M, Jadidi K, et al. Choroidal thickness changes following cataract surgery in patients with type 2 diabetes mellitus. J Curr Ophthalmol. 2019; 31:49-54.
- Bautista LE, Vera LM, Arenas IA, et al. Independent association between inflammatory markers (C-reactive protein, interleukin-6, and TNF-α) and essential hypertension. J Hum Hypertens. 2005; 19:149-54.
- Mahajan S, Raina B, Gupta SK. Epidemiological profile of patients undergoing cataract surgery in a tertiary eye care centre. JK Science: J Med Educ 2021; 23:98-101.
- Shori C, Shori R, Laxmiprasad G, et al. A study of clinical and ophthalmologic profile of patients undergoing cataract surgery. Med Sci 2017; 5:2229-32.
- Aarthi R, Roy G, Kar SS, Srinivasan R. Prevalence of cataract among adults above 50 years in a rural community of Villupuram, Tamil Nadu. Int j adv med health res. 2015; 2:50-4.
- Nirmalan PK, Thulasiraj RD, Maneksha V, et al. A population based eye survey of older adults in Tirunelveli district of south India: blindness, cataract surgery, and visual outcomes. Br J Ophthalmol. 2002; 86:505-12.
- Raina B, Sharma P. The study of the demographic profile of patients of senile mature cataract attending the eye OPD of GMC Jammu, India. IJRMS. 2020; 8:833-5.
- Erşekerci TK, Kurt A, Kılıç R, et al. Demographic characteristics and comorbidity profiles in patients with senile cataract. Int J Ophthalmol. 2018; 9:1-7.
- Pham TQ, Wang JJ, Rochtchina E, et al. Systemic and ocular comorbidity of cataract surgical patients in a western Sydney public hospital. Clin Exp Ophthalmol. 2004; 32:383-7.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
